All published articles of this journal are available on ScienceDirect.
Identifying Barriers and Enablers to Vaccine uptake from Immunizers and Individuals Receiving a COVID-19 Vaccine in Saskatchewan
Abstract
Background:
Vaccine hesitancy presents a challenge to public health, especially during a global pandemic. Understanding reasons for vaccine hesitancy in local populations may help policymakers and public health practitioners increase vaccine uptake.
Objective:
We surveyed individuals receiving a COVID-19 vaccine and immunizers in Saskatchewan, Canada and categorized their responses according to the Theoretical Domains Framework. This provides policymakers with evidence-based suggestions for behaviour change interventions that may promote vaccine uptake among hesitant individuals.
Methods:
Two online surveys were developed to better understand vaccine hesitancy in Saskatchewan: one aimed at individuals receiving a vaccination and the other at immunizers. Both surveys were available for a one-week period when vaccination uptake had plateaued in Saskatchewan. Individuals receiving a vaccine were asked what made them decide to get a vaccine, and both groups were asked what they thought would promote vaccine uptake among hesitant individuals. Responses were analyzed thematically based on the Theoretical Domains Framework and reported descriptively.
Results:
Individuals receiving a COVID-19 vaccine indicated that mandates and restrictions and having a positive attitude toward COVID-19 vaccines were the most common reasons for receiving a vaccine. Immunizers most frequently indicated that media issues led to vaccine hesitancy and that having access to, and trust in, reputable information sources would enable more vaccine hesitant individuals to seek a COVID-19 vaccination.
Conclusion:
Mandates and restrictions, promoting positive attitudes towards vaccines, and ensuring people have access to, and trust in, reputable information sources, are key enablers for promoting vaccine uptake among vaccine hesitant individuals.
1. INTRODUCTION
Vaccine hesitancy, defined as a delay in acceptance or refusal of vaccination despite the availability of vaccination services [1], has been a factor inhibiting the uptake of COVID-19 vaccines and a challenge to public health in Canada [2]. As of August 28, 2021, Saskatchewan had the lowest COVID-19 vaccine uptake [58.3% of the total population fully vaccinated] among all provinces in Canada [66.8% nationally] [3]. Although vaccine hesitancy is not a new phenomenon, we still lack sufficient evidence to inform the effectiveness of strategies to address this issue, particularly in the context of COVID-19 vaccines [4]. With respect to COVID-19 vaccine hesitancy specifically, research by Muhajarine et al. provides insights into factors related to vaccine acceptance in Saskatchewan; for example, people who more often wear masks are more likely to accept a vaccination [5]. Researchers have also indicated that perception of COVID-19 as a threatening disease and negative attitudes or general mistrust towards vaccines are factors that may affect vaccine uptake [5-7]. From a broader population approach, Crawshaw et al. [8] recently initiated a living behavioural science evidence synthesis on COVID-19 vaccination uptake among the general public, outlining a number of barriers and facilitators to vaccination compiled from international studies. In all of these instances, while the authors are able to provide information about the types of interventions that may increase vaccine uptake, there is limited information about how effective these strategies are in practice, particularly in different local contexts where a number of factors may differ from published research.
One benefit to the approach of Crawshaw et al. [8] is their use of a behavioural framework to contextualize their results in terms of behaviour change efforts and provide direction for policymakers when implementing changes. Their review uses the COM-B model of behaviour [Capability + Opportunity + Motivation = Behaviour] [9] and the Theoretical Domains Framework (TDF) [10] to categorize their findings into various barriers and enablers of vaccine uptake based on behavioural science. The COM-B model describes any behaviour as a function of an individual’s capability, opportunity, and motivation to perform that behaviour [9]. The TDF expands upon these three categories to include 14 theoretical domains that can inform implementation interventions based on multiple behavioural theories [10]. For example, in their review, Crawshaw et al. [8] identified gaps in knowledge about COVID-19 vaccines as a common barrier to vaccine uptake. This barrier was mapped to the knowledge domain within the TDF and represents a barrier to an individual’s capability (COM-B) to perform the behaviour (i.e., seek a vaccination).
Given the paucity of evidence regarding which interventions are most effective at promoting vaccine uptake among hesitant individuals, as part of a larger developmental evaluation of Saskatchewan’s vaccine rollout program, we set out to determine what was motivating individuals to seek a COVID-19 vaccine in Saskatchewan. We also asked both immunizers and individuals receiving a vaccine what they thought would motivate vaccine hesitant individuals to seek a COVID-19 vaccine. We used the framework developed by Crawshaw et al. [8] to present local data in a similar context, in an effort to provide policymakers with locally-relevant, evidence-based information on which behaviour change efforts may be most effective in promoting vaccine uptake. The information from our surveys may also be relevant to other jurisdictions throughout Canada and globally.
2. MATERIALS AND METHODS
2.1. Setting
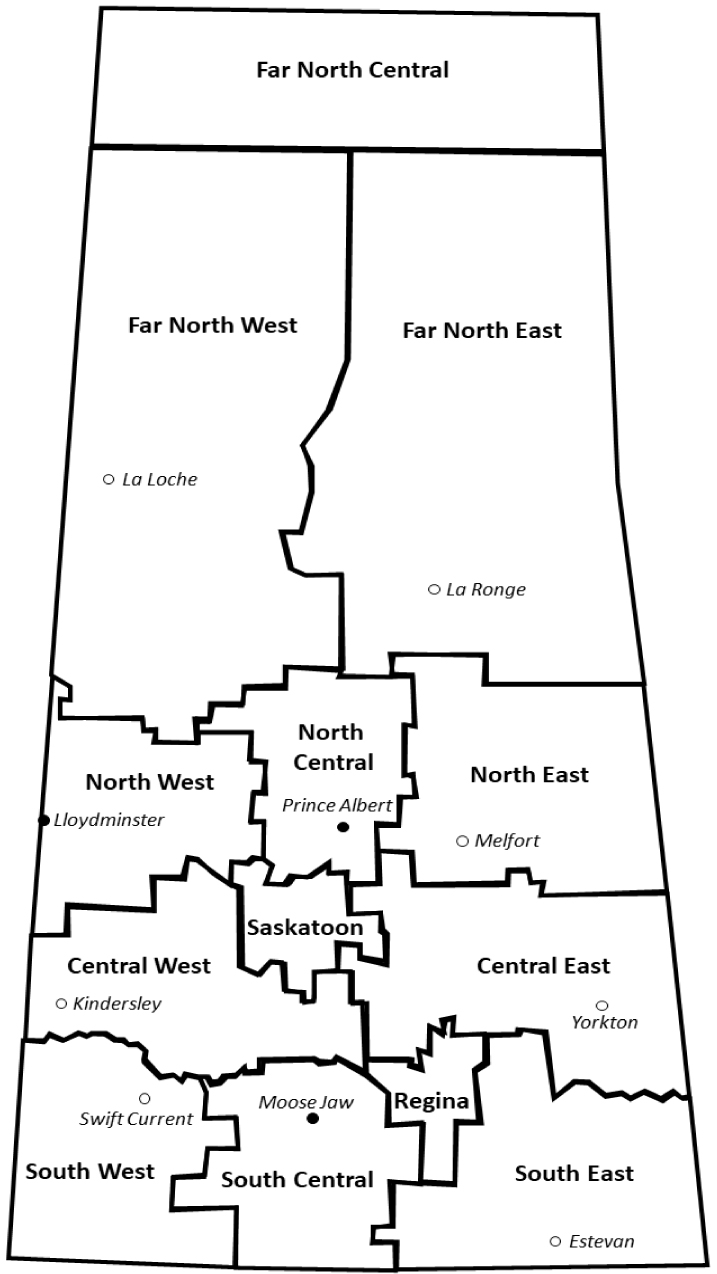
Saskatchewan is a Canadian province of ~1.17 million people [11] spread over more than 650,000 km2. Approximately 40% of the population resides in two large urban centres (Regina and Saskatoon), another 8% in three medium-sized urban centres (Prince Albert, Moose Jaw, and Lloydminster), and the remaining 52% reside in small urban centres and rural locations spread throughout the province [12].
For the COVID-19 vaccine rollout, the provincial Saskatchewan Health Authority (SHA) divided the province into 13 geographic regions (Fig 1). Vaccine rollout has been primarily under the jurisdiction of the SHA, in collaboration with the Saskatchewan Government Ministry of Health. Following an initial pilot phase, vaccine eligibility was primarily based on age, beginning with the eldest and decreasing in age as vaccine supply became available. As of May 20, 2021, anyone ≥12 years old was eligible to receive a COVID-19 vaccine [13]. Initially, mass vaccination and drive-through clinics were set up throughout the province to meet the demand for early uptake; personal care homes and long-term care facilities were also targeted early to vaccinate those higher-risk populations. By April 29, 2021, private pharmacies were also providing supplemental vaccine delivery [14]. As the summer progressed and vaccine uptake waned, mass clinics were closed and the vaccine delivery strategy transitioned to pop-up clinics in locations and at events throughout the province.
During the week prior to survey distribution, provincial policy changed allowing individuals who had a mixed vaccine regimen e.g., an mRNA-based vaccine and a viral vector-based vaccine to obtain a third dose to meet travel requirements e.g., to travel to countries that required two doses of a single vaccine [15]. Additionally, children who were born in 2009 but were not yet 12 years of age were also permitted to receive a vaccine [16].
2.2. Surveys
We developed two electronic surveys using the Research Electronic Database Capture tool REDCap [17, 18] to collect information from two sources: individuals who were receiving a vaccine and immunizers. Due to the short time period in which the surveys were required to be developed and disseminated, rigorous validity and reliability assessments were not performed. However, face validity was established as multiple stakeholders in the COVID-19 vaccination rollout were included in survey development, including researchers, SHA administrative leadership, clinicians, and other experts involved in organizing and administering vaccine clinics across the province. This helped to ensure that survey questions were being interpreted reliably and were providing valid answers. Data were collected between August 24 and September 1, 2021.
For individuals receiving a vaccine, staff at the clinic invited them to either fill out a paper survey or access the electronic survey using their smartphone [or other device] while they waited during their 15 minute recovery period. Paper surveys were subsequently scanned and emailed to the study team for data entry using the electronic survey. For this group, demographic information was collected relating to age, gender, geographic location, and which dose of vaccine they had just received. Two open-ended questions were posed: 1 What made you decide to get a COVID-19 vaccine today? and 2 What do you think would get people who haven’t been vaccinated to get a COVID-19 vaccination?
Immunizers were invited to participate in the electronic survey via an email that was sent to ~1200 SHA employees who had worked at least one shift as an immunizer in the three months prior to the survey start date. Immunizers were asked to identify the geographic region in which they worked and were posed two open-ended questions: 1 What do you think is needed to get vaccine hesitant individuals to get a COVID-19 vaccination? and 2 Please provide up to three reasons why, in your experience, vaccine hesitant individuals are not getting a COVID-19 vaccine.
2.3. Data Analysis
Survey data collected in REDCap were exported to Microsoft Excel and analysed by two teams of two coders; one team reviewed responses from individuals receiving the vaccine, and the other reviewed responses from immunizers. When the two coders disagreed on a category for a particular response, a third reviewer made the final decision. Survey responses were coded deductively based on the set of barriers and enablers and their associated COM-B components and TDF domains outlined by Crawshaw et al. [8].
Some questions received more coded responses than the total number of respondents because multiple codes could be assigned to a single answer. For example, if a respondent indicated they were getting vaccinated because they were a teacher and wanted to protect their students and family and to be able to travel, that response would encompass three codes: a belief that COVID-19 vaccines will help protect their family, when getting vaccinated is seen as a professional or collective/prosocial responsibility, and to be able to travel. For survey responses that did not match an existing category, new barriers or enablers were coded and associated with a behaviour component from the COM-B model and a domain within the TDF. For example, we identified fear of losing a job if they are not vaccinated as a new code i.e., not previously identified by Crawshaw et al. [8]. This code was deemed an enabler connected to the emotion domain (TDF) as a motivational aspect of behaviour (COM-B). Results were presented as a descriptive analysis of response proportions.
3. RESULTS
3.1. Individuals Who Received a COVID-19 Vaccine
We received 1012 survey responses from 26,449 individuals (3.8% response rate) who received a COVID-19 vaccine while the survey was available. The response rate was similar among first (262/8001; 3.3%), second (410/11,198; 3.7%) and third dose recipients (322/7250; 4.4%). Demographic data are available in (Table 1). Respondents were categorized into ten-year age categories, starting with <20 years [11-19] through ≥70 years (combined into one category as few respondents were >79 years old).
| Total Respondents (N) | 1012 | Gender | Count (n) | % | |
| Male | 509 | 50.3% | |||
| Age (years) | Female | 488 | 48.2% | ||
| Median | 38 | Other/No Response | 15 | 1.5% | |
| Range | 11-94 | ||||
| Age Category (years) | Count (n) | % | Geographic Region | Count (n) | % |
| <20 | 155 | 15.3% | Saskatoon | 414 | 40.9% |
| 20-29 | 211 | 20.8% | Regina | 165 | 16.3% |
| 30-39 | 161 | 15.9% | North West | 120 | 11.9% |
| 40-49 | 134 | 13.2% | Central East | 80 | 7.9% |
| 50-59 | 176 | 17.4% | Central West | 42 | 4.2% |
| 60-69 | 147 | 14.5% | South East | 41 | 4.1% |
| ≥70 | 17 | 1.7% | North Central | 34 | 3.4% |
| No Response | 11 | 1.1% | Far North East | 26 | 2.6% |
| North East | 16 | 1.6% | |||
| Vaccine Dose | Count (n) | % | South West | 16 | 1.6% |
| First | 262 | 25.9% | South Central | 16 | 1.6% |
| Second | 410 | 40.5% | Far North West | 8 | 0.8% |
| Third | 322 | 31.8% | Far North Central | 1 | 0.1% |
| No Response | 18 | 1.8% | No Response | 33 | 3.3% |
| - | Vaccine Dose | |||||||
| - | First | Second | Third | No Response | ||||
| Age Category | Count [n] | % | Count [n] | % | Count [n] | % | Count [n] | % |
| <20 | 77 | 29.4% | 70 | 17.1% | 4 | 1.2% | 4 | 22.2% |
| 20 - 29 | 74 | 28.2% | 123 | 30.0% | 10 | 3.1% | 4 | 22.2% |
| 30-39 | 44 | 16.8% | 93 | 22.7% | 23 | 7.1% | 1 | 5.6% |
| 40-49 | 37 | 14.1% | 69 | 16.8% | 27 | 8.4% | 1 | 5.6% |
| 50-59 | 16 | 6.1% | 31 | 7.6% | 126 | 39.1% | 3 | 16.7% |
| 60-69 | 5 | 1.9% | 13 | 3.2% | 126 | 39.1% | 3 | 16.7% |
| ≥70 | 3 | 1.1% | 11 | 2.7% | 3 | 0.9% | - | - |
| No Response | 6 | 2.3% | - | - | 3 | 0.9% | 2 | 11.1% |
3.1.1. What made you Decide to get a COVID-19 Vaccine Today?
There were 840 coded responses from answers to the question of why an individual was receiving a vaccine. The top five responses are outlined below, along with whether the response represents an enabler or barrier, the associated component of the COM-B model (i.e., capability, opportunity, or motivation), and the relevant domain from the TDF. The full list of response categories is available in Table 2.
| Barrier/ Enabler | COM-B1 | TDF2 | Theme | Count [n]3 | % |
|---|---|---|---|---|---|
| Enabler | Motivation | Goal | To be able to travel | 307 | 36.5% |
| Enabler | Motivation | Beliefs About Consequences | Positive attitudes/high perceived benefit of COVID-19 vaccines | 139 | 16.5% |
| Enabler | Opportunity | Environmental Context and Resources | Mandates and restrictions (e.g., government, school, work, proof of vaccination for events and public places, etc.) | 91 | 10.8% |
| Enabler | Opportunity | Environmental Context and Resources | Ease of access in terms of time, convenience, and cost | 67 | 8.0% |
| Enabler | Motivation | Social/Professional Role and Identity | When getting vaccinated is seen as a professional or collective/prosocial responsibility | 67 | 8.0% |
| Enabler | Motivation | Beliefs About Consequences | Belief that COVID-19 vaccines will help protect family | 38 | 4.5% |
| Enabler | Opportunity | Social Influences | Pressure or encouragement from family/spouse/government/others | 37 | 4.4% |
| Enabler | Motivation | Beliefs About Consequences | Concerns about becoming infected with COVID-19 | 33 | 3.9% |
| Enabler | Motivation | Goal | Return to normal, attend social events/gatherings | 24 | 2.9% |
| Enabler | Opportunity | Environmental Context and Resources | Having access to and trust in reputable information sources | 11 | 1.3% |
| Enabler | Motivation | Emotion | Fear about being infected with COVID-19 and its impact | 6 | 0.7% |
| Enabler | Opportunity | Social Influences | Advice from medical professionals encouraging vaccination | 6 | 0.7% |
| Enabler | Motivation | Emotion | Fear of losing the job if not vaccinated | 3 | 0.4% |
| Enabler | Motivation | Reinforcement | Members of families/close social networks being infected with COVID-19 | 3 | 0.4% |
| Enabler | Motivation | Emotion | Shame/being ostracized for not being vaccinated | 2 | 0.2% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine safety | 2 | 0.2% |
| Enabler | Motivation | Social/Professional Role and Identity | Certain political preferences/identities | 1 | 0.1% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about adverse reactions [specific contraindications among patients, e.g., patients with rheumatologic diseases] | 1 | 0.1% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine efficacy | 1 | 0.1% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine development | 1 | 0.1% |
2Theoretical Domains Framework
3N=840.
The most common reason for receiving a vaccine was to be able to travel (enabler/motivation/goal; 307/840, 36.5%). This was similar between male and female respondents (130/397, 32.7% and 174/439, 39.6%, respectively) and was the most common response among most age categories, including 20-29 (39/174, 22.4%), 40-49 (30/116, 35.9%), 50-59 (94/144, 70.7%), 60-69 (93/140, 66.4%), and ≥70 (5/10, 50.0%). This was also the most common response among individuals receiving their third dose (222/312, 71.2%) and in 9/13 geographic regions in the province, including Central East, (20/62, 32.3%), Central West (7/22, 31.8%), Far North West (2/7, 28.6%), North East (3/16, 18.8%), North West (27/112, 24.1%), Regina (72/158, 45.6%), Saskatoon (134/325, 41.2%), South Central (6/16, 37.5%), and South East (17/37, 45.9%).
The second most common reason for receiving a vaccine was having a positive attitude toward or high perceived benefits of a COVID-19 vaccine (enabler/motivation/beliefs about consequences; 139/840, 16.5%). This answer was ranked highest among the <20 and 30-39 year old age categories (20/115, 25.2% and 35/149, 23.5%, respectively) and individuals receiving their second dose (86/325, 26.5%). This was also the most common reason in the North East (8/32, 25.0%), North Central (5/23, 21.7%), and South West (4/13, 30.8%) geographical regions.
The third most common reason for receiving a vaccine was due to mandates and restrictions (enabler/opportunity/envi ronmental context and resources; 91/840, 10.8%). This reason was more common among younger age categories (<50 years, 85/91, 93.4%) compared to older age categories (≥50 years, 6/91, 6.6%) and was also the primary reason given by individuals receiving their first dose (59/194, 30.4%). Among the geographic regions, this reason varied from second to fifth most common, and was not noted at all in the three Far North regions and the North East region.
The final two reasons among the top five for receiving a vaccination share equal representation (67/840, 8.0% each). These are ease of access in terms of time, convenience, and cost (enabler/opportunity/environmental context and resources) and when getting vaccinated is seen as a professional or collective/prosocial responsibility (enabler/motivation/social or professional role and identity). Ease of access was the more common reason among male respondents (41/397, 10.3%), while female respondents more often indicated a collective responsibility to get vaccinated (37/439, 8.4%).
3.1.2. What do you think would get people who haven’t been vaccinated to get a COVID-19 vaccination?
There were 699 coded responses from answers to the question of what might promote COVID-19 vaccine uptake among unvaccinated individuals. The top five responses are outlined below and the full list of response categories is available in Table 3.
|
Barrier/ Enabler |
COM-B1 | TDF2 | Theme | Count [n]3 | % |
|---|---|---|---|---|---|
| Enabler | Opportunity | Environmental Context and Resources | Mandates and restrictions [e.g., government, school, work, proof of vaccination for events and public places, etc.] | 213 | 30.5% |
| Enabler | Opportunity | Environmental Context and Resources | Having access to, and trust in, reputable information sources | 157 | 22.5% |
| Barrier | Motivation | Beliefs About Consequences | Beliefs about personal choice/freedom/feeling forced | 70 | 10.0% |
| Enabler | Motivation | Reinforcement | Incentives [e.g., money, prizes, etc.] | 46 | 6.6% |
| Enabler | Motivation | Reinforcement | Members of families/close social network being infected with COVID-19 | 38 | 5.4% |
| Barrier | Opportunity | Environmental Context and Resources | Media issues [e.g., coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation, etc.] | 30 | 4.3% |
| Enabler | Motivation | Beliefs About Consequences | Getting COVID-19 themselves | 27 | 3.9% |
| Enabler | Opportunity | Environmental Context and Resources | Ease of access in terms of time, convenience, and cost | 20 | 2.9% |
| Enabler | Opportunity | Social Influences | Pressure or encouragement from family/spouse/government/others | 17 | 2.4% |
| Enabler | Motivation | Social/Professional Role and Identity | When getting vaccinated seen as a professional or collective/prosocial responsibility | 16 | 2.3% |
| Enabler | Motivation | Goal | Return to normal, attend social events/gatherings | 14 | 2.0% |
| Enabler | Capability | Knowledge | One-on-one, targeted, or small group outreach/education/conversations | 11 | 1.6% |
| Enabler | Motivation | Goal | To be able to travel | 9 | 1.3% |
| Barrier | Opportunity | Social Influences | Mistrust in government/public health response to COVID-19 | 8 | 1.1% |
| Enabler | Opportunity | Social Influences | Advice from medical professionals encouraging vaccination | 4 | 0.6% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine development | 4 | 0.6% |
| Enabler | Motivation | Emotion | Fear about being infected with COVID-19 and its impact | 3 | 0.4% |
| Enabler | Motivation | Beliefs About Consequences | Positive attitudes/high perceived benefit of COVID-19 vaccines | 3 | 0.4% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine safety | 3 | 0.4% |
| Barrier | Capability | Knowledge | Gaps in knowledge about COVID-19 vaccines | 2 | 0.3% |
| Enabler | Motivation | Emotion | Shame/being ostracized for not being vaccinated | 1 | 0.1% |
| Enabler | Motivation | Beliefs About Consequences | Belief that COVID-19 vaccines will help protect family | 1 | 0.1% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine efficacy | 1 | 0.1% |
| Barrier | Opportunity | Social Influences | Negative influence of close contacts and high-profile persons | 1 | 0.1% |
2Theoretical Domains Framework
3N=699.
The most common response to what an individual thought would promote vaccine uptake among unvaccinated individuals was mandates and restrictions (enabler/opportunity/ environmental context and resources; 213/699, 30.5%). This was the top response among both male (104/339, 30.7%) and female (108/351, 30.8%) respondents and all age categories except for 20-29 and ≥70 years. It was also the top response among those receiving first (34/150, 22.7%, tied with below) and third (125/260, 48.1%) doses, but was only the top response in 6/13 geographic regions, including Central East (15/52, 28.8%), Far North East (11/27, 40.7%), North West (17/80, 21.3%, tied with below), Regina (44/128, 34.4%), Saskatoon (100/279, 35.8%), and South West (5/11, 45.5%).
The second most common response to what would promote vaccine uptake among unvaccinated individuals was having access to, and trust in, reputable information sources (enabler/opportunity/environmental context and resources; 157/699, 22.5%). This was the most common response in 6/13 geographic regions, including Central West (8/24, 33.3%), Far North West (2/8, 25.0%), North Central (5/22, 22.7%), North East (5/11, 45.5%), North West (17/80, 21.3%, tied with above), and South East (9/31, 29.0%, tied with below). This was also the top response among 20-29 year olds (39/130, 30.0%) and those ≥70 (4/12, 33.3%), as well as those receiving a first (34/150, 22.7%, tied with above) or second (82/284, 28.9%) dose.
The third most common response to what would promote vaccine uptake among unvaccinated individuals was the only barrier identified among the top five responses: beliefs about personal choice/freedom/feeling forced to get vaccinated (barrier/motivation/beliefs about consequences; 70/699, 10.0%). This was the most common response in the South Central (4/12, 33.3%) and South East (9/31, 29.0%, tied with above) regions and was the second most common response in Central West (4/24, 16.7%). However, it was not among the top five responses in 50-59 and 60-69 year olds.
The fourth most common response to what would promote vaccine uptake among unvaccinated individuals was incentives (e.g., money, prizes, etc.; enabler/motivation/reinforcement; 46/699, 6.6%). This response was ranked higher among individuals <40 years old (32/46, 69.6%) compared to those ≥40 (13/46, 28.3%); one respondent did not provide their age.
The last of the top five most common responses to what would promote vaccine uptake among unvaccinated individuals was having a member of their family or close social network become infected with COVID-19 (enabler/motivation/ reinforcement; 38/699, 5.4%). This was the third most common response in the Regina region (9/128, 7.0%) and was more common among those ≥40 years old (28/38, 73.7%).
Table 4.
|
Barrier/ Enabler |
COM-B1 | TDF2 | Theme | Count [n]3 | % |
|---|---|---|---|---|---|
| Enabler | Opportunity | Environmental Context and Resources | Having access to, and trust in, reputable information sources | 227 | 33.5% |
| Enabler | Opportunity | Environmental Context and Resources | Mandates and restrictions [e.g., government, school, work, proof of vaccination for events and public places, etc.] | 175 | 25.8% |
| Enabler | Opportunity | Environmental Context and Resources | Ease of access in terms of time, convenience, and cost | 69 | 10.2% |
| Barrier | Opportunity | Environmental Context and Resources | Media issues [e.g., coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation, etc.] | 56 | 8.3% |
| Enabler | Motivation | Reinforcement | Incentives [e.g., money, prizes, etc.] | 36 | 5.3% |
| Enabler | Capability | Knowledge | One-on-one, targeted, or small group outreach/education/conversations | 33 | 4.9% |
| Barrier | Motivation | Beliefs About Consequences | Beliefs about personal choice/freedom/feeling forced | 19 | 2.8% |
| Enabler | Opportunity | Social Influences | Pressure or encouragement from family/spouse/government/others | 17 | 2.5% |
| Enabler | Motivation | Reinforcement | Members of families/close social network being infected with COVID-19 | 14 | 2.1% |
| Enabler | Opportunity | Social Influences | Advice from medical professionals encouraging vaccination | 7 | 1.0% |
| Enabler | Motivation | Beliefs About Consequences | Getting COVID-19 themselves | 4 | 0.6% |
| Barrier | Opportunity | Social Influences | Mistrust in government/public health response to COVID-19 | 3 | 0.4% |
| Enabler | Motivation | Beliefs About Consequences | Positive attitudes/high perceived benefit of COVID-19 vaccines | 3 | 0.4% |
| Enabler | Motivation | Goal | Return to normal, attend social events/gatherings | 2 | 0.3% |
| Enabler | Motivation | Goal | To be able to travel | 2 | 0.3% |
| Enabler | Motivation | Social/Professional Role and Identity | When getting vaccinated seen as a professional or collective/prosocial responsibility | 2 | 0.3% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine safety | 2 | 0.3% |
| Barrier | Opportunity | Social Influences | Negative influence of close contacts and high-profile persons | 2 | 0.3% |
| Enabler | Motivation | Emotion | Shame/being ostracized for not being vaccinated | 1 | 0.1% |
| Enabler | Motivation | Emotion | Fear of losing job if not vaccinated | 1 | 0.1% |
| Enabler | Motivation | Beliefs About Consequences | Belief that COVID-19 vaccines will help protect family | 1 | 0.1% |
| Barrier | Opportunity | Social Influences | Direct advice from medical professionals about vaccination | 1 | 0.1% |
2Theoretical Domains Framework
3N=677.
3.2. Immunizers
We received 559 survey responses from ~1200 immunizers who were invited to participate (~47% response rate). Most responses were collected in the two large urban areas, Saskatoon (136/559, 24.3%) and Regina (106/559, 19.9%). The North West (71/559, 12.7%), North East (60/559, 10.7%), Central East (35/559, 6.3%), South East (33/559, 5.9%) and North Central (29/559, 5.2%) regions provided the next highest proportion of responses. All other regions contributed less than 5% of the total responses each and 1/559 (0.2%) respondent provided no geographic location.
3.2.1. What do you think is needed to get vaccine hesitant individuals to get a COVID-19 vaccination?
There were 677 coded responses from answers to the question of what would promote vaccine uptake among unvaccinated individuals. The top five responses are outlined below, and the full list of response categories is available in Table 4.
The top five most common responses to this question, in order of prevalence, were: having access to, and trust in, reputable information sources (enabler/opportunity/envi ronmental context and resources; 227/677, 33.5%), mandates and restrictions (enabler/opportunity/environmental context and resources; 175/677, 25.8%), ease of access in terms of time, convenience, and cost (enabler/opportunity/environ mental context and resources; 69/677, 10.2%), issues with media, including coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation, etc. (barrier/opportunity/environmental context and resources; 56/677, 8.3%), and incentives like money, prizes, etc. (enabler/motivation/reinforcement; 36/677, 5.3%). Response ranking was similar across geographical regions, with the exception that the fourth most common response in both the North West and North East regions was beliefs about personal choice/freedom/feeling forced (barrier/motivation/beliefs about consequences; 5/74, 6.8% and 6/73, 8.2%, respectively).
3.2.2. Why, in your experience, are vaccine hesitant individuals not getting a COVID-19 vaccine?
There were 1359 coded responses from answers to the question of why vaccine hesitant individuals are not getting a COVID-19 vaccination. The top five responses are outlined below and the full list of response categories is available in Table 5.
|
Barrier/ Enabler |
COM-B1 | TDF2 | Theme | Count [n]3 | % |
|---|---|---|---|---|---|
| Barrier | Opportunity | Environmental Context and Resources | Media issues [e.g., coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation, etc.] | 272 | 20.0% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine necessity | 199 | 14.6% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine safety | 190 | 14.0% |
| Barrier | Motivation | Beliefs About Consequences | Beliefs about personal choice/freedom/feeling forced | 169 | 12.4% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine development | 137 | 10.1% |
| Barrier | Capability | Knowledge | Gaps in knowledge about COVID-19 vaccines | 114 | 8.4% |
| Barrier | Opportunity | Social Influences | Mistrust in government/public health response to COVID-19 | 109 | 8.0% |
| Barrier | Opportunity | Environmental Context and Resources | Access issues in terms of time, convenience, and cost | 69 | 5.1% |
| Barrier | Opportunity | Social Influences | Negative influence of close contacts and high-profile persons | 36 | 2.6% |
| Barrier | Motivation | Emotion | Fear of needles | 26 | 1.9% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about COVID-19 vaccine efficacy | 23 | 1.7% |
| Barrier | Motivation | Beliefs About Consequences | Concerns about adverse reactions [specific contraindications among patients, e.g., patients with rheumatologic diseases] | 9 | 0.7% |
| Barrier | Opportunity | Social Influences | Direct advice from medical professionals about vaccination | 6 | 0.4% |
2Theoretical Domains Framework
3N=1359.
The most common reason indicated by immunizers for why, in their experience, vaccine hesitant individuals were not seeking COVID-19 vaccines was due to media issues, including coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation, etc. (barrier/opportunity/environmental context and resources; 272/1359, 20.0%). This was the top-ranked theme in all but two geographic regions: the North East (where it was third) and South Central (in a three-way tie for fourth). The remaining top four responses were, in proportional order: concerns about COVID-19 vaccine necessity (barrier/motivation/beliefs about consequences; 199/1359, 14.6%), concerns about COVID-19 vaccine safety (barrier/motivation/beliefs about consequences; 190/1359, 14.0%), beliefs about personal choice/freedom/feeling forced (barrier/motivation/beliefs about consequences; 169/1359, 12.4%) and concerns about COVID-19 vaccine development (barrier/motivation/beliefs about consequences; 137/1359, 10.1%). When broken down by region, order and composition the top five themes were more varied for this question compared to the previous one, with some regions containing themes in their top five that were not part of the overall top five. For example, mistrust in government/public health response to COVID-19 (barrier/opportunity/social influences) was in the top five in the Far North East (2/20, 10.0%) and Far North West (7/66, 10.6%) regions.
4. DISCUSSION
In the context of this survey and concurrent local policy changes around third dose eligibility for travel purposes, it is not surprising that the most common reason for seeking a COVID-19 vaccination was to meet travel restrictions. As a behaviour change strategy, however, travel restrictions are underpinned by foreign governments i.e., other countries, states, or provinces imposing vaccine-related travel restrictions upon citizens foreign to those governments. For example, if the US government requires foreign visitors to provide proof of vaccination for entry into the USA [19], it may motivate Canadian citizens to seek a vaccination if they intend to travel to US destinations. However, if the Canadian government were to impose similar restrictions on US travellers, it is unlikely to have the same effect on Canadian citizens seeking a vaccination. Another way to view this may be governments recommending their citizens be vaccinated before travelling to certain destinations [20], as a way of preventing travellers from becoming infected with COVID-19 while abroad and/or returning home while still infective. This approach is similar to that which already exists for a number of communicable infectious diseases [21, 22]. Regardless of the approach, while there is a paucity of data in the literature to indicate the efficacy of instituting travel restrictions in promoting vaccine uptake among hesitant individuals, our results show that 33/194 (17.0%) respondents receiving their first dose indicated travel purposes as a reason for seeking a vaccine. Thus, employing travel restrictions in cooperation with neighbouring states, provinces, or countries may be an effective strategy to increase COVID-19 vaccine uptake.
Apart from travel purposes, the most common reason individuals reported seeking a vaccine was having a positive attitude toward or high perceived benefit of COVID-19 vaccines. Paul et al. [23] found that general mistrust in vaccines and concerns about future side effects would be barriers to achieving population immunity to COVID-19 through vaccination in the UK. Together, these data underscore the importance of public health messaging to target the mistrust barrier and promote positive attitudes towards COVID-19 vaccines. It is interesting that 64/139 (46.0%) of these responses in our survey were from individuals in the <20 and 30-39 year old age categories; these two categories combined also make up nearly half (121/262, 46.2%) of the individuals receiving their first dose (Table 1). However, these individuals have been eligible to receive a vaccine in Saskatchewan since at least May 20, 2021, 14 weeks prior to the survey, and even earlier for 30-39-year-olds and for individuals living in the Far North regions [13]. This indicates that a perceived benefit or positive attitude toward vaccines among these individuals is not enough to motivate them to seek a vaccine in a timely manner, and there are likely other factors to consider. For example, 3/149 (2.0%) respondents in the 30-39-year-old age category who indicated they had a positive attitude toward or high perceived benefit of COVID-19 vaccines also indicated that they were receiving their vaccine due to the next most common response: mandates or restrictions [which were becoming more prevalent among schools, businesses, and workplaces toward the end of the summer]. This information may be of use to policy makers who shouldn’t rely solely on promotion of the benefits of vaccination to motivate younger individuals to get vaccinated sooner rather than later during a pandemic.
Indeed, mandates and restrictions, the next most common response, appear to be more effective at motivating younger individuals and those seeking a first dose to get vaccinated given that 85/91 (93.4%) of those who provided this reason were <50 years old and 59/194 (30.4%) were receiving their first dose. Cascini et al. [24] showed that younger individuals were associated with increased vaccine hesitancy in their review of vaccine uptake among the global general population. A survey of 18 cities and counties across the US also showed that COVID-19 vaccination being required for activities was an important factor in the decision to get vaccinated for 68% of the general population [25]. In Saskatchewan, as of August 28, 2021, only 50.6% of individuals aged 12-49 were fully vaccinated compared to 82.8% of those >50 years old [3], indicating that vaccine mandates and restrictions may be an effective way to increase the number of fully vaccinated individuals among younger age categories.
Both immunizers and those seeking a COVID-19 vaccine had similar responses when asked how vaccine uptake could be promoted among hesitant individuals. The most common responses were mandates and restrictions and having access to, and trust in, reputable information sources. Similar to what many immunizers reported in our study, a survey of healthcare workers at a tertiary care hospital in the Czech Republic identified concerns about vaccine safety and efficacy and distrust in vaccine efficacy as top reasons for vaccine hesitancy among that population [26]. After those two responses, immunizers more often emphasized ease of access in terms of time, convenience, and cost as an enabler for vaccine hesitant individuals (this was also a top response in the Zencity et al. survey) [25], while those seeking a vaccination identified a barrier of beliefs about personal choice/freedom/feeling forced. Both respondent groups also identified incentives (e.g., money, prizes, etc). as a top five enabler, but immunizers more often identified media issues (e.g., coercion, negative influence, oversaturation, scare tactics, conflicting information, misinformation). Media issues was the sixth most popular comment among individuals seeking a COVID-19 vaccine, as well.
Both the media issues and access to, and trust in, reputable information sources categories contained abundant variation in the specifics of responses. For example, the availability and spread of misinformation via social media were often noted, as were continuously changing recommendations based on new information about COVID-19, vaccines, and public health measures, with respondents, indicating they believed that both of these led to confusion and low uptake among vaccine hesitant individuals. Many respondents wrote about a need for more plain language information [free of scientific jargon], while others said more data and epidemiologic information about viral spread and vaccine efficacy among population subgroups (e.g., percentage of fully vaccinated individuals who are infected or hospitalized with COVID-19) would be useful in persuading hesitant individuals to get vaccinated. In fact, the latter point has recently been implemented in the Government of Saskatchewan’s public updates [27]. Additionally, as seen in Table 5, immunizers most often indicated reasons that relate to concerns about COVID-19 vaccines i.e., vaccine development, safety, and necessity as potential reasons for hesitant individuals not seeking a vaccine (again, similar to the findings of [26]). All of the above can be addressed, in part, by ensuring individuals have access to, and trust in, reputable information sources.
Lastly, many individuals seeking a vaccine responded with, “I don’t know,” to the question of what would promote vaccine uptake among hesitant individuals. This indicates that many people are at a loss for how best to convince the remaining unvaccinated individuals across populations to take part in this most important public health measure.
4.1. Limitations
The low response rate among individuals receiving a vaccine is one limitation of this study and thus, caution is warranted when generalizing results to the broader population of vaccine hesitant individuals. Due to the provincial rollout of the survey through individual vaccine clinics, we are unable to determine the number of individuals receiving a vaccine who were actually offered the opportunity to complete the survey. Thus, the precise response rate is difficult to calculate.
Another limitation that potentially affects the generalization of our results is our inability to rigorously test the survey tools for validity and reliability due to the time constraints of the study. However, the inclusion of multiple stakeholders in the development of the surveys provided face validity. Additionally, the nature of the questions posed in the surveys probed broadly for behavioural mechanisms underlying vaccine hesitancy or vaccine-seeking behaviour and thus, are inherently open to some interpretation.
Another limitation of this study relates to our ability to extrapolate behaviour change mechanisms to promote vaccine uptake among hesitant individuals from survey responses provided by immunizers and those receiving a COVID-19 vaccine. Continuously evolving vaccination policies during survey development and while the survey was available meant that our survey population included unintended respondents (i.e., individuals receiving their third dose). However, 672/1012 (66.4%) respondents received a first or second dose and, by the definition provided by MacDonald et al. [1], these represent vaccine hesitant individuals given that the vaccine was widely available for at least 14 weeks prior to their vaccination. Thus, two-thirds of our responses from individuals seeking a vaccine could be considered from vaccine hesitant individuals. In addition, immunizers have the unique perspective of interacting face-to-face with both individuals receiving a vaccine and those who present to clinics with no intention of being vaccinated. Thus, immunizers have a unique and relevant perspective to offer on what they believe motivates individuals to get vaccinated.
Vaccine hesitancy is a complex issue as there are many reasons individuals choose not to seek vaccination, and these often differ in importance in different local contexts [24]. The barriers and enablers identified in our survey may be more relevant to residents of Saskatchewan. However, using the behavioural framework outlined by Crawshaw et al. [8] provides an approach grounded in behavioural science from which to make recommendations for behaviour change interventions more broadly. Additionally, locally collected data further emphasizes the relevance of the recommended interventions for addressing barriers and enablers within the local population.
CONCLUSION
Our survey of both immunizers and individuals seeking a COVID-19 vaccination in Saskatchewan indicates that mandates and restrictions, promoting positive attitudes towards vaccines, and ensuring people have access to, and trust in, reputable information sources are key enablers for promoting vaccine uptake among vaccine hesitant individuals. While mandates and restrictions may more effectively promote vaccine uptake among younger individuals, promoting reputable information and counteracting misinformation may be more effective at reaching a broader contingent of the population.
LIST OF ABBREVIATIONS
| COMB | = Capability + Opportunity + Motivation = Behaviour |
| COVID-19 | = Coronavirus Disease 2019 |
| REDCap | = Research Electronic Database Capture |
| SHA | = Saskatchewan Health Authority |
| TDF | = Theoretical Domains Framework |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was not reviewed by a research ethics board as it was performed as a time-sensitive quality improvement initiative. Quality improvement studies are exempted from ethical review by local (HIPA) and national (TCPS2) research guidelines.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human procedures were performed in accordance with the Declaration of Helsinki principles.
CONSENT FOR PUBLICATION
Consent was implied when participants submitted their survey responses.
STANDARD OF REPORTING
STROBE.
AVAILABILITY OF DATA AND MATERIALS
Data are available from the corresponding author on reasonable request.
FUNDING
No funding was received for conducting this study.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to thank the members of the Saskatchewan Health Authority Emergency Operations Centre and Integrated Health Incident Command Centres for their assistance in developing and distributing the surveys. We would also like to thank all those who took the time to participate in the survey and Michelle Degelman for her assistance in managing data collection and analysis.


