All published articles of this journal are available on ScienceDirect.
Internet of Medical Things – The Future of Healthcare
Abstract
Background:
The Internet of Medical Things (IoMT) is now being connected to medical equipment to make patients more comfortable, offer better and more affordable health care options, and make it easier for people to get good care in the comfort of their own homes.
Objective:
The primary purpose of this study is to highlight the architecture and use of IoMT (Internet of Medical Things) technology in the healthcare system.
Methods:
Several sources were used to acquire the material, including review articles published in various journals that had keywords such as, Internet of Medical Things, Wireless Fidelity, Remote Healthcare Monitoring (RHM), Point-of-care testing (POCT), and Sensors.
Results:
IoMT has succeeded in lowering both the cost of digital healthcare systems and the amount of energy they use. Sensors are used to measure a wide range of things, from physiological to emotional responses. They can be used to predict illness before it happens.
Conclusion:
The term “Internet of Medical Things” refers to the broad adoption of healthcare solutions that may be provided in the home. Making such systems intelligent and efficient for timely prediction of important illnesses has the potential to save millions of lives while decreasing the burden on conventional healthcare institutions, such as hospitals. patients and physicians may now access real-time data due to advancements in IoM.
1. INTRODUCTION
A fundamental aspect of human rights is access to high-quality medical care, yet it is not widely available. The world's economic, environmental, and social progress, as well as the accompanying lifestyle, have been linked to an alarming rise in the prevalence of long-term ailments such as cardiovascular illness, leukemia, and diabetes. These prolonged diseases represent the biggest risk to the well-being of humans. Furthermore, if an infectious illness spreads, it will cause an overwhelming number of individuals to seek medical treatment, putting more pressure on healthcare services. For example, the fast transmission of COVID-19 is currently putting stress on the world's healthcare resources. This type of situation results in ineffective patient and data management [1]. Nowadays, the healthcare and advanced technology sectors [2, 3] have taken on important roles in daily life, including healthcare systems [4]. The primary purpose of using modern technology in medicine is to make it easier for patients and doctors to talk to each other. This will improve the effectiveness of medical devices and services and make them easier to access [5-9].
The IoMT is a subpart of the IoT, where the IoT deals with communication and always-on connectivity between devices, called things. Specifically, when these things relate to the medical industry, such as dosimeters, pulse oximeters, etc., then the IoT is renamed the IoMT [10].
IoMT refers to the use of mobile computing, medical sensors, and cloud computing to monitor patients' vital signs in real-time and the use of communication technologies to relay data to a cloud computing framework. The data can be accessed by physicians to monitor, diagnose, and treat patients effectively. The Internet of Medical Things combines the dependability and safety of conventional medical equipment. It is general enough to cope with a range of illnesses that ask for extremely diverse monitoring and actuation needs, and it has the capacity to handle several devices that are deployed for numerous patients. This gives it the power to tackle the issue of aging and chronic illnesses.
Currently, IoMT [11-13] is already performing an essential function in remote healthcare monitoring (RHM) [14, 15]. The Internet of Medical Things (IoMT) is a term that refers to the fusion of the Internet of Things with healthcare technology (IoT). The spread of personal computing devices, along with advances in technology, allows the establishment of the Internet of Medical Things (IoMT), which offers solutions to address the needs of both our growing elderly populace as well as patients who suffer from chronic diseases. The Internet of Medical Things is the network that connects not only a large number of individual medical devices but also equipment and organizations that offer medical services, such as hospitals, medical research facilities, and private businesses. The rise of the IoMT is primarily attributable to an increase in the usage and development of linked and distributed medical devices, which has resulted in the emergence of both potentially advantageous applications [16].
IoMT belongs to intelligent and electronic medical devices that are able to gather, monitor, and improve patients' health problems in real time, all while doing so at a lower cost. Wearable technology includes fitness trackers, smart health watches, wearable blood pressure monitors (BPM), ring-type heart rate monitors, and biosensors. Wearable gadgets are designed to be worn on the body [17].
IoMTs are the future of healthcare systems. As it develops, it delivers faster and less expensive health care [18]. The Internet of Things (IoT) is mostly utilized to gather remote information for patients via wearable sensors/devices [19] and save it in cloud databases. This information is made available to caregivers for real-time analysis and use [20]. The Internet of Medical Things is composed of three distinct stages: the device layer (also known as the body sensor network or BSN), the cloud service layer, and the fog layer [21] shown in Fig. (1).
The sensor data is collected by BAN and sent to a gateway node. The information is stored as well as analyzed by the transmission layer using the threshold values that are standard to indicate any anomalies. Furthermore, the information might be sent up into the cloud, where it would be stored and subjected to extensive computations. Doctors and other medical professionals can use an online portal to log in, check and confirm diagnoses, and take the right steps.
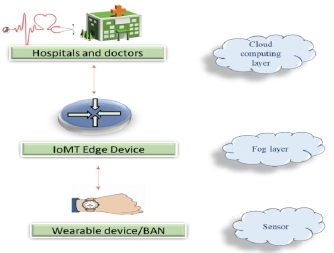
According to the information presented above, the design of the system is ineffective in crisis management owing to the high delay in outcomes. The cloud receives data from BAN sensors on patients' health for further analysis. This raises the total latency of the system, and patients in emergency situations cannot receive a quick analysis. This latency issue is being solved by the emerging fog and edge computing paradigms [1]. At a fog layer, a system of emergency alarms is set up with specific threshold values for the different metrics that are being watched.
It has been found that while measuring environmental factors only needs a fixed system, measuring physiological variables needs continuous data analysis [22]. RHM [23-28] is a continuous health data monitoring technique. This comprises physiological monitoring, physical activity, nutrition monitoring, medication tracking, and behavior observation. Cloud computing allows for the wireless transmission of health-related information to both patients and medical professionals [29, 30]. As a result, IoMT enables real-time, quick, remote, and reliable illness detection and improves decision-making. A huge quantity of data is gathered, evaluated, and monitored during this process [31].
With today's hectic lifestyle, the majority of individuals do not undergo routine medical check-ups. Furthermore, healthcare costs are growing, and each year, governments pay a large sum of money to cover the cost of providing healthcare services. In order to overcome all of these challenges, there is a large need for healthcare monitoring that is performed remotely and in real time [32-34].
1.1. IOMT (Internet of Medical Things) WORKING
The majority of IoMT systems operate in the following key layers, which incorporate a vast range of technologies, devices, and sensors that are linked to one another by means of wired or wireless connections [35, 36].
Data sources such as health monitoring gadgets and mobile applications are incorporated with sensors, including infrared sensors, medical sensors, radio frequency identification (RFID) cameras, and sensors are included in the perception layer, which is the lowest stratum of the IoMT (GPS). The sensing systems detect changes in their surroundings, identify objects, locations, demographics, and magnitudes, and then convert this data into computerised data using the assistance of dependable, wired or wireless network communications that serve as a higher-performance transport medium.
1.2. Gateway Layer
As was stated earlier, the sensors need communication with the gateway in order to function properly. This connectivity must be created using networks that are capable of sharing and keeping information centralized. The transmission may take place across a wide range and could have a very short or relatively long range. Examples of short-range communication include radio frequency identification (RFID), Zigbee, and Wireless Fidelity. Examples of wide-range communication include cloud computing, blockchain technology, and so on [37].
Many kinds of gateways are listed below Fig. (2).
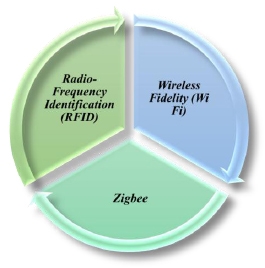
1.2.1. Radio-Frequency Identification (RFID)
It includes a microprocessor as well as an antenna that is able to detect a particular object in the environment, as well as a user that communicates with the tag through radio waves to send or collect information as an electronic product code (EPC).
1.2.2. Zigbee
It has a mesh network structure, enabling integrated, uninterrupted data transfer among medical devices. It ensures information distribution continues even when some of the devices are not functioning properly. The frequency range of Zigbee is comparable to that of Bluetooth (2.4 GHz), but the communication range is substantially greater. It is made up of routers, end nodes, and a processing centre, all of which allow for the aggregation and analysis of data. Zigbee has low power consumption, in addition to a high transfer rate and capacity for the network.
1.2.3. Wireless Fidelity (Wi Fi)
It is a wireless local area network (WLAN) with a longer range of transmission. It is a popular gateway mode used in hospitals due to its quick and effective network construction capacity, increased smartphone compatibility, and provision to enable strict control and security. However, the primary limiting factors are considerably greater power consumption and network instability.
1.3. Management Service Layer
The processing of massive amounts of raw data in order to extract meaningful data necessitates the use of tools that comprise the management service that may function at a faster rate employing analytics, safety precautions, process modelling, and device monitoring.
For secure communication, the Secure Sockets Layer Application Programming Interface (SSL API) is used. It makes it possible to collect information, such as detailed electronic medical records (EMRs), from a patient's sports, the Internet of Medical Things, and smartphone tools. This information is then sent to the cloud, where it can be used to help make decisions about treatment interventions [38].
1.4. Application Layer
The analysis of the information and the delivery of application-specific services are the two primary responsibilities of the application layer. The application layer makes use of artificial intelligence (AI) and deep machine learning to analyze EMR data and to monitor changing patterns in the obtained data using a number of daily and weekly plots in order to provide decisions regarding possible diagnoses and treatments.
2. IOMT IMPACTING HEALTHCARE
There are a variety of ways in which IoMT influences the healthcare industry. These changes are most readily apparent when putting IoMT into practice at home, on the body, in the community, or within a hospital [39] (Fig. 3).
2.1. In-home IoMT
People are capable of transmitting health information from their houses to other locations, such as their primary care providers or hospitals, using a technology called (IoMT).
For example, remote patient monitoring (RPM) is the use of healthcare tools to communicate data such as blood pressure or oxygen levels from recently released patients to their hospital for assessment through their physicians. This may help to prevent hospital readmissions by identifying problems before they become critical.
When it comes to delivering continued therapy outside of the patient's surroundings, the use of IoMT devices in combination with telehealth may also prove to be advantageous. Personal emergency response systems (PERS), for instance, have the ability to detect potentially life-threatening events like cardiac arrest and immediately contact emergency personnel.
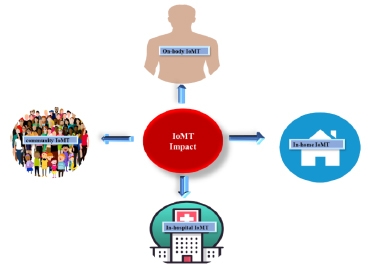
2.2. On-body IoMT
On-body consumer IoMT devices are wearable devices to measure health indicators for personal use as well as share them with healthcare practitioners. These devices may be purchased by anybody and are available for purchase online. These devices are not only able to monitor a conventional metric, such as heart rate, but they also have the potential to serve as early warning indicators for health problems that are more serious in nature. For example, the Apple Watch can alert users of abnormal cardiac rates.
2.3. Community IoMT
It is the usage of IoMT technologies in a larger geographical region. Mobility services, for example, are tools that monitor patients while they are travelling in a vehicle. In the same way, first responders and paramedics use emergency response intelligence systems to keep track of patients' information outside of hospitals.
Community IoMT includes techniques that allow medical care to be given remotely, in addition to on-site and emergency care.
2.4. In-hospital IoMT
Hospitals must maintain the quality and availability of their medical resources throughout time, as well as understand how workers and patients move across the facility. Healthcare personnel utilise IoMT sensors and other monitoring devices to record all of these interactions so that administrators get a complete view of what is happening.
3. IOMT IN THE HEALTHCARE SYSTEM USES A BROAD RANGE OF SENSORS
Medical tools are widely accessible, but they are expensive as well as use a large amount of electricity. As a result, sensors are used in IoMT-based healthcare systems in order to preserve power and create solutions that are both low-cost and economical.
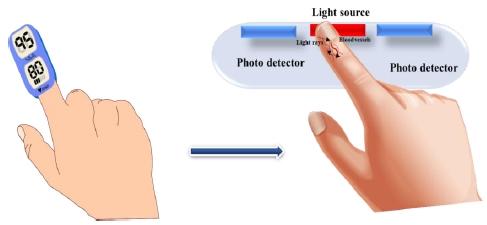
3.1. Pulse Oximeters
It is a tool that does not require the patient to undergo any invasive procedures in order to check their blood oxygen saturation. Such data may be applied to measure the health of a patient and discover any abnormalities that may be present. Conditions such as asthma, pneumonia, anaemia, and other lung-related disorders, as well as other conditions, may be detected using a blood oximeter. In clinical applications, the pulse oximetry technique has been shown to be an advantageous characteristic for assessing oxygen saturation. SpO2 is often detected using a sensor connected to the patient's finger. There are two methods for measuring SpO2: transmissive and reflected. The transmissive approach is the more prevalent of the two. Such pulse oximeters work by sending light through the blood in the finger and then analysing differences in light penetration in oxygenated or deoxygenated blood to determine the oxygen saturation in the blood (known as the SpO2 level) (Fig. 3).
MAX30102, invented by Maxim Integrated, is the most extensively utilized pulse oximeter sensor [40].
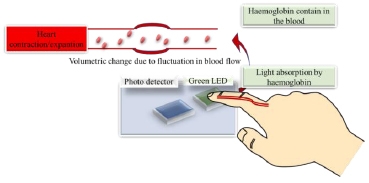
3.2. Pulse Rate Sensors
The rate of the patient's pulse is observed in order to evaluate the state of the patient 's heart. In the event of a crisis, it may be utilized to pinpoint the source of the problem immediately. APDS-9008 is the pulse rate sensor that is used by the greatest number of people. In order to put it to use as a sensor for determining the rate at which the heart is beating, a green infrared LED with low intensity is employed to identify the pulse via the reflection of light that occurs in each heartbeat [41] (Fig. (4).
3.3. ECG Sensors
To check proper heartbeat and strength, electrocardiogram (ECG) data is essential. It is vital in the detection and management of heart disease. The AD8232 is a popular ECG measuring module that may be used in a variety of applications, such as a heartbeat sensor, as well as a sensor for the ECG, which means that it serves various functions and is thus extensively utilized. The front end of the device may make use of it as a heartbeat sensor. The system incorporates a rapid circuit restoration capability that decreases the amount of waiting time caused by the high pass filter's low cut-off frequency. It also provides an ECG Android app via which users may examine their data for health monitoring reasons [42].
3.4. Blood Glucose Monitor
Patients diagnosed with diabetes are required to make use of blood glucose monitors in order to maintain adequate control over their blood sugar levels. On the market nowadays, one may choose from a number of different blood glucose monitors. They are desirable in an IoT environment [43]. It emphasises the problems of invasive blood glucose monitoring as well as the possibility of contamination from used needles, which might result in infections. With that in mind, their recommended solution is to design a non-invasive blood glucose level measuring tool. The sensor kit for these monitors includes an infrared LED, a photodiode, and an AT-MEGA328 microprocessor. IR radiation is used in this device to measure blood glucose levels. Furthermore, several systems have smart alerting functions that may notify the patient if an abnormality is identified [44]. iGLU is another system. Using an Intelligent Glucose Meter Using near-infrared spectroscopy and machine learning algorithms, this system analyses the data acquired from patients and identifies any irregularities that may be present in that data. These characteristics enable endocrinologists to remotely monitor the patient [45].
3.5. Temperature Sensors
The LM-35, TMP236, DS18B20, and MAX30205 are the temperature sensors that are used the most frequently. The DS18B20 is used to determine the patient 's body temperature in a wearable patient monitoring device. The MAX30205 temperature sensor not only gives an exact reading of the temperature but also acts as an overtemperature alert. The MAX30205 is suited for wearable devices because of its high precision and low operating voltage. Furthermore, its digital capabilities facilitate integration with any system.
The LM-35 is most typically employed in wearable sensor networks. It has a huge temperature range compared to the DS18B20 [46].
3.6. Electromyography Sensor
The Electromyography Sensor, often known as an EMG, is used for the purpose of determining the electrical impulses of the muscles. With the help of this sensor, physicians and other medical experts are able to track nerve and muscle abnormalities in their patients. These sensors are also utilised in devices that are worn by the patient in order to monitor their behaviour. EMG sensors are essential to the development of emotion-based intelligent information sensing systems. These systems use EMG signals in conjunction with other biomedical sensors in order to identify fluctuations in facial muscles and associate each variation with its associated emotion. This approach can identify the patient's impacted condition of health. Advancer Technologies is also developing an Arduino-powered EMG sensor on the market [47].
3.7. Blood Pressure Sensors
Significant research has been conducted on non-invasive methods of measuring blood pressure, such as the modern technique known as the oscillometric method [48], which involves compressing blood vessels with the help of an air-inflated cuff in order to obtain readings of systolic and diastolic pressure. The alternative method involves estimating a patient's blood pressure without the use of a cuff. This process is based on many types of biomedical sensors, such as ECG and PPG sensors. Advances in research and study in ECG and PPG signal analysis have resulted in the creation of a system for estimating and evaluating patients blood pressures. Such an approach is advantageous in the long term since it lowers the system's hardware expenses and makes the patients more comfortable [49].
4. APPLICATION OF IOMT IN THE HEALTH CARE SYSTEM
4.1. The Sensor Patch Detects Blood Leakage during Hemodialysis
A new system that utilizes Bluetooth Low Energy (BLE) and Wi-Fi, integrating it with IoMT (Internet of Medical Things) technologies to create a sensor patch This system was made up of a multi-ring-shaped sensor. As the volume of liquid increased, the sensor was able to identify leaks. Additionally, the device had a mapping circuit as well as a Bluetooth low energy module. During manufacture, a signal line was included in the insulating layers; however, the only part of the array that was open to the environment was the sensing point. The following three phases comprised the technique from blood leaking to detection: (1) absorption, in which the gauze absorbed the blood, which then diffused to the patch; (2) reaction, in which the blood diffused into the patch, which caused the detection voltage to rise; and (3) saturation, in which the blood could no longer spread and the voltage remained stable [50].
4.2. Smart Medication for High Blood Pressure
Digital (smart) drugs with integrated IoMT sensors in each tablet may be utilised to assess antibiotic concentrations in bodily fluids and dose tracking will offer more accurate data on treatment effectiveness on a personalized basis [51]. Naik et al. also showed the usage of an ingestible sensor that was designated with a CE-mark in order to evaluate individuals with chronic high blood pressure [52].
4.3. Digital Biomarkers
Diagnostic tools that are self-powered and linked to the IoMT are currently being developed. These tools have the potential to enable real-time monitoring of biomarkers in bodily fluids such as sweat, urine, blood, and so on. Because of this, it may be easier to distinguish between illnesses caused by bacteria and those caused by viruses. This can be very useful. In addition, the patients' response to therapy may be carefully tracked. This would indicate whether or not the patients is actually responding to therapy and could possibly indicate that resistance is present. [53-63, 37]
Wessels et al. (2021) used complicated neural networks to make a new smart biomarker that can find lymph node metastasis [64].
4.4. Disease Surveillance and Tracking
Testing and tracking are the primary concerns for disease spread management over the globe, especially in order to slow transmission. Several different devices that are based on IoMT have been put to use in order to test and track people who are infected with the illness, as well as to identify the location of patients in order to track the possibility of disease transmission. Infectious disorders such as malaria, dengue fever, influenza A (H1N1), human papilloma virus, Ebola virus disease, Zika virus and coronavirus (COVID-19) may be treated more effectively with the use of point-of-care testing (POCT) devices that are based on IoMT [37] shown in Fig. (5).
Bibi et al., 2020, established an IoMT-based system that allowed for real-time testing that was both fast and secure, as well as the diagnosis and management of leukaemia using cloud computing [65].
4.5. Stress and Anxiety Monitoring
Stress and anxiety problems are becoming more widespread in today's society. Poor stress management may result in stress disorders, psychological anguish, and physical diseases. According to preliminary studies, people who recovered from COVID-19 experienced an increase in anxiety problems and other mental illnesses. It is a low-cost anxiety disorder monitor based on IoT that extracts emotion characteristics from physiological measurements in a semi-immersive environment. The data on a user's heart rate and physical activity is gathered by an Internet of Things node and then sent to a Raspberry Pi 3 for preprocessing before being uploaded to an Internet of Things cloud. The results of this system's validation showed that it had an accuracy rate of 90 percent in recognizing anxiety disorders [66].
4.6. Seizure Detection
A seizure is a rapid electrical disruption that occurs in the brain. As a result, it is of the utmost importance to recognize or detect it in a timely manner in order to give appropriate care and therapy to the patients.
An IoMT-based approach may detect seizure onset using a patient's electroencephalography (EEG) data. The system analyses neurological data obtained from an EEG sensor and continually processes it in order to extract hyper-synchronous pulses from the brain. Such information collection is then utilized to identify seizure incidence [67].
4.7. Wearable Ozone Therapy
Ozone treatment has a distinct benefit due to its simplicity of creation. Ozone may be artificially created (through UV-light) within small portable units carried by the patients, providing for low-dose continuous therapy regimens while minimizing the negative impacts of increased concentrations on normal skin cells [68]. Ozonated air promotes wound healing by subjecting the wound to oxidative stress, which in turn causes a rise in the generation and migration of wound healing components as well as an increase in the amounts of oxygen at the wound site [69]. A wearable ozone production technology would enable patients to get ozone therapy topically outside of a clinical environment. Design, manufacturing, and testing of a portable and wearable platform administer ozone to the wound site locally.
4.8. Aerial Thermal Scanners
Tele-thermographic systems (TIS) contain an embedded thermal infrared camera with a temperature reference that is able to correctly determine an individual's skin temperature without making any kind of direct physical contact with that person. These easy-to-use technologies that don't need any intervention are quite helpful for detecting elevated body temperatures in heavily crowded locations. Mohammed et al. (2020) used thermal images to detect elevated temperatures associated with coronavirus infection utilising an IoMT-based drone technology [70].
4.9. Automatic Insulin Injection
The Raspberry-Pi 3 is used, which is not only inexpensive but also versatile. Information about four of the body's vitals is gathered and shown on the website with a camera that streams live video in order to do a continual examination. For the purposes of live monitoring, there are two different login keys: one is reserved for the physician, and the other is given to the patient's relatives. A message is provided to the physician through the GSM module whenever a sensor detects any instability or abnormality. When physicians see that insulin injections are necessary, they may do it from anywhere by pressing a button, which enables the release of a limited dosage of insulin into the patients [1].
5. IOMT SECURITY AND PRIVACY
Security and privacy issues are now one of the most significant difficulties that Internet of Things (IoT) systems are currently facing. According to the Federal Bureau of Investigation (FBI), present IoMT tools are very susceptible to exploitation because of inadequate verification and obsolete technology. In recent years, the IoMT has been at the forefront of cyber-attacks. According to surveys, approximately 90% of healthcare firms that use IoT have reported at least one security problem. According to another survey, around 35% of the over 370 firms that use IoMT had at least one cybersecurity breach in 2016. In 2018, hackers locked up medical information about patients at an Indiana hospital. The hospital had to pay a lot of money to get the information back [71].
A smartcard-based user-controlled single sign-on (SC–UCSSO) system was suggested by Lin et al., 2021 for use in telemedicine. This system helps maintain patients' privacy while also improving security and reliability [72, 73].
“CoviChain” makes use of the technology known as blockchain to solve the problems with data security and privacy, as well as to prevent the disclosure of personal information about people while increasing the amount of data that can be stored [74].
CONCLUSION
The nation's healthcare systems are now struggling with issues such as staffing shortages among essential medical experts, extended wait times, an increase in the demand for services, and limited financial resources. The Internet of Medical Things, often known as IoMT, is a paradigm shift in the healthcare business that has been put into place to improve medical services, lower the cost of those services, extend life expectancy, and achieve a number of other related goals. The development of technologies like cloud computing, fog computing, edge computing, and artificial intelligence has helped to accelerate the adoption of IoMT while also making it more secure. A significant improvement has been made to the healthcare system as a result of the development of remote health monitoring and smart gadgets, telemedicine, wearable ozone treatment and sensor patches. These innovations provide a significant contribution to the prevention of sickness by enabling testing, early identification, and treatment. IoMT enables medical apparatus and products to show real-time data to doctors on the status of the patient. If IoMT is going to exist or rise smart hospitals, we are going to need a serious standardisation policy in the industry to effectively implement this.
LIST OF ABBREVIATIONS
| IoMT | = Internet of Medical Things |
| RHM | = Remote Healthcare Monitoring |
| POCT | = Point-of-care testing |
| RFID | = radio frequency identification |
| EPC | = electronic product code |
| WLAN | = wireless local area network |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
I am grateful to the pharmacy faculty at PSIT for motivating me to write this review article.


