All published articles of this journal are available on ScienceDirect.
Exploring Adolescent Sexual Health Practices and Outcomes in Umguza and Mberengwa Districts in Zimbabwe
Abstract
Background:
Worldwide, adolescents have had limited access to reproductive health services due to several factors. The nature of communities and their organisations play a significant role in shaping adolescent sexual behaviours and practices. This study sought to explore the extent of the influence of community environmental factors in moulding adolescent sexual behaviours in Mberengwa and Umguza districts.
Methods:
A quantitative cross-sectional survey was conducted on 370 and 360 systematically selected adolescents in Mberengwa and Umguza districts, respectively, using a pre-tested researcher-administered questionnaire. The collected data was captured in Excel and imported to STATA Version 13 Standard Edition for analysis. Different statistical methods (both descriptive and inferential) were utilised to interrogate collected data and inferences made.
Results:
Most respondents were female and were between 13-17 years. Most of the respondents were literate. Umguza district had a significantly higher prevalence of pregnancies, Sexually Transmitted Infections, and a higher number of adolescents engaging in sexual activities. Predictors of Sexually Transmitted Infections and pregnancies were the sex of the respondent, tribe, sexual encounters, age, and religion.
Conclusion:
Adolescents are at risk of contracting Sexually Transmitted Infections and impregnation as they engage in risky sexual behaviours, as evidenced by the findings. The two districts have a significantly higher prevalence of having sex than the national average.
1. INTRODUCTION
Adolescents have had limited access to reproductive health (RH) services due to several factors globally [1]. Since most adolescents are below the age who can voluntarily participate in any activities regarding their SH, they end up shunning accessing these services [2]. Most countries have laws and policies that stipulate ages of consent at around 16 /18 years and above, with those younger than these specified ages requiring parental consent for them to access SH services, such as HIV counselling and testing, access to contraceptive products, and many more [2, 3]. It should be noted that requiring parental consent for adolescents is meant to protect them from being taken advantage of or abused in general [3, 4]. However, requiring parental consent on sexual health-related issues is a significant barrier in acquiring such services as adolescents' right to privacy is invaded, and they likely end up in trouble with their parents or guardians [4].
Health Systems (HSs) significantly influence or shape adolescents' sexual behaviours [5]. Some HSs have been less accommodative to adolescents by being judgemental [3]. This scenario has been pointed out as a significant hindrance to SH services by adolescents as, the majority of times, they are not given enough room to be comfortable to inquire and seek clarity on the services they need [3, 6, 7].
The Zimbabwean scenario is not different from what is found in many countries as they emphasise parental consent on many issues/ services consumed by adolescents [8]. However, in collaboration with some Non-Governmental Organisations (NGOs), the country has taken giant steps to try and accommodate adolescents that are: the provision of adolescent-friendly facilities where some institutions have dedicated consultations rooms and private entry to those adolescents to facilitate and aid comfort and privacy for adolescents to utilise these services fully, training of the Health Service Providers (HSPs) to be sensitive to ASH and develop strategies that facilitate and promote high demand and uptake of SH services, being sensitive to religious and cultural factors, provide age-appropriate services to mention a few [9-12]. However, not much has happened to transform the IHS such that its efficiency and effectiveness are also improved as far as management of ASH issues is concerned [13]. It is worth noting that the IHS in Zimbabwe serves a significant proportion of the population; therefore, its transformation and improvement of services are also significant [14].
Mberengwa and Umguza districts have the highest prevalence of sexually transmitted infections (STIs) and teenage pregnancy compared to other districts in Zimbabwe [12, 15]. There is also a high rate of school dropouts amongst adolescents in these two districts. Not much has been done to assess the impact of health systems (HSs) on ASH, particularly in highly cultural areas, such as Mberengwa and Umguza districts. Therefore, this paper sought to explore the extent of the influence of Indigenous Health Systems (IHS) and Modern Health Systems (MHS) in moulding adolescent sexual behaviours in Mberengwa and Umguza districts. Furthermore, the study further explored adolescent sexual experiences. It sought to explore their views (adolescents) on whether it was essential to integrate these two systems (IHS and MHS) and, if so, how. Findings from this study provide a window of opportunity for different stakeholders to leverage in crafting and implementing policies and programs that are meant to improve adolescents' sexual health outcomes. From these findings, informed decisions founded on empirical evidence could ensure that contextual and relevant programs and policies that respond to the needs of adolescents are crafted and implemented.
2. MATERIALS AND METHODS
2.1. Study Setting
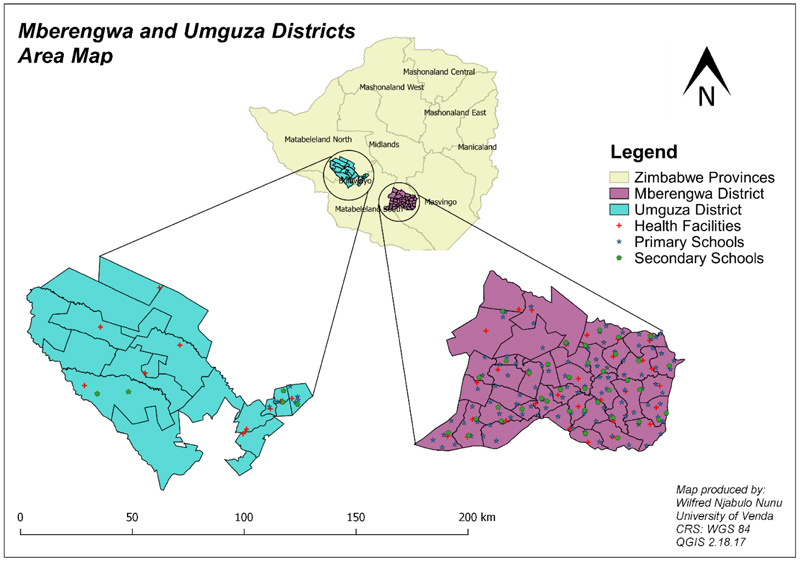
The study was conducted in Mberengwa and Umguza districts. These districts are highly cultural and have the highest prevalence of STIs and teenage pregnancies [16-18]. Most individuals in these districts are of low socio-economic quintile as the districts are rural and most survive through peasant farming and illegal gold panning [19]. Most male adolescents who drop out of school in these districts usually end up as gold panners or migrate to neighbouring countries like South Africa and Botswana, searching for greener pastures [20-22]. The two districts are captured in Fig. (1).
2.2. Study Design
A quantitative cross-sectional survey was conducted on adolescents in Mberengwa and Umguza districts. This design enabled the researcher to explore relationships between different variables and adolescent sexual practices and experiences [23]. This design also allowed for the prevalence of STIs and teenage pregnancies to be estimated in the adolescent populations in the two districts [23]. Furthermore, through this design, multiple methods of analysis could be used to triangulate the findings over and above the fact that it was an affordable approach as there was no need to follow up with the respondents [23]. It saved time and ensured efficient resource utilisation [23].
2.3. Study Population and Sampling
This study targeted adolescents aged 10 to 19 years, as defined by the World Health Organisation (WHO) [24]. Based on the 2012 Zimbabwean Census Report, it was estimated that there were 68 339 adolescents in Umguza and 168 087 in Mberengwa in 2012 [25]. Adjusting this population using the 1.56% population growth rate per annum, the adolescent populations were estimated to be 73840 and 181618 for Umguza and Mberengwa, respectively, in 2019. A sample size calculator on EPI INFO was then used to estimate the minimum sample size to make meaningful inferences. The attribute used in the sample size determination was a 95% Confidence Level with a margin of error of 5% and a response distribution of 50%. This scenario gave a sample size of 360 and 370 for Umguza and Mberengwa districts, respectively. Stratified random sampling was then used to ensure that all district wards were proportionally covered. Mberengwa has 37 wards; therefore, ten participants were recruited from each ward, while in Umguza (18 wards), twenty were recruited from each ward. Participants were identified through community registers at the ward level and then followed up at schools or homesteads for data collection.
2.4. Data Collection Tools
A pre-tested semi-structured researcher-administered questionnaire was used to collect data from respondents. The researchers administered the questionnaire to improve the response rate and completeness of the questions, as the targeted respondents were adolescents. The researchers clarified the questions when the respondents did not understand the poised questions. This ensured that the adolescents fully understood the questions that were being asked and catered for those that were illiterate. The tool was adapted from John Cleland's questionnaire for surveys on young people's sexual and reproductive health on the WHO website [26]. The questionnaire (developed in English and then translated to Ndebele and Shona) had six sections: demographics; practices; reasons for engaging in sexual activities and extent of supervision; the role of identified IHSs and their relationship with adolescent sexual experiences; the role of MHSs in shaping adolescent sexual experiences; and lastly adolescents' views on integrating IHS and MHS. The questionnaire comprised open-ended and closed questions and took 15 to 30 minutes to administer.
2.5. Data Management and Analysis
The collected data were captured on an excel spreadsheet and imported into STATA Version 13 Standard Edition for analysis. Firstly, a correlation test was performed on all variables of interest to ascertain whether there was multicollinearity [27, 28]. If the correlation analysis results in an outcome greater than 0.8, multicollinearity exists [29]. Multicollinearity occurs when independent variables in a model are associated [30]. This association is problematic because independent variables should be independent [30]. If this association between variables is high enough, it can cause problems when you fit the model and interpret the results [30]. Furthermore, a Stepwise Logistic Regression (SLR) analysis was conducted to ascertain the validity of the predictor variables that were subsequently used to build the Multiple Logistic Regression (MLR) models. This was done using Bivariate analysis to determine which variables were to be used to construct the MLR model, where different variables of interest were cross-tabulated with the outcome variables “Prevalence of STIs and Pregnancy/impregnating.” All variables with a p-value of 0.2 or less qualified for the forward selection and were tested on the MLR for associations. It is standard practice to forward selected variables with a p-value of 0.2 or less to minimise the loss of variables in the early stages of model building [31, 32]. This method is often used to provide an initial screening of the candidate variables when many variables are involved [32, 33]. Finally, all variables with a p-value of 0.05 or less were presented in the final MLR model. The MLR model was used to determine the relationship between different variables and how they influenced STI prevalence and teenage pregnancies/impregnating (as these were used as the outcome variables for this model). Furthermore, Chi-squared tests (χ2), Cox Regression-Breslow method of ties, and Kaplan-Meier Survival Estimates were used to compare STIs prevalence, pregnancy/impregnation, and engagement in sexual intercourse by adolescents in the two districts. These specialized tests enable one to compare patterns between two populations and make inferences on the differences and similarities.
3. RESULTS
3.1. Variable Correlation Test
All the covariates had a correlation output of less than 0.8, symbolising no relationship between the covariates. Therefore, the covariates were not biased as no multicollinearity was detected. Therefore, these variables were passed to be fit for tabulations in the building of the MLR Model. The findings of this test are presented in Table 1.
Table 1.
| - | Sex of Respondent | Attended School | Religion | Tribe | Employment Status | Involvement in Cultural Ceremonies | Engagement in Sexual Activities | Suffered from STIs | Pregnancy |
|---|---|---|---|---|---|---|---|---|---|
| Sex of Respondent | 1.00 | * | |||||||
| Attended School | * | * | |||||||
| Religion | 0.26 | * | 1.00 | ||||||
| Tribe | 0.09 | * | 0.20 | 1.00 | |||||
| Employment Status | 0.12 | * | 0.06 | -0.02 | 1.00 | ||||
| Involvement in cultural ceremonies | 0.01 | * | 0.07 | 0.13 | -0.01 | 1.00 | |||
| Engagement in sexual activities | -0.09 | * | 0.03 | 0.12 | 0.01 | 0.04 | 1.00 | ||
| Suffered from STIs | -0.15 | * | 0.13 | -0.02 | 0.21 | 0.09 | 0.06 | 1.00 | |
| Pregnancy | 0.0874 | 0.19 | -0.05 | 0.20 | 0.05 | 0.07 | 0.65 | 1.00 |
3.2. Socio-demographic Characteristics
Most respondents were females in both districts, accounting for over 50% of respondents. The dominant age group was 13-17 years, and nearly 100% were literate. The majority had attended school, and none of the respondents had been or attained a tertiary level education. The percentage prevalence of STIs, engagement in sexual activities, and percentage prevalence of pregnancies were significantly higher in Umguza than in Mberengwa Districts (STIs 10.3 6.8; had sex 26.7, 20.3, and prevalence of pregnancies 12.5, 7.0 respectively). These findings are presented in Table 2.
3.3. Outcomes of Bivariate Cross-tabulations using the SLR.
3.3.1. Using the Outcome Variable “Having Suffered from STIs.”
Several variables gave a p-value of less than 0.2 and were forward selected to build the MLR using “Having suffered from STIs” as an outcome variable. These findings are presented in Table 3.
| - |
Mberengwa n (%) |
Umguza n (%) |
|---|---|---|
| Sex | ||
| Male | 178 (48.1) | 154 (42.8) |
| Female | 192 (51.9) | 206 (57.2) |
| Age | ||
| 10-12 years | 146 (39.5) | 101 (28.1) |
| 13-17 years | 200 (54.0) | 216 (60.0) |
| 18-19 years | 24 (6.5) | 43 (11.9) |
| Ability to Read | ||
| Yes | 366 (98.9) | 348 (96.7) |
| No | 4 (1.1) | 12 (3.3) |
| Ever Attended School | ||
| Yes | 364 (98.4%) | 357 (99.2) |
| No | 6 (1.6%) | 3 (0.8) |
| Level of Education | ||
| None | 195 (52.7) | 201 |
| Primary | 160 (43.2) | 36 |
| Secondary | 15 (4.1) | 118 |
| Tertiary | 0 | 0 |
| Currently Attending School | ||
| Yes | 343 (92.7) | 329 (93.4) |
| No | 27(7.3) | 31 (5.3) |
| Number of years you expect to be at school | ||
| <10 years | 175 (51.3) | 137 (43.2) |
| 10+ years | 166 (48.7) | 180 (8.6) |
| Age when one center school | ||
| <10 years | 0 | 0 |
| 10-12 years | 5 (18.5) | 3 (9.7) |
| 13-17 years | 22 (81.5) | 28 (90.3) |
| 18-19 years | 0 | 0 |
| Religion | ||
| None | 58 (15.6) | 53 (15.1) |
| Catholic | 9 (2.4) | 15 (4.3) |
| Protestant | 76 (20.5) | 72 (20.5) |
| Pentecostal | 106 (28.6) | 110 (31.3) |
| Other | 121 (32.7) | 101 (28.8) |
| Frequency of attending religious services | ||
| Every day | 28 (7.6) | 33 (9.3) |
| At least once a week | 259 (70) | 243 (68.3) |
| At least once a month | 23 (6.2) | 28 (7.9) |
| At least once a year | 3 (0.8) | 3 (0.8) |
| Never | 57 (15.4) | 49 (13.8) |
| Importance of religion | ||
| Important | 139 (81.3) | 321 (92.5) |
| Not Important | 32 (18.7) | 26 (7.5) |
| Tribe | ||
| Xhosa | 2 (0.5) | 44 (12.4) |
| Ndebele | 165 (44.6) | 175 (49.3) |
| Lemba | 29 (7.8) | 6 (1.7) |
| Shona | 143 (38.6) | 60 (16.9) |
| Other | 31(8.4) | 70 (19.7) |
| Employed | ||
| Yes | 14 (3.8) | 15 (4.3) |
| No | 356 (96.2) | 336 (95.7) |
| Prevalence of STIs | ||
| Suffered from STI | 25 (6.8) | 38 (10.3) |
| Did not suffer from STI | 345 (93.2) | 322 (89.7) |
| Had Sex | ||
| Yes | 75 (20.3) | 96 (26.7) |
| No | 295 (79.7) | 264 (73.3) |
| Pregnancy/Impregnating | ||
| Ever pregnant/ Impregnated | 26 (7.0) | 45 (12.5) |
| Never pregnant or impregnated | 344 (93.7) | 315 (87.5) |
| Nature of Work | ||
| Herding cattle; Cleaning neighbours homesteads; Cleaning of neighbours homesteads who are based in South Africa; Informal gold panning; Vending; Caretaker; Teller; Working at a shop; Working in South Africa; Gardener; doing piece jobs | ||
| Average amount earned | ||
| 410 | 350 | |
| Outcome Variable Having Suffered from STIs | |||||
|---|---|---|---|---|---|
| Mberengwa n(Yes 25: No 345) | Umguza n(Yes 38: No 322) | ||||
| Have STIs (%) | Do not have STIs (%) | Have STIs (%) | Do Not have STIs (%) | ||
| Sex | |||||
| Male | 37.0 | 49.0 | 53.8 | 30.4 | |
| Female | 63.0 | 51.0 | 46.2 | 69.6 | |
| P-value | 0.111 | 0,022* | |||
| Age | |||||
| 10-12 years | 0 | 13.7 | 2.6 | 19.6 | |
| 13-17 years | 70.4 | 72.5 | 53.8 | 58.9 | |
| 18-19 years | 29.6 | 13.7 | 43.6 | 21.4 | |
| P-value | 0.049* | 0.011* | |||
| Ability to Read | |||||
| Yes | 100.0 | 98.0 | 94.9 | 94.6 | |
| No | 0 | 2.0 | 5.1 | 5.4 | |
| P-value | 0.464 | 0.961 | |||
| Ever Attended School | |||||
| Yes | 100. | 100.0 | 100.0 | 100.0 | |
| No | 0 | 0 | 0 | 0 | |
| P-value | N/A | N/A | |||
| Level of Education Completed | |||||
| None | 96.3 | 64.7 | 66.7 | 55.4 | |
| Primary | 3.7 | 5.9 | 20.5 | 12.5 | |
| Secondary | 0 | 0 | 0 | 0 | |
| Tertiary | 0 | 29.4 | 12.8 | 32.1 | |
| P-value | 0.005* | 0.083* | |||
| Currently Attending School | |||||
| Yes | 100.0 | 100.0 | 100.0 | 87.5 | |
| No | 0 | 0 | 0 | 12.5 | |
| P-value | N/A | 0.023* | |||
| Number of years you expect to be at school | |||||
| <10 years | 100 | 44.4 | 33.3 | 35.0 | |
| 10+ years | 0 | 55.6 | 66.7 | 65.0 | |
| P-value | 0.001* | 0.896 | |||
| Age when one center school | |||||
| <10 years | 0 | 0 | 100.0 | 100.0 | |
| 10-12 years | 5.6 | 20.0 | 0 | 0 | |
| 13-17 years | 94.4 | 80.0 | 0 | 0 | |
| 18-19 years | 0 | 0 | 0 | 0 | |
| P-value | 0.311 | N/A | |||
| Religion | |||||
| None | 11.1 | 13.7 | 26.3 | 8.9 | |
| Catholic | 33.3 | 0 | 2.0 | 8.9 | |
| Protestant | 33.3 | 21.6 | 21.1 | 32.1 | |
| Pentecostal | 29.6 | 37.3 | 34.2 | 14.3 | |
| Other | 25.9 | 27.5 | 13.2 | 35.7 | |
| P-value | 0.715 | 0.007* | |||
| Tribe | |||||
| Xhosa | 0 | 3.9 | 17.9 | 23.2 | |
| Ndebele | 7.4 | 41.2 | 48.7 | 35.7 | |
| Lemba | 44.4 | 5.9 | 0 | 1.8 | |
| Shona | 44.4 | 37.3 | 7.7 | 16.1 | |
| Other | 3.7 | 11.8 | 25.6 | 23.2 | |
| P-value | 0.000* | 0.512 | |||
| Employment Status | |||||
| Employed | 25.9 | 29.0 | 15.4 | 7.5 | |
| Not Employed | 74.1 | 71.0 | 84.6 | 92.4 | |
| P-value | 0.004* | 0.166* | |||
| Average Income | |||||
| Income | 400 | 500 | 308 | 200 | |
| P-value | N/A | N/A | |||
| Communication with Parents or guardians | |||||
| Very easy | 18.5 | 58.9 | 30.8 | 55.4 | |
| Easy | 18.5 | 11.8 | 23.1 | 12.5 | |
| Average | 14.8 | 2.0 | 23.1 | 5.4 | |
| Very difficult | 44.4 | 13.7 | 7.7 | 14.3 | |
| Difficult | 3.7 | 11.8 | 10.3 | 12.5 | |
| Do not see them | 0 | 2.0 | 5.1 | 0 | |
| P-value | 0.002* | 0.015* | |||
| Discussion of sex-related issues with anyone | |||||
| Yes | 59.3 | 35.8 | 51.3 | 55.4 | |
| No | 40.7 | 64.2 | 48.7 | 44.6 | |
| P-value | 0.258 | 0.695 | |||
| Source of sexual information | |||||
| Initiation schools | 0 | 8.0 | 0 | 0 | |
| School teacher | 40.0 | 48.0 | 0 | 0 | |
| Parents/guardians | 0 | 4.0 | 48.6 | 40.4 | |
| Siblings | 0 | 2.0 | 5.7 | 8.5 | |
| Other family members | 28.0 | 10.0 | 14.3 | 12.7 | |
| Friends | 12.0 | 16.0 | 11.4 | 14.9 | |
| Health Care Providers | 8.0 | 6.0 | 8.6 | 40.4 | |
| Media | 0 | 0 | 11.4 | 4.3 | |
| Other specify | 12.0 | 6.0 | 0 | 0 | |
| P-value | 0.320 | 0.730 | |||
| Involved in cultural initiation | |||||
| Yes | 18.5 | 21.6 | 33.3 | 20.0 | |
| No | 81.5 | 78.4 | 66.7 | 80.0 | |
| P-value | 0.751 | 0.154* | |||
| Had sex | |||||
| Yes | 100.0 | 100.0 | 100.0 | 98.2 | |
| No | 0 | 0 | 0 | 1.8 | |
| P-value | N/A | 0.401 | |||
| Age at First Sexual Encounter | |||||
| <10 years | 0 | 9.8 | 10.3 | 3.6 | |
| 10-12 years | 11.1 | 21.6 | 25.6 | 46.4 | |
| 13-17 years | 88.9 | 64.7 | 64.1 | 50.0 | |
| 18-19 years | 0 | 3.9 | 0 | 0 | |
| P-value | 0.103* | 0.079* | |||
| Methods used for preventing STIs and pregnancy | |||||
| Condom | 14.8 | 52.1 | 46.2 | 30.4 | |
| Withdrawal | 29.6 | 14.6 | 23.1 | 26.8 | |
| Pill | 7.4 | 0 | 0 | 0 | |
| Injection | 0 | 0 | 0 | 0 | |
| Other | 48.1 | 33.3 | 30.8 | 42.9 | |
| P-value | 0.005* | 0.277 | |||
| Treatment of STIs | |||||
| Went to traditional healers/ herbalist |
38.5 | 0 | 100.0 | 100.0 | |
| Went to a health facility | 42.3 | 100.0 | 0 | 0 | |
| Did not seek treatment | 11.5 | 0 | 0 | 0 | |
| Other specify | 7.7 | 0 | 0 | 0 | |
| P-value | 0.478 | N/A | |||
| Pregnant or Impregnated | |||||
| Yes | 92.9 | 2.1 | 74.1 | 32.1 | |
| No | 7.1 | 97.9 | 25.6 | 67.9 | |
| P-value | 0.000* | 0.000* | |||
| Sexual Encounter(s) | |||||
| I wanted to have sex | 51.9 | 31.4 | 56.4 | 21.4 | |
| My partner wanted us to have sex | 18.5 | 19.6 | 15.4 | 44.6 | |
| Neither of us wanted, but it just happened | 11.1 | 31.4 | 23.1 | 10.7 | |
| I was culturally obliged to | 14.9 | 0 | 0 | 14.3 | |
| Other specify | 3.7 | 17.6 | 5.1 | 8.9 | |
| P-value | 0.004* | 0.000* | |||
| Taught to have sex | |||||
| Yes | 25.9 | 40.0 | 74.4 | 85.7 | |
| No | 74.1 | 60.0 | 25.6 | 14.3 | |
| P-value | 0.355 | 0.000* | |||
| Source of information | |||||
| Cultural initiation | 33.3 | 15.4 | 17.9 | 0 | |
| Brothers | 11.1 | 15.4 | 3.6 | 21.6 | |
| Sisters | 11.1 | 46.2 | 0 | 13.5 | |
| School Curriculum | 33.3 | 15.4 | 50.0 | 51.4 | |
| Other family members | 11.1 | 3.8 | 25.0 | 8.1 | |
| Other specify | 0 | 0 | 3.6 | 5.4 | |
| P-value | 0.118* | 0.008* | |||
| Activities at initiation schools | |||||
| Sexual education | 15.0 | 25.6 | 32.4 | 22.4 | |
| Circumcision | 30.0 | 20.9 | 14.7 | 10.2 | |
| Vaginal modifications | 20.0 | 4.7 | 17.6 | 20.4 | |
| Other | 35.0 | 48.8 | 35.3 | 46.9 | |
| P-value | 0.163* | 0.523 | |||
| Do these activities influence your decision to engage in sexual activities | |||||
| Yes | 24.0 | 29.3 | 35.3 | 32.0 | |
| No | 76.0 | 70.7 | 64.7 | 68.0 | |
| P-value | 0.641 | 0.753 | |||
| Encountered any challenge | |||||
| Yes No P-value |
11.5 | 12.9 | 20.7 | 4.4 | |
| 88.5 | 87.1 | 79.3 | 95.6 | ||
| 0.876 | 0.028* | ||||
| Health education | |||||
| Yes | 44.7 | 56.9 | 69.2 | 60.0 | |
| No | 55.3 | 43.1 | 30.8 | 40.0 | |
| P-value | 0.067* | 0.359 | |||
| Interaction with health service providers | |||||
| Through school health services | 85.7 | 69.7 | 43.8 | 51.5 | |
| From health facility | 9.5 | 15.2 | 37.5 | 30.3 | |
| Through media | 0 | 12.1 | 15.6 | 18.2 | |
| Other specify | 4.8 | 3.0 | 3.1 | 0 | |
| P-value | 0.334 | 0.671 | |||
| IHS important in shaping sexual health | |||||
| Yes | 55.6 | 56.0 | 41.0 | 42.9 | |
| No | 44.4 | 44.0 | 59.0 | 57.1 | |
| P-value | 0.970 | 0.859 | |||
| MHS being important in shaping sexual health | |||||
| Yes | 30.5 | 47.4 | 64.1 | 60.0 | |
| No | 69.5 | 52.6 | 35.9 | 40.0 | |
| P-value | 0.179* | 0.687 | |||
| Activities at initiation schools | |||||
| Sexual education | 15.0 | 25.6 | 32.4 | 22.4 | |
| Circumcision | 30.0 | 20.9 | 14.7 | 10.2 | |
| Vaginal modifications | 20.0 | 4.7 | 17.6 | 20.4 | |
| Other | 35.0 | 48.8 | 35.3 | 46.9 | |
| P-value | 0.163* | 0.523 | |||
| Do these activities influence your decision to engage in sexual activities | |||||
| Yes | 64.0 | 29.3 | 35.3 | 32.0 | |
| No | 36.0 | 70.7 | 64.7 | 68.0 | |
| P-value | 0.641 | 0.753 | |||
| Encountered any challenge | |||||
| Yes | 11.5 | 46.0 | 20.7 | 4.4 | |
| No | 88.5 | 54.0 | 79.3 | 95.6 | |
| P-value | 0.876 | 0.028* | |||
| Health education | |||||
| Yes | 44.7 | 56.9 | 69.2 | 60.0 | |
| No | 55.3 | 43.1 | 30.8 | 40.0 | |
| P-value | 0.067* | 0.359 | |||
| Interaction with health service providers | |||||
| Through school health services | 85.7 | 69.7 | 43.8 | 51.5 | |
| From health facility | 9.5 | 15.2 | 37.5 | 30.3 | |
| Through media | 0 | 12.1 | 15.6 | 18.2 | |
| Other specify | 4.8 | 3.03 | 3.1 | 0 | |
| P-value | 0.334 | 0.671 | |||
| IHS important in shaping sexual health | |||||
| Yes | 55.6 | 56.0 | 41.0 | 42.9 | |
| No | 44.4 | 44.0 | 59.0 | 57.1 | |
| P-value | 0.970 | 0.859 | |||
| MHS being important in shaping sexual health | |||||
| Yes | 64.3 | 80.4 | 64.1 | 60.0 | |
| No | 35.7 | 19.6 | 35.9 | 40.0 | |
| P-value | 0.179* | 0.687 | |||
3.3.2. Using the outcome variable “pregnant or impregnated.”
Some variables were associated with the outcome variable (age, level of education, and the number of years expected to be at school, just to name a few). A significant proportion of the variables gave a p-value of 0.2 or less and thus were selected to be included in the final building of the MLR model. These findings are presented in Table 4.
Table 4.
| Outcome Variable Pregnant or Impregnated | |||||
|---|---|---|---|---|---|
| Mberengwa n(Yes 26: No 344) | Umguza n(Yes 45: No 315) | ||||
| Have STIs | Do not have STIs | Have STIs | Do Not have STIs | ||
| Sex | |||||
| Male | 35.7 | 50.0 | 42.1 | 54.4 | |
| Female | 64.3 | 50.0 | 57.9 | 45.6 | |
| P-value | 0.200* | 0.241 | |||
| Age | |||||
| 10-12 years | 0 | 12.5 | 0 | 25.0 | |
| 13-17 years | 67.9 | 75.0 | 48.9 | 64.6 | |
| 18-19 years | 32.1 | 12.5 | 51.1 | 10.4 | |
| P-value | 0.029* | 0.000* | |||
| Ability to Read | |||||
| Yes | 100.0 | 97.9 | 91.5 | 97.9 | |
| No | 0 | 2.1 | 8.5 | 2.1 | |
| P-value | 0.442 | 0.161* | |||
| Ever Attended School | |||||
| Yes | 100.0 | 100.0 | 100.0 | 100.0 | |
| No | 0 | 0 | 0 | 0 | |
| P-value | N/A | N/A | |||
| Level of Education | |||||
| None | 96.4 | 66.7 | 70.2 | 50.0 | |
| Primary | 3.6 | 6.3 | 19.1 | 12.5 | |
| Secondary | 0 | 0 | 0 | 0 | |
| Tertiary | 0 | 27.1 | 10.6 | 37.5 | |
| P-value | 0.007* | 0.009* | |||
| Currently Attending School | |||||
| Yes | 100.0 | 100.0 | 52.9 | 0 | |
| No | 0 | 0 | 47.1 | 100.0 | |
| P-value | N/A | 0.007* | |||
| Number of years you expect to be at school | |||||
| <10 years | 100 | 48.9 | 35.0 | 34.1 | |
| 10+ years | 0 | 51.2 | 65.0 | 65.9 | |
| P-value | 0.003* | 0.947 | |||
| Age when one center school | |||||
| <10 years | 5.0 | 33.3 | 100.0 | 100.0 | |
| 10-12 years | 95.0 | 66.7 | 0 | 0 | |
| 13-17 years | 0 | 0 | 0 | 0 | |
| 18-19 years | 0 | 0 | 0 | 0 | |
| P-value | 0.104* | N/A | |||
| Religion | |||||
| None | 14.3 | 12.5 | 23.9 | 8.3 | |
| Catholic | 0 | 0 | 10.9 | 2.1 | |
| Protestant | 35.7 | 18.8 | 16.7 | 37.5 | |
| Pentecostal | 28.6 | 37.5 | 28.3 | 16.7 | |
| Other | 14.3 | 31.3 | 19.6 | 35.4 | |
| P-value | 0.375 | 0.009* | |||
| Tribe | |||||
| Xhosa | 0 | 4.2 | 27.7 | 14.6 | |
| Ndebele | 10.7 | 37.5 | 34.0 | 47.9 | |
| Lemba | 46.4 | 4.2 | 2.1 | 0 | |
| Shona | 39.3 | 41.7 | 4.3 | 20.8 | |
| Other | 3.8 | 12.5 | 31.9 | 16.7 | |
| P-value | 0.000* | 0.021* | |||
| Employment Status | |||||
| Employed | 25.0 | 4.2 | 12.8 | 8.9 | |
| Not Employed | 75.0 | 95.8 | 87.2 | 91.1 | |
| P-value | 0.007* | 0.184* | |||
| Average Income | |||||
| Income | 400 | 500 | 393 | 106 | |
| P-value | N/A | N/A | |||
| Communication with parents or guardians | |||||
| Very easy | 14.3 | 60.4 | 40.4 | 50.0 | |
| Easy | 17.9 | 12.5 | 17.0 | 16.7 | |
| Average | 17.9 | 0 | 21.3 | 4.2 | |
| Very difficult | 42.9 | 14.6 | 10.6 | 12.5 | |
| Difficult | 7.1 | 10.4 | 6.4 | 16.7 | |
| Do not see them | 0 | 2.1 | 4.3 | 0 | |
| P-value | 0.000* | 0.068* | |||
| Discussion of sex-related issues with anyone | |||||
| Yes | 60.7 | 50.0 | 48.9 | 54.5 | |
| No | 39.3 | 50.0 | 51.1 | 45.5 | |
| P-value | 0.195* | 0.358 | |||
| Source of Sexual Information | |||||
| Initiation schools | 0 | 8.5 | 0 | 2.2 | |
| School teacher | 38.5 | 46.8 | 0 | 0 | |
| Parents/guardians | 0 | 4.3 | 34.1 | 45.7 | |
| Siblings | 0 | 2.1 | 4.5 | 8.7 | |
| Other family members | 26.9 | 10.6 | 18.2 | 6.5 | |
| Friends | 11.5 | 17.0 | 11.4 | 13.0 | |
| Health Care Providers | 7.7 | 6.4 | 13.6 | 13.0 | |
| Other specify | 15.4 | 4.3 | 6.8 | 8.7 | |
| P-value | 0.204 | 0.351 | |||
| Involved in cultural initiation | |||||
| Yes | 17.9 | 20.8 | 56.5 | 47.0 | |
| No | 82.1 | 79.2 | 43.5 | 53.0 | |
| P-value | 0.753 | 0.430 | |||
| Had sex | |||||
| Yes | 100.0 | 100.0 | 100.0 | 97.9 | |
| No | 0 | 0 | 0 | 2.1 | |
| P-value | N/A | 0.320 | |||
| Age at First Sexual Encounter | |||||
| <10 years | 0 | 14.3 | 2.1 | 10.4 | |
| 10-12 years | 14.3 | 18.8 | 31.9 | 43.8 | |
| 13-17 years | 85.7 | 68.8 | 66.0 | 45.8 | |
| 18-19 years | 0 | 4.2 | 0 | 0 | |
| P-value | 0.223 | 0.075* | |||
| Methods used for preventing STIs and pregnancy | |||||
| Condom | 14.3 | 54.3 | 42.6 | 31.3 | |
| Withdrawal | 28.6 | 15.2 | 25.5 | 25.0 | |
| Pill | 7.1 | 0 | 0 | 0 | |
| Injection | 0 | 0 | 0 | 0 | |
| Other | 50.0 | 30.4 | 31.9 | 43.8 | |
| P-value | 0.003* | 0.427 | |||
| Treatment of STIs | |||||
| Went to traditional healers/ herbalist |
40.0 | 0 | 48.3 | 20.0 | |
| Went to a health facility | 40.0 | 100.0 | 51.7 | 80.0 | |
| Did not seek treatment | 12.0 | 0 | 0 | 0 | |
| Other specify | 8.0 | 0 | 0 | 0 | |
| P-value | 0.701 | 0.117* | |||
| Pregnant or Impregnated | |||||
| Yes | 100.0 | 0 | 100.0 | 0 | |
| No | 0 | 100.0 | 0 | 100.0 | |
| P-value | 0.000* | 0.000* | |||
| Sexual Encounter (s) | |||||
| I wanted to have sex | 50.0 | 33.3 | 53.2 | 18.8 | |
| My partner wanted us to have sex | 17.9 | 20.8 | 21.3 | 43.8 | |
| Neither of us wanted, but it just happened | 14.3 | 31.3 | 17.0 | 14.6 | |
| I was culturally obliged to | 14.3 | 0 | 8.5 | 8.3 | |
| Other specify | 3.6 | 14.6 | 0 | 14.6 | |
| P-value | 0.016* | 0.001* | |||
| Taught to have sex | |||||
| Yes | 28.6 | 40.4 | 48.9 | 53.6 | |
| No | 71.4 | 59.6 | 51.1 | 46.3 | |
| P-value | 0.435 | 0.659 | |||
| Source of information | |||||
| Cultural initiation | 33.3 | 17.4 | 6.9 | 9.1 | |
| Brothers | 11.1 | 17.4 | 3.4 | 24.2 | |
| Sisters | 11.1 | 43.5 | 10.3 | 6.1 | |
| School Curriculum | 33.3 | 17.4 | 55.2 | 51.5 | |
| Other specify | 11.1 | 4.3 | 24.1 | 9.1 | |
| P-value | 0.166* | 0.094* | |||
| Activities at initiation schools | |||||
| Sexual education | 14.3 | 27.5 | 40.0 | 14.0 | |
| Circumcision | 28.6 | 20.0 | 12.5 | 11.6 | |
| Vaginal modifications | 23.8 | 2.5 | 17.5 | 20.9 | |
| Other | 33.3 | 50.0 | 30.0 | 54.5 | |
| P-value | 0.033* | 0.056* | |||
| Do these activities influence your decision to engage in sexual activities | |||||
| Yes | 29.6 | 26.3 | 43.2 | 22.5 | |
| No | 70.4 | 73.7 | 56.8 | 77.5 | |
| P-value | 0.769 | 0.045* | |||
| Encountered any challenge | |||||
| Yes | 42.9 | 50.0 | 62.5 | 53.0 | |
| No | 57.1 | 50.0 | 37.5 | 47.0 | |
| P-value | 0.723 | 0.612 | |||
| Health education | |||||
| Yes | 82.1 | 54.2 | 53.3 | 44.1 | |
| No | 17.9 | 45.8 | 46.7 | 55.9 | |
| P-value | 0.014* | 0.145* | |||
| Interaction with health service providers | |||||
| Through school health services | 86.4 | 70.0 | 48.6 | 46.7 | |
| From health facility | 13.6 | 13.3 | 34.3 | 33.3 | |
| Through media | 0 | 13.3 | 14.3 | 20.0 | |
| Other specify | 4.5 | 3.3 | 2.9 | 0 | |
| P-value | 0.337 | 0.756 | |||
| IHS important in shaping sexual health | |||||
| Yes | 60.7 | 54.2 | 48.9 | 35.4 | |
| No | 39.3 | 45.8 | 51.1 | 64.6 | |
| P-value | 0.579 | 0.182* | |||
| MHS being important in shaping sexual health | |||||
| Yes | 67.9 | 83.3 | 66.0 | 57.4 | |
| No | 32.1 | 16.7 | 34.0 | 42.6 | |
| P-value | 0.118* | 0.125* | |||
| Activities at initiation schools | |||||
| Sexual education | 11.1 | 27.5 | 40.0 | 14.0 | |
| Circumcision | 28.6 | 20.0 | 12.5 | 11.6 | |
| Vaginal modifications | 23.8 | 2.5 | 17.5 | 20.9 | |
| Other | 33.3 | 50.0 | 30.0 | 53.5 | |
| P-value | 0.033* | 0.056* | |||
| Do these activities influence your decision to engage in sexual activities | |||||
| Yes | 29.6 | 26.3 | 44.2 | 22.5 | |
| No | 70.4 | 73.7 | 55.8 | 77.5 | |
| P-value | 0.769 | 0.045* | |||
| Encountered any challenge | |||||
| Yes | 10.7 | 13.8 | 12.5 | 8.8 | |
| No | 89.3 | 86.2 | 87.5 | 91.2 | |
| P-value | 0.723 | 0.612 | |||
| Health education | |||||
| Yes | 82.1 | 54.2 | 68.1 | 59.6 | |
| No | 17.9 | 45.8 | 31.9 | 40.4 | |
| P-value | 0.014* | 0.391 | |||
| Interaction with health service providers | |||||
| Through school health services | 82.6 | 70.0 | 48.6 | 46.7 | |
| From health facility | 13.0 | 13.3 | 34.3 | 33.3 | |
| Through media | 0 | 13.3 | 14.3 | 20.0 | |
| Other specify | 4.3 | 3.3 | 2.9 | 0 | |
| P-value | 0.337 | 0.214 | |||
| IHS important in shaping sexual health | |||||
| Yes | 60.7 | 54.2 | 48.9 | 35.4 | |
| No | 39.3 | 45.8 | 51.1 | 64.6 | |
| P-value | 0.579 | 0.182* | |||
| MHS being important in shaping sexual health | |||||
| Yes | 67.9 | 83.3 | 64.6 | 57.4 | |
| No | 32.1 | 16.7 | 33.3 | 42.5 | |
| P-value | 0.118* | 0.396 | |||
3.4. Multiple Logistic Regression Analysis
3.4.1. Factors Influencing the Prevalence of STIs
A total of four factors were found to influence STIs' prevalence in Mberengwa (Sex of Respondent, Tribe and Sexual Encounter) and Umguza (Pregnant or Impregnated, Sex of Respondent). Respondents from the Lemba tribe were 98 times more likely to suffer from STIs than other tribes. These findings are presented in Table 5.
Table 5.
| Outcome Prevalence of STIs | |||||||
|---|---|---|---|---|---|---|---|
| Mberengwa | Umguza | ||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Pregnant or Impregnated | No | *** | |||||
| Yes | 31.9 | 2.3-451.4 | 0.010* | ||||
| Sex of Respondent | Male | *** | *** | ||||
| Female | 3.3 | 1.2-16.4 | 0.041* | 15.2 | 1.9-78.2 | 0.050* | |
| Tribe | Xhosa | *** | |||||
| Ndebele | 2.1 | 0.1-56.8 | 0.669 | ||||
| Lemba | 97.6 | 2.0-4718.7 | 0.021* | ||||
| Shona | 7.6 | 1.4-157.0 | 0.191 | ||||
| Other | 1 | ||||||
| Sexual Encounter | I wanted to have sex | *** | |||||
| My partner wanted us to have sex | 0.8 | 0.1-4.7 | 0.807 | ||||
| It just happened | 3.2 | 1.4-65.2 | 0.047* | ||||
| I was culturally obliged to | 1 | ||||||
| Other | 1 | ||||||
3.4.2. Factors Associated with the Prevalence of Pregnancies or Impregnating
A total of five predictors influenced the prevalence of pregnancies and impregnation in these two districts. In Umguza, females were 51 times more likely to get pregnant, while in Mberengwa, the females were five times more likely to get pregnant. In Umguza, religion influenced pregnancies; those in Pentecostal churches were eight times more likely to be pregnant or impregnated than those who were not subscribed to any religion. These findings are presented in Table 6.
| Outcome Pregnancies/Impregnated | |||||||
|---|---|---|---|---|---|---|---|
| Mberengwa | Umguza | ||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Gender | Male | *** | *** | ||||
| Female | 4.8 | 1.5-27.9 | 0.031* | 50.7 | 5.7-2790.0 | 0.000* | |
| Tribe | Xhosa | *** | |||||
| Ndebele | 2.4 | 2.1-48.3 | 0.045* | ||||
| Lemba | 1 | ||||||
| Shona | 3.2 | 1.8-51.3 | 0.021* | ||||
| Other | 1 | ||||||
| Sexual Encounter | I wanted to have sex | *** | |||||
| My partner wanted us to have sex | 1.26 | 0.23-2.5 | 0.082 | ||||
| It just happened | 2.4 | 1.5-15.3 | 0.041* | ||||
| I was culturally obliged to | 4.3 | 2.1-45.3 | 0.021* | ||||
| Other | 1 | ||||||
| Age | <10 | *** | |||||
| 10-12 | 1 | ||||||
| 13-17 | 2.5 | 1.9-22.7 | 0.041* | ||||
| 18-19 | 1 | ||||||
| Religion | None | *** | |||||
| Catholic | 1 | ||||||
| Protestant | 1.3 | 0.0-56.2 | 0.982 | ||||
| Pentecostal | 8.2 | 2.3-1492.0 | 0.040* | ||||
| Other | 0.2 | 0.0-16.2 | 0.470 | ||||
| Districts | Had STIs n (%) | Did not Have STIs n (%) |
χ2 p-value |
Hazard Ratio | 95% CI | P-value |
|---|---|---|---|---|---|---|
| Mberengwa | 25 (6.8) | 345 (93.2) | 0.04* | *** | ||
| Umguza | 38 (10.6) | 322 (89.4) | 1.25 | 1.05-2.73 | 0.043* | |
| Districts | Pregnant or Impregnated n (%) |
Did not Impregnate or get pregnant n (%) |
χ2 p-value |
Hazard Ratio | 95% CI | P-value |
| Mberengwa | 26 (7.0) | 344 (93.0) | 0.043* | *** | ||
| Umguza | 45 (12.5) | 315 (87.5) | 1.20 | 1.01-1.92 | 0.034 | |
| Districts | Had Sex n (%) | Did not have Sex n (%) |
χ2 p-value |
Hazard Ratio | 95% CI | P-value |
| Mberengwa | 75 (20.3) | 295 (79.7) | 0.038* | *** | ||
| Umguza | 96 (26.7) | 264 (73.3) | 1.85 | 1.04-3.08 | 0.040* | |
3.5. Differences in the Two Districts
3.5.1. Cox Regression-Breslow Method of Ties
There were significant differences in STIs prevalence, impregnation, and sexual activity engagement in the two districts. Adolescents in Umguza were 1.25 times more likely to have STIs, 1.2 times more likely to be pregnant /impregnated, and 1.85 times more likely to engage in sexual activities than those in Mberengwa District. These findings are presented in Table 7.
3.5.2. Kaplan-Meier Survival Estimates
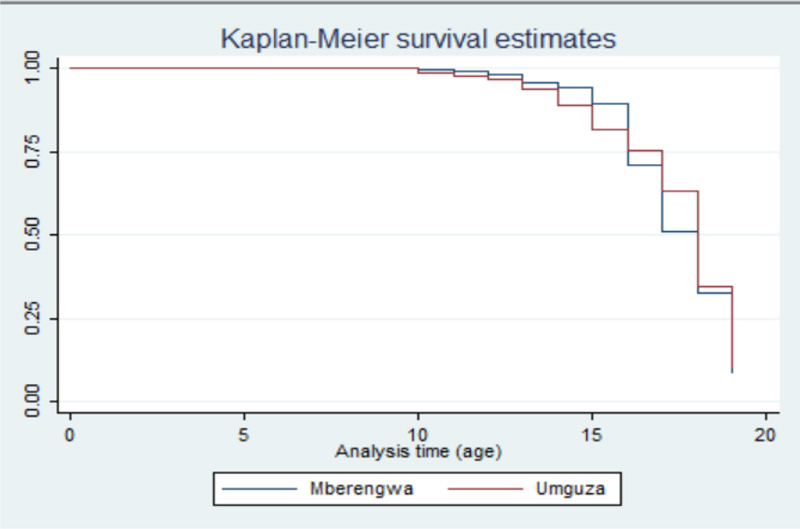
3.5.2.1. Engagement in Sexual Activities
Age at first sex was lower in Umguza compared to Mberengwa though more adolescents in Mberengwa get involved in these activities around 16 years and above in huge numbers. The remaining majority get involved at 19 years. These findings are presented in Fig. (2).
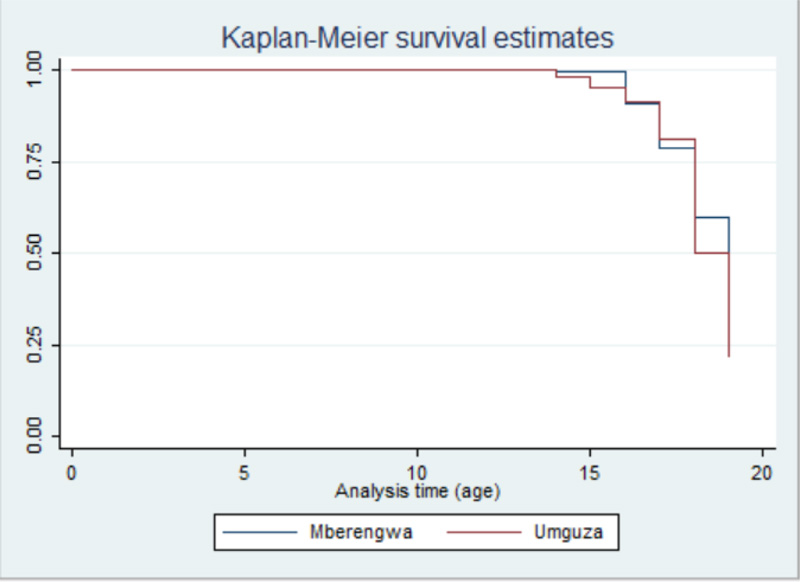
3.5.2.2. Getting Pregnant or Impregnating
There is not much difference when comparing ages and pregnancies in the two districts, with the majority peaking towards the 19-year mark. These findings are presented in Fig. (3).
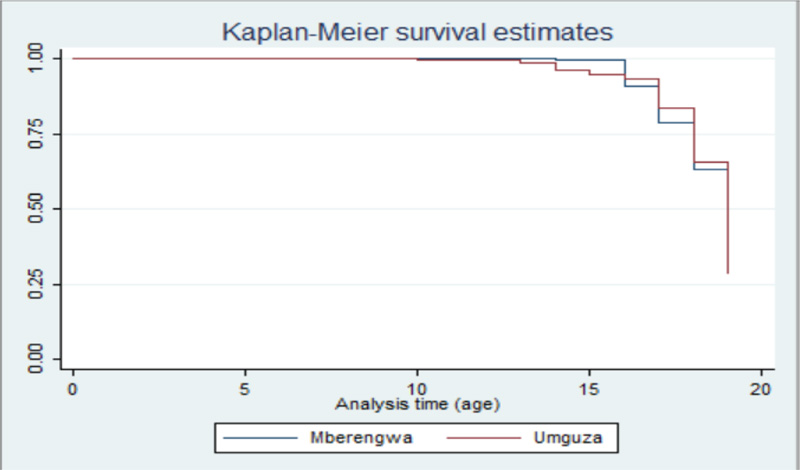
3.5.2.3. Prevalence of STIs
STIs at Umguza are detected early (around 13) compared to Mberengwa, which starts approximately at the age of 15. In both the districts, it peaks towards the 19-year mark. These findings are presented in Fig. (4).
4. DISCUSSION
The sex of respondents significantly contributed to engagement in sexual issues, with females engaging in sexual intercourse at an earlier age than male adolescents in both districts. The age at first sex in females was lower than that of males. These findings are anchored by different studies that reported similar outcomes and allude that most female adolescents mature earlier than their male counterparts. They thus usually engage in sexual activities earlier [34, 35]. This also puts them at risk of pregnancies and high STI prevalence, as reported in this study, compared to their male counterparts. Studies report that cross-generational sex usually involves young female adolescents and older men than young male adolescents and older females [36]. Therefore, this predisposes females to STIs and pregnancy more than male adolescents [36].
Religion was reported to influence the prevalence of pregnancies/impregnation in Umguza compared to Mberengwa, where this variable was insignificant. It was observed that respondents attending Pentecostal churches had higher chances of getting pregnant than those who did not participate in any church activities. In Zimbabwe, there is an influx of different Pentecostal churches that have been blamed for poor ethos as they are doctrine to make money from the congregants [37]. Sexual abuse has been reported among different members, particularly females, in these churches [38].
Another significant predictor variable was the nature of sexual encounters and the prevalence of STIs and pregnancies /impregnating. Those who were culturally obliged and claimed that sex just happened were at a higher risk of being pregnant in Mberengwa than those who claimed they wanted to have sex. Usually, sex happens unplanned, most of the time. In that case, proper preventive measures, such as using condoms, are forgone as there would, in most cases, be unavailable at that time and point [39]. Studies suggest that in planned sexual encounters, individuals prepare themselves upfront and go to all extents necessary to protect themselves. They would have enough time and opportunity to plan [39]. Adolescents who are culturally obliged to have sex might not have any decision-making power; everything is detected to them by those in that marriage [39]. Therefore, this leads to a scenario where they have no say and would have sex according to how the other dominant spouse prescribes it [40].
It was also observed in the study that the prevalence of STIs, pregnancy/impregnation, and the number of adolescents who had sex were higher in Umguza as compared to Mberengwa. One of the potential reasons is that in Umguza as a district, a significant number of parents or guardians migrate to neighbouring countries like Botswana and South Africa as the district is in region five, where there are deficient rainfall and farming is not lucrative as compared to Mberengwa, which receives a significantly higher amount of rain compared to Umguza [41]. This leaves many homesteads child-headed and losing control, particularly if the parents and guardians are not consistently sending resources for upkeep [42]. This is also well supported by the findings that a significantly higher proportion of adolescents in Umguza drop out of school because of a lack of resources to pay fees and survive. They are then forced to look for ways to sustain their livelihoods [42].
4.1. Limitations of the Study
The study was conducted in two districts, i.e., Umguza and Mberengwa in Zimbabwe. The findings were, therefore, contextual to these study districts and might be difficult to generalise for other districts in the country due to differences in cultural setups and other settings.
CONCLUSION
The two districts have a significantly higher prevalence of having sex than the national average. Adolescents are at risk of contracting STIs and impregnation as they engage in risky sexual behaviours as evidenced by the findings. Therefore, there is a need to craft policies and programs to eliminate these risky sexual behaviours that predispose adolescents to poor SH outcomes.
AUTHORS' CONTRIBUTIONS
WNN conceptualised the research as partial fulfillment of the Ph.D. requirements. LM was the supervisor of these Ph.D. studies, while JTM and RTL were core supervisors. The three contributed by guiding the Ph.D. student in conceptualisation, research, and manuscript preparation. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was sought from the University of Venda's Ethics Clearance Committee (Ethics Number: SHS/19/PH/17/2608) and the Medical Research Council of Zimbabwe (Ethics Clearance number: MRCZ/A/2611). Permission to conduct the study was also sought from the Ministry of Health and Child Care and the Ministry of Education if respondents were to be followed up at schools. Permission to conduct the study in the specific districts was sought from traditional leaders (Traditional chiefs and headmen).
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. This research was conducted following the Nuremberg code and principles stated in the Helsinki Declaration for studies involving human participants.
CONSENT FOR PUBLICATION
Written consent was sought from all respondents. Since data were also collected from adolescents (some of whom were under the age of 18), written “consent” was sought from their parents / legal guardians and adolescents themselves “assented” to be part of the study. Information sheets and assent forms were provided for participants to read and sign if they agreed to be part of the study.
STANDARDS OF REPORTING
STROBE guidelines have been followed.
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of this study are available within the article.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
FUNDING
The research was funded by the National University of Science and Technology under the Staff Development Programme.
ACKNOWLEDGMENTS
Declared none.


