All published articles of this journal are available on ScienceDirect.
Knowledge, Attitude, and Practice Towards Sexually Transmitted Infections Among Women of Reproductive Age in an Urban Community Health Centre in Indonesia
Abstract
Introduction:
Sexually transmitted infections (STIs), an emerging public health burden, are increasing due to a lack of understanding about their prevention.
Objective:
To understand the association between STI-related knowledge, attitudes, and practices (KAP) among women of reproductive age in an urban community health centre in Jakarta, Indonesia.
Material and Methods:
A cross-sectional study and consecutive sampling technique were employed on 50 women using a structured, self-administered questionnaire. All data were analysed using Spearman’s rank correlation, χ2, or Fisher’s exact test to test the hypothesis.
Results:
Encountered women had an average age of 26.80 ± 4.64 years, were married (74%), primiparous (46%), and with a high level of education (88%). The median scores for attitude and knowledge were 76.90 and 79.20, respectively, and there was a moderate correlation between these scores (ρ=0.482, p<0.001). Overall, 84% of individuals had good knowledge, and 88% of respondents had a positive attitude. Practical insight was moderate, with the rate of abstinence, using condoms, suggesting condoms, and stigmatising persons with HIV/AIDS being 54%, 32%, 2%, and 36%, respectively. Education level was a significant predictor of knowledge, and women’s attitudes toward STIs were associated with their knowledge (OR 7.80, p=0.044). There was no relationship between socio-demographic profiles and the KAP of STIs. Knowledge and attitude did not contribute significantly towards abstinence, using condoms, suggesting condoms, and HIV/AIDS-related stigmatisation due to the complexity of practice actualisation related to theories of planned behaviour.
Conclusion:
STI-related knowledge and attitude correlate well, but this study found that neither predicts STI-related practice.
1. INTRODUCTION
Sexually transmitted infections (STIs) are considered a significant public health threat worldwide, more prevalent in developing countries due to high population density and mobility, and are widespread due to exposure to various risk factors [1, 2]. As evidence that people of reproductive age have a high risk of developing STIs throughout their lifetimes, as of 2021, 95.6% of the 38.4 million people living with HIV/AIDS (PLWHA) worldwide were women [3]. However, Indonesian STI data are still difficult to access. A previous study in a primary care clinic in Jakarta found that the prevalence of STIs was 34.2% overall, with gonorrhoea occurring in 22.4% of cases, syphilis in 7.1%, and HIV prevailing in 4.7% of cases [4].
A growing body of evidence revealed that women are more disadvantaged by STIs-related issues due to a higher risk of developing the disease due to the unique vaginal anatomy, but having more debilitating complications because of the lack of STI symptoms, the threat of antimicrobial resistance, risks of infertility and pelvic inflammatory disease, and high-risk pregnancy [5-7]. Every week, around 4,900 young women aged 15–24 become infected with HIV [3]. Also, human papillomavirus (HPV), which attacks the reproductive system, have more severe consequences in women (cervical cancer) than in men [8]. This worrying issue worsens Indonesian women with their specific needs and challenges regarding reproductive health issues, such as hostile circumstances, lack of access to health information, poverty, and misconceptions due to cultural beliefs [9]. Due to the rapid urbanisation in developing countries, there is an enormous abundance of health-related misinformation available online. Unfounded health myths and health beliefs are also perpetuated through telling and retelling. Additionally, seeking medical help is delayed because many initially turn to alternative medicine solutions. All of these factors may aggravate the progression of the disease [10, 11].
On the other hand, given the various unique factors contributing to the rising STI incidences, urbanisation may play a critical role in spreading the disease. In urban environments, with more entertainment options like pubs and clubs, women are more exposed to risky behaviours, such as increased premarital sex and frequent multiple sexual intercourses [12-14]. Additionally, urban areas tend to have higher concentrations of commercialised sexual workers and drug users, possibly due to rising urban impoverishment [12]. It is also important to note that higher population densities may lead to more frequent human interactions and shifting social norms and thus may promote STI transmission [15, 16]. Although urban residents often have better health, education, and wealth, socioeconomic inequities are frequently made worse in Indonesian settings. These differences may determine a person’s general health and affect how infections pattern [15, 16].
Local characteristics such as knowledge, attitudes, and practices (KAP) of women should be established first to develop educational programs and interventions to control the occurrence of STIs. However, this data on the Southeast Asia population remains limited [17, 18], and most KAP studies on STIs come from Africa [19-23]. Furthermore, due to traditional and revived social norms that maintain tight taboos on premarital sex and stigmatise participants, it is challenging to understand the issues concerning sexuality and reproductive health in Indonesia [24]. This situation results in a lack of apolitical discussion of STIs within communities [25]. A recent study from urban communities in Indonesia only focused on HPV infection and did not necessarily explore the overall understanding of STIs [26]. Other studies merely highlighted the incidence of STIs [4] and sexual well-being [27] among adolescents rather than elaborating on the KAP among women. Striving to fill the research gap and overcome the issue of women’s STIs, this study aimed to understand the characteristics of the socio-demographic profile of reproductive-age women in an urban community health centre in Jakarta, Indonesia, as well as explore the association between KAP and STIs.
2. MATERIALS AND METHODS
2.1. Background Information on the Study Area
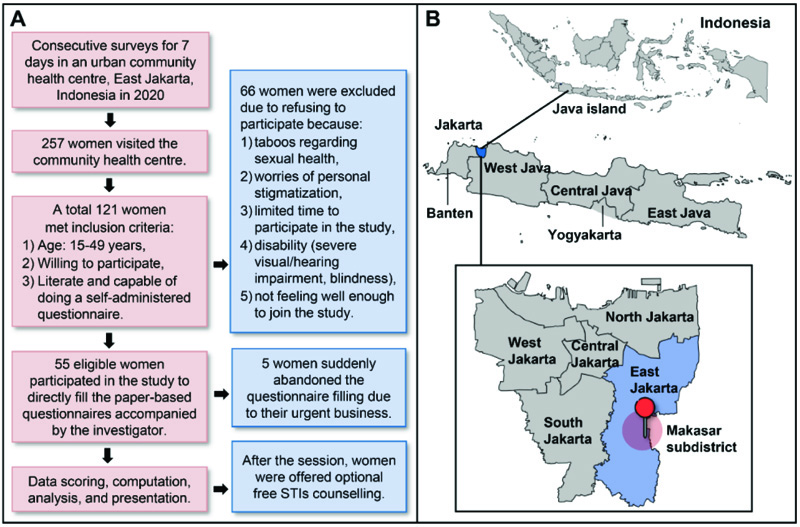
Jakarta is one of the more urbanised provinces of Indonesia and, as a major city in Indonesia, made home to 10.64 million inhabitants, including 2.9 million women of reproductive age, in 2021 [28]. As the largest municipality in Jakarta, East Jakarta covers 27.51% of the province’s area, measures 182.70 km2, and has a population of 3 million [28, 29]. Here, the number of women of reproductive age was around 850,397 in 2021 [29, 30]. One of the ten subdistricts in East Jakarta, the Makassar Subdistrict (Fig. 1), has a population of around 208,365 people (6.82% of the total East Jakarta population) and occupies 11.62% of the area of East Jakarta [29].
Makassar subdistrict is home to the Makassar Community Health Center, which offers STIs-specific services and is one of the city’s leading primary care providers [31]. This facility frequently identifies high-risk factors that contribute to the high incidence of STIs in this area, as confirmed by an earlier primary care study in East Jakarta [4]. According to an in-depth interview with a local healthcare officer, prostitution localisations, online prostitution services, commercial sex workers, adolescent sexual abuse and harassment, and unwanted pregnancies are worrisome phenomena that have been documented. As a result, the number of STI visits in the community health centre policlinic has increased.
2.2. Study Population, Design, Sampling, and Selection of Participants
This survey-based analytical cross-sectional study was conducted using a self-administered and structured questionnaire from July 14th to 20th, 2020, in an urban community health centre in Makassar Subdistrict, East Jakarta, Indonesia. Employing a consecutive sampling technique, all female patients who visited the polyclinics in this centre (not limited to STIs cases) of reproductive age (15–49 years) [32] were invited to participate in this research. Patients who were voluntarily willing to participate and literate to fill out the questionnaire were included in this study. Some patients were excluded due to refusal to participate for several reasons, as stated in Fig. (1). The sample size in our study was 50 subjects, which fulfilled the minimum sample size calculated based on the formula for the proportion of two independent groups [33]
Abbreviation: STIs: sexually transmitted infections.
and an online calculator from Statistic, UK [34]. For calculation, we assumed a 95% confidence interval (CI), a Zα=1.96, statistical β-power of 80% (Zβ=0.84), a sample proportion in group 1 (P1) of 0.60, and a sample proportion in group 2 (P2) of 0.33 following a previous study [22, 35]. The details of the formula are described below.
 |
(1) |
2.3. Study Instrument, Variables, and Data Collection
The primary data was collected directly from patients using a questionnaire that has been pre-tested on 10% of the study participants and has been verified by experts from Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia [36]. It also has been statistically validated previously with a Cronbach’s alpha reliability testing of 0.75 (reliable) and a validity coefficient of r=0.65 (moderate correlation) for each aspect of KAP following reference value interpretation [37, 38]. The questionnaire consisted of four sections: (1) demographics, (2) knowledge, (3) attitude, and (4) practice assessment (Supplementary File 1). Assessed socio-demographic profiles were age, educational level, marital status, and the number of children (parity). Young adults (<30 years) were defined following the European statistical criteria [39]. The educational level and parity classifications were based on earlier research [26, 40]. The questions of KAP in this questionnaire were built upon existing literature that described the question items by exploring respondents’ knowledge [17, 26, 41-43], attitude [17, 26, 41, 43-45], and practice [44, 46, 47] about STIs. Before applying the research instrument, our questionnaire was translated backwards and afterwards into ‘Bahasa Indonesia’ to prevent language barriers. In total, there were 34 questions in our questionnaire.
The knowledge assessment consists of 15 items of multiple choice questions regarding the definition of STIs, transmission method, risk factors, prevention actions, HPV, cervical cancer, and vaccination, understanding of seeking (medical) help, STIs symptoms and detection, as well as treatments. Meanwhile, aspects of attitudes were assessed using 15 items of questions with a Likert scale (score 1 to 4), with the highest score given to favourable answers. The questions include perspectives regarding the transmission and prevention of STIs, specific protections from STIs, sexual education, and STIs stigmatisation. The last measured aspect was practice or behaviour related to STIs, with 4 simple items of practices being measured, including abstinence, condom use, condom suggestion to peers, and stigmatisation of STIs. The knowledge and attitude score measurement is based on a scoring system from earlier studies, which highlighted that a correct response with a score equal to or more than 60% would be classified as having good knowledge or positive attitudes. The knowledge measurement was rated as ‘poor’, and the attitude was interpreted as ‘negative’ if the participant scored less than 60%. Only two dichotomised answers—yes, reflecting favoured practice, and no, reflecting unfavourable practice—were used to score the four measured practices [26, 48, 49]. The questionnaires were filled in anonymously, masked by the respondent number (participant identities were recorded separately), including the demographic features in the first part. Since this study is a part of community development, thus in the final section of the study, investigators provide optional free health counselling if respondents need additional resources or information on STIs.
2.4. Data Analysis
The data were entered into Microsoft Excel Office 365 v2208, 32-bit edition (MSO Corp, the US) and exported to SPSS package v24 64-bit edition (IBM corp, the US) for analysis. According to the Shapiro-Wilk normality test, continuous data were described as mean with standard deviation (SD) or median score with interquartile range (IQR). A score of knowledge and attitude was drawn for their correlation using Spearman’s rank test. Rho degree (ρ) of correlation was interpreted according to the standard: 0, no correlation; 0.01–0.2, very weak correlation; 0.2–0.4, weak correlation; 0.4–0.6, moderate correlation; 0.6–0.8, strong correlation; 0.8–1, very strong correlation; and 1, monotonic correlation [50]. Categorical variables were described, and the absolute frequency and percentage were compared statistically. The statistical test used in the bivariate analysis was the χ2 or Fisher exact test [51]. The binary logistics regression model and Cochran-Mantel-Haenszel test with a common odds ratio (OR) were applied to identify the association between knowledge and attitude levels. The level of significance (p-value) was denoted at <0.05. Visualisation of data employed Microsoft Excel and PowerPoint, while the scatterplot was generated using Minitab v19.1, 64-bit edition (Minitab, LLC, the US). We followed the STROBE guideline for cross-sectional studies to report and write this study [52].
2.5. Ethical Approval and Patients’ Consent
The Health Research and Ethics Committee of the Faculty of Medicine, Universitas Indonesia, granted ethical permission for this study (KET-237/UN2.F1/ETIK/PPM.00.02/2020) under the umbrella research of KAP on HPV infection, which previously has been published [26]. After receiving a verbal explanation regarding the use of this research, written informed consent was gained from each participant. Participants voluntarily participate in this study with the investigator’s assurance regarding their information confidentiality. The subjects also knew their right to withdraw from the study.
3. RESULTS
3.1. Characteristics of the Subjects: Socio-demographic Analysis
In total, 50 women of reproductive age were recruited. They had a mean age of 26.80 ± 4.64 years, with 70% of them aged 20–29 years, 60% had the highest education level of SHS, and 88% of participants were categorised as having high-level education, 74% were married, and 48% primiparous. A detailed characterisation of the subject’s socio-demographic profiles involved in this study is shown in Table 1.
| Subjects Characteristics | n | % |
|---|---|---|
| Age (Years) | - | - |
| 15-19 | 3 | 6.0 |
| 20-29 | 35 | 70.0 |
| 30-49 | 12 | 24.0 |
| Age Classification (Years) | - | - |
| ≤30 (Young Adults) | 40 | 80.0 |
| >30 (Adults) | 10 | 20.0 |
| Highest Level of Formal Educational | - | - |
| Primary school | 4 | 8.0 |
| Junior high school (JHS) | 2 | 4.0 |
| Senior high school (SHS) | 30 | 60.0 |
| Vocation | 3 | 6.0 |
| Bachelor | 11 | 22.0 |
| Level of Education | - | - |
| Low (≤ JHS) | 6 | 12.0 |
| High (≥ SHS) | 44 | 88.0 |
| Marital Status | - | - |
| Married | 37 | 74.0 |
| Not married | 13 | 26.0 |
| Number of Children | - | - |
| 0 | 13 | 26.0 |
| 1 | 23 | 46.0 |
| 2 | 12 | 24.0 |
| 3 | 2 | 4.0 |
| Parity Status | - | - |
| Nulliparous | 13 | 26.0 |
| Primiparous | 23 | 46.0 |
| Multiparous | 14 | 28.0 |
| Evaluated Aspects | Number of Subjects | ||
|---|---|---|---|
| n | % | ||
| 1. Knowledge | Good | 42 | 84 |
| Poor | 8 | 16 | |
| 2. Attitudes | Positive | 44 | 88 |
| Negative | 6 | 12 | |
| 3. Practice | 3.1 Abstinence from high-risk sex intercourse | - | - |
| Yes | 27 | 54 | |
| No | 23 | 46 | |
| 3.2 Using condom | - | - | |
| Yes | 16 | 32 | |
| No | 34 | 68 | |
| 3.3 Recommend using condoms to others | - | - | |
| Yes | 1 | 2 | |
| No | 49 | 98 | |
| 3.4 Stay away from people living with HIV/AIDS | - | - | |
| Yes | 18 | 36 | |
| No | 32 | 64 | |
| KAP Aspects | Knowledge | p-value | OR | 95%CI | ||||
|---|---|---|---|---|---|---|---|---|
| Poor | Good | |||||||
| n | % | n | % | Min | Max | |||
| Age | - | - | - | - | - | - | - | - |
| ≤30 years | 7 | 87.5 | 33 | 78.6 | >0.999a | Ref | - | - |
| >30 years | 1 | 12.5 | 9 | 21.4 | - | 1.909 | 0.207 | 17.598 |
| Education | - | - | - | - | - | - | - | - |
| Low (≤JHS) | 3 | 37.5 | 3 | 7.1 | 0.044a | Ref | - | - |
| High (>SHS) | 5 | 62.5 | 39 | 92.9 | - | 7.800 | 1.225 | 49.677 |
| Married | - | - | - | - | - | - | - | - |
| Yes | 7 | 87.5 | 30 | 71.4 | 0.662a | Ref | - | - |
| No | 1 | 12.5 | 12 | 28.6 | - | 2.800 | 0.310 | 25.261 |
3.2. Knowledge, Attitude, and Practice toward Sexually Transmitted Infection
The participants’ median knowledge and attitude scores were 76.90 (IQR: 61.50–84.60) and 79.20 (IQR: 77.10–83.30), respectively. As presented in Table 2 knowledge of STIs was good in 84% of subjects, and a positive attitude was found in 88% of subjects. Practice aspect related to STIs prevention and stigmatisation shows a moderate-level understanding into the participants of this study.
As shown in Table 3, the most significant determinant factor of knowledge was the level of formal education, over the parameter of age and marital status, where high-level education gives an OR 7.80 to give a higher probability of having good knowledge of STIs.
Table 4 shows that good knowledge of STIs significantly predicted positive attitudes (p=0.044) with almost 8-fold odds, which is the most remarkable determinant of this aspect. Meanwhile, age, education, and marriage were not associated with attitudes. This irrelevance was confirmed by the correlation analyses between these two aspects, which revealed a moderate correlation with the ρ-value of 0.482, p<0.001. In the scatterplot (Fig. 2), it was shown that many points of scores between knowledge and attitudes intersect each other. Bivariate analysis in Tables 3 and 4 could not be further extended into multivariate analysis since only one significant factor was determined.
This study further analysed individual aspects of practice assessment on how they are associated with knowledge and attitudes. Table 5 demonstrates that knowledge (p>0.999) and attitudes (p=0.674) were not related to abstinence practice, although more than half of patients practice abstinence when knowing the risk present in their circumstances. Meanwhile, other socio-demographic profiles were not remarkably related to this practice.
| KAP Aspects | Attitudes | p-value | OR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| Negative | Positive | |||||||
| n | % | n | % | Min | Max | |||
| Age | - | - | - | - | 0.586a | - | - | - |
| ≤30 years | 4 | 66.7 | 8 | 81.2 | - | Ref | - | - |
| >30 years | 2 | 33.3 | 36 | 18.2 | - | 0.444 | 0.069 | 2.861 |
| Education | - | - | - | - | 0.556a | - | - | - |
| Low (≤JHS) | 1 | 16.7 | 5 | 11.4 | - | Ref | - | - |
| High (>SHS) | 5 | 83.3 | 39 | 88.6 | - | 1.560 | 0.150 | 16.198 |
| Married | - | - | - | - | 0.319a | - | - | - |
| Yes | 6 | 100.0 | 31 | 70.5 | - | Ref | - | - |
| No | 0 | 0 | 13 | 29.5 | - | n/a | n/a | n/a |
| Knowledge | - | - | - | - | - | - | - | - |
| Poor | 3 | 50.0 | 5 | 11.4 | 0.044a | Ref | - | - |
| Good | 3 | 50.0 | 39 | 88.6 | - | 7.800 | 1.225 | 49.677 |
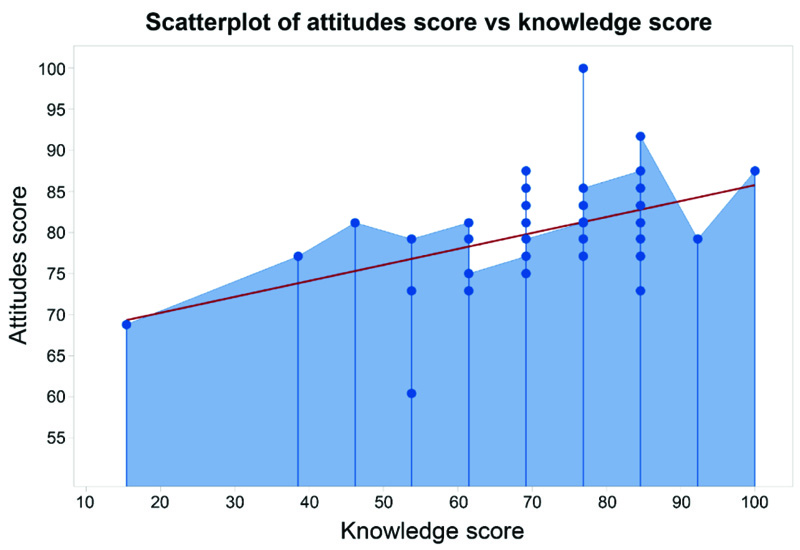
Table 5.
| KAP Aspects |
Abstinence from high-risk sex intercourse |
p-value | OR | 95%CI | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| n | % | n | % | Min | Max | |||
| Age | - | - | - | - | 0.736a | - | - | - |
| ≤30 years | 19 | 82.6 | 21 | 77.8 | - | Ref | - | - |
| >30 years | 4 | 17.4 | 6 | 22.2 | - | 1.356 | 0.332 | 5.554 |
| Education | - | - | - | - | 0.395a | - | - | - |
| Low (≤JHS) | 4 | 17.4 | 2 | 7.4 | - | Ref | - | - |
| High (>SHS) | 19 | 82.6 | 25 | 92.6 | - | 2.632 | 0.435 | 15.907 |
| Married | - | - | - | - | 0.990b | - | - | - |
| Yes | 17 | 73.9 | 20 | 74.1 | - | Ref | - | - |
| No | 6 | 26.1 | 7 | 25.9 | - | 0.990 | 0.279 | 3.523 |
| Knowledge | - | - | - | - | - | - | - | - |
| Poor | 4 | 17.4 | 4 | 17.4 | >0.999a | Ref | - | - |
| Good | 19 | 82.6 | 23 | 85.2 | - | 1.211 | 0.267 | 5.498 |
| Attitude | - | - | - | - | - | - | - | - |
| Negative | 2 | 8.7 | 4 | 14.8 | 0.674a | Ref | - | - |
| Positive | 21 | 91.3 | 23 | 85.2 | - | 0.548 | 0.091 | 3.305 |
Despite the fact that using condoms offers specific STI protection, study results indicated (Table 6) that knowledge (p=0.647) and attitude (p=0.647), as well as socio-demographic factors, including age, education, and marital status, were not associated with condom adoption and usage. These findings were also related to the fact that only a few women (32%) showed condom use practice. The analysis also reveals that knowledge (p>0.999) and attitudes (p>0.999) were not related to the practice of suggesting condom use to people who are about to have sex since only one subject said have experienced recommending or would recommend condom use for her relatives, partners, or even friends. Thus the significant association could not be precisely drawn (the table is not presented).
| KAP Aspects | Using condom | p-value | OR | 95%CI | ||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| n | % | n | % | Min | Max | |||
| Age | - | - | - | - | 0.468a | - | - | - |
| ≤30 years | 26 | 76.5 | 14 | 87.5 | - | Ref | - | - |
| >30 years | 8 | 23.5 | 2 | 12.5 | - | 0.464 | 0.087 | 2.492 |
| Education | - | - | - | - | >0.999a | - | - | - |
| Low (≤JHS) | 4 | 11.8 | 2 | 12.5 | - | Ref | - | - |
| High (>SHS) | 30 | 88.2 | 14 | 87.5 | - | 0.933 | 0.152 | 5.715 |
| Married | - | - | - | - | 0.301a | - | - | - |
| Yes | 27 | 79.4 | 10 | 62.5 | - | Ref | - | - |
| No | 7 | 20.6 | 6 | 37.5 | - | 2.314 | 0.625 | 8.575 |
| Knowledge | - | - | - | - | 0.409a | - | - | - |
| Poor | 7 | 20.6 | 1 | 6.3 | - | Ref | - | - |
| Good | 27 | 79.4 | 15 | 93.8 | - | 3.889 | 0.436 | 34.689 |
| Attitudes | - | - | - | - | 0.650a | - | - | - |
| Negative | 5 | 14.7 | 1 | 6.3 | - | Ref | - | - |
| Positive | 29 | 85.3 | 15 | 93.8 | - | 2.586 | 0.277 | 24.189 |
| KAP Aspects |
Stay away from people living with HIV/AIDS |
p-value | OR | 95%CI | ||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | |||||||
| n | % | n | % | Min | Max | |||
| Age | - | - | - | - | >0.999a | - | - | - |
| ≤30 years | 25 | 81.3 | 14 | 77.8 | - | Ref | - | - |
| >30 years | 6 | 18.8 | 4 | 22.2 | - | 1.238 | 0.299 | 5.134 |
| Education | - | - | - | - | 0.171a | - | - | - |
| Low (≤JHS) | 2 | 6.3 | 4 | 22.2 | - | Ref | - | - |
| High (>SHS) | 30 | 93.8 | 14 | 77.8 | - | 0.233 | 0.038 | 1.429 |
| Married | - | - | - | - | 0.098a | - | - | - |
| Yes | 21 | 65.6 | 16 | 88.9 | - | Ref | - | - |
| No | 11 | 34.4 | 2 | 11.1 | - | 0.239 | 0.046 | 1.231 |
| Knowledge | - | - | - | - | - | - | - | - |
| Poor | 6 | 18.8 | 2 | 11.1 | 0.694a | Ref | - | - |
| Good | 26 | 81.3 | 16 | 88.9 | - | 1.846 | 0.332 | 10.281 |
| Attitudes | - | - | - | - | - | - | - | - |
| Negative | 5 | 15.6 | 1 | 5.6 | 0.399a | Ref | - | - |
| Positive | 27 | 84.4 | 17 | 94.4 | - | 3.148 | 0.338 | 29.311 |
Table 7 demonstrates that knowledge (p=0.694) and attitudes (p=0.399), as well as socio-demographic characteristics (such as age, education, and marriage), did not influence the women’s practice or perspective toward the stigmatisation of STIs. Of all subjects, about 36% of them choose to stay away from people with HIV/AIDS. Bivariate analysis in Tables 5 to 7 could not be further pursued as multivariate analysis since no significant factor was generated.
4. DISCUSSION
This work contributes to the sparse but expanding body of research on the understanding of STIs among women of reproductive age in urban environments of the Southeast Asia region. Westernisation and other ‘modernising’ influences have contributed to increasing sexual permissiveness amongst Indonesian youth, especially women [53]. Premarital sex among sexually active girls has been reported to be increasing by 23% worldwide [54, 55] and found to be more common in urban areas, such as Jakarta, as a result of changing norms and values that make this behaviour increasingly acceptable among young people, especially in the context of a romantic relationship [25]. These phenomena will increase STIs, which will be more prevalent in sexually active women of childbearing age. This age group has become a significant factor in spreading STIs, mainly due to partnered sexual activity, pregnancy, and childbirth [7]. In this regard, our present work spotted a higher proportion of younger adults with a mean age of 26.80 ± 4.64 years as participants, older than in a previous study in urban Nigeria (19.90 ± 2.50 years) [22]. Age has been associated with susceptibility to STIs related to their sexual exploration at a young age [56]. It also tends to be related to premarital sexual behaviour. Although the results were not statistically significant, a previous study in India indicated a tendency that females aged 15–19 were more likely (OR: 1.99, 95%CI: 0.68–5.83, p>0.05) to have premarital sexual intercourse than those aged 20–24 [57]. Adolescents are more likely to engage in risky behaviours that might end in STIs because of peer, cultural, and social pressures [58]. The situation might worsen since most Indonesian youths are unaware of how to prevent STIs [25, 59].
The high prevalence of premarital sex and STIs followed the understanding level and sexual behaviour associated with formal education [59]. Our subjects possessed sufficient education level (60% of women had passed SHS), in line with a local governance survey of East Jakarta, which revealed that 49.57% of citizens had passed SHS [29] and similar to a study in urban Nigeria (64%) [22]. This study found that higher educational attainment has significantly contributed to high-level knowledge of STIs and their prevention. We found that more than 80% of our respondents had good knowledge, comparable to the study in the urban community of Nigeria (66%) [22]. The level of knowledge of our participants who represent the urban Indonesian community was much higher than in research conducted in rural community health centres in Indonesia, which found the percentage of visitors who had good knowledge was 54% in West Kalimantan [60] and 50% in Riau [61, 62]. These different results may reflect ongoing challenges of urban-rural disparity in education expansion and the utilisation of primary health care in providing specific and targeted health promotion among the Indonesian population [63, 64]. However, urban women still lack knowledge on a specific topic (HPV infection) since only 32.4% of women had good knowledge in an earlier study [26].
Moreover, compared to the rural study focusing on reproductive health issues in Indonesia, our findings indicate a significant disparity in knowledge between urban and rural Indonesia [62]. We also noted that education level was the sole robust predictor of knowledge level over age, marriage, and parity, conforming to prior studies in Indonesia [4], Nigeria [20] and Malaysia [35], which also indicated no relationship between these socio-demographic characteristics towards knowledge level of STIs. Therefore, we emphasise that education and knowledge have a crucial role in reducing the phenomenon of risky sexual behaviour, STIs and other reproductive health-related issues today. Supporting this idea, a Taiwan study also stated that educational attainment is the most potent determinant of the timing of first marriage, lowering the level of sexual activity and thus lowering the probability of marriage at young ages [65]. More educated women are more likely to successfully control the biological urges to engage in premarital sexual activities. They are more aware of the risks associated with this kind of activity, including the increased risks of contracting STIs and unwanted pregnancies [65].
In elaborating on marriage and childbearing characteristics, this study found that about 74% of women were married, with 46% and 28% primiparous and multiparous, respectively. Although sexual activity is not merely determined by marital and parity status, at least this information gives us approximations of the number of participants with experience of sexual intercourse. Marriage is thought to be a risk factor for developing STIs and HPV-related cancers. A study in China found a higher pregnancy rate to be significantly associated with increased cervical cancer risk (OR 3.8–4.2), while a higher number of live births increased the OR for cervical cancer by around 16.8 (p<0.05) in women with more than three live births [66]. In light of this, a meta-analysis showed that women with high parity had 2.65 times the likelihood of acquiring cervical cancer compared to women with low parity (OR 2.65, 95%CI: 2.08–3.38) [67]. Since cervical cancer is also a debilitating impact of STIs (i.e., HPV infection), thus this should also be our concern, and we reinforce a suggestion towards women of reproductive age to routinely conduct cervical screening when they have a history of sexual intercourse, either marital or premarital, to confirm whether HPV infection is present.
It was found that 88% of women had a positive attitude about STIs in this study, higher than in previous studies in rural areas of Indonesia (46.7–70.0%) [60, 61] and Ethiopia (54.5%) [23]. These results were probably due to our participants’ high level of knowledge (but not necessarily due to their level of education), where good knowledge was predicted to enhance 7.8 times higher odds of having favourable attitudes. Meanwhile, education was not associated with attitude (OR 1.56, p=0.556). This link between knowledge and attitude can be explained by the fact that, according to the theory of planned behaviour, knowledge is a critical modifier of positive attitudes [68]. Someone with extensive knowledge tends to be positive in attitude (related to screening for STIs, seeking health personnel, and avoiding pornography) [69]. Similar to the insignificant association between the socio-demographic profiles and knowledge, we also confirmed that a socio-demographic profile is insignificantly associated with participants’ attitudes in this study. In contrast, a Malaysian study found that age was associated with attitude despite not being associated with knowledge [35].
Although our knowledge and attitudes regarding STIs were favourable at first glance, hurdles still exist in urban regions of Indonesia since the community's health literacy level varies between and within regions. Adolescent sexuality is still heavily stigmatised in Indonesia [27]. Moreover, we failed to capture the association between knowledge and attitude toward practice. However, various studies have revealed similar scenarios in other countries worldwide [70, 71]. A previous study in a coastal area of Indonesia also indicated that good knowledge and attitudes did not guarantee good practice. Their research demonstrated a good knowledge of HIV/AIDS in coastal areas and that attitudes toward the disease are adequate, yet it cannot be assumed that people will behave safely. In this study, some participants still had premarital sexual intercourse, did not use condoms, had sexual activities with prostitutes, had multiple sexual partners, and had ongoing STI symptoms during the survey [72]. Our findings did not support Bloom’s taxonomy theory (1956) of educational learning objective, in which practice is influenced by knowledge and attitude because knowledge is a necessary precondition for putting skills and abilities into practice [70, 71]. However, if we view this phenomenon from the recent theory of reasoned action and planned behaviour (TPB), we would get a broader perspective that the practice or behaviour aspect is a complex framework and not merely determined by a good knowledge score and attitude [68]. The lack of correlation between knowledge and attitude towards practice might be due to uncaptured or unidentified confounding factors that may influence these phenomena [73]. In the TPB, there are three main backgrounds of contributing confounding factors, such as personal background (i.e., personality, mood, emotion, intelligence, values, stereotypes, general attitudes, and experiences); social environment (i.e., education, age, gender, income, religion, race, ethnicity, and culture); and availability information (knowledge, media, and intervention) [68]. These background factors interact with each other to produce three proximal constructs: attitudes toward the behaviour (positive or negative outcomes of the behaviour), subjective norms (perceived social pressure to engage or disengage in the behaviour), and perceived behavioural control (perceived ability to perform the behaviour). It is considered that the practice/behaviour and intention are directly related. The intention to engage in a practice/behaviour is believed to be influenced by attitudes, subjective norms, and perceived behavioural control. In this model, individuals will begin to engage in certain practices or behaviours once they have gained the awareness, knowledge, and desire to do so; thus, although knowledge and attitude levels were already satisfying, as long as the participants did not have good awareness and willingness regarding its practice, non-correlation is expected [70, 71].
To exemplify the application of TPB, we found that people tend to respond negatively to the practice of using and giving condoms. It is possible because, in Eastern culture, condoms are often associated with free premarital sex behaviour, which is not following Indonesian values and norms. In our study, 32% of respondents said that they used condoms; a similar rate was observed in urban people in India (24.5%) [74] and Kenya (29.0%) [19] but contrasted with a Nigerian study on urban communities (79.3%) [22] and a Malaysian study on students (63.8%) [17]. The fact that more respondents to our study were married and therefore believed that condoms were less valuable than when they were single contributed to the reduced rate of condom use. Giving advice or condoms to friends is also uncommon in our society because it is closely tied to stigmatisation. An earlier study in the same municipality confirmed the lack of condoms in East Jakarta primary care, which found that using a condom only occurred in 14.1% of STI patients in the polyclinic [4]. Most reasons are unpleasant feelings, an embarrassment to buying condoms, and cost-related issues [4]. These results may provide stakeholders with information to continue their efforts to promote frequent condom use, particularly for the targeted high-risk group, as the key to decreasing STI transmission with the purpose of prevention over stigma, religion, norms, or personal subjectivity concerns [58].
As for abstinence practice, there were not many positive responses because most respondents were married; hence, abstinence may not be their best option to prevent STIs. We also found that knowledge and attitude were not strong enough to influence the practice of avoiding PLWHA. However, in the bivariate analysis, there was a tendency that good knowledge (OR 1.846, p=0.694) and a positive attitude (OR 3.148, p=0.399), is slightly giving a better understanding to the community that HIV patients are not to be shunned, stigmatised, or even isolated from social life. Although a good understanding of the practice of avoiding PLWHA was seen in this study, and most of our respondents did not avoid PLWHA, we should admit that Indonesia still faces challenges in stigmatisation toward PLWHA [75]. Similar to Indian society, it is evident that STIs are strongly linked to social condemnation, disgrace, and rejection in Indonesia [76]. Sexuality and its health implications continue to be widely stigmatised. Although their rights and needs may be accepted in principle and practice, they nonetheless face numerous impediments when trying to get assistance in actual life. With extensive knowledge and a positive attitude, eventually, an understanding that STIs and HIV patients will not be stigmatised or isolated from society will develop [77-80]. Aligned with this, a study in China also showed a relationship between education and attitude, whereby the higher the level of education a person had, the more positive their attitude and acceptance of PLWHA [81]. Inversely, a lack of HIV-related knowledge can lead to misconceptions regarding disease transmission [82]. In overcoming this issue, mass media information is essential for society to understand STI-related, HIV-related, and stigmatisation attitudes and information [83, 84]. However, much neglect is given to media information about HIV, which reduces understanding and impacts stigmatisation attitudes. A previous study on the stigmatisation attitude of people showed a correlation with ignorance of information on transmission, prevention, and treatment of HIV [81].
Negative labelling, ignorance of HIV, fear of contracting the disease, personal values, religious beliefs, and sociocultural norms and values are all identified as catalysts or enablers of HIV-related stigma and discrimination in Indonesia [85]. In families, communities, and healthcare facilities, attitudes toward the undervalued attribute frequently result in prejudice, stereotyping, and discrimination toward PLWHA [86, 87]. At the community level, examples of stigmatisation and discrimination include refusing to sit close to PLWHA, changing seats away from PLWHA, being afraid to physically interact with PLWHA [87], PLWHA dropping out of school, not being allowed to play together, and not eating with peers [88]. There was still a lack of tolerance toward people with STIs and HIV/AIDS, thus encouraging stigmatisation. Several Indonesian studies related to HIV/AIDS stigmatisation revealed that 56% of household heads demonstrated high stigmatisation of PLWHA [89], more than half (71.63%) of youths stigmatised PLWHA [90], and younger people were 1.19 times more likely to discriminate against people with HIV [91].
Interestingly, the highest prevalence of stigmatising attitudes was on the island of Java (59.82%), particularly in the urban areas, compared to other regions in Indonesia [75]. A further impact of discrimination on PLWHA is worrisome, such as the loss of jobs, social status, and family and community support hence developing a tendency to avoid proper treatment [75]. Stigmatisation and discrimination that result in a reluctance to seek treatment for PLWH will worsen their health condition and increase their prevalence due to undetected spread. According to a study [75], younger people are more likely to discriminate against people with HIV, and thus we should focus on female participants at a younger age. Youths do not understand and realise their stigmatisation and discrimination and their effects on people with HIV [75].
The lack of correlation between knowledge and attitudes with practice might reflect that some preceding factors may need to be improved, which is how to apply these two aspects to actual practice. Our findings are an alarm and highlight substantial dysfunction in the Indonesian educational system, where the focus should not only be on improving knowledge and attitude but also on improving the actual practice of young people regarding STIs. Moreover, to better understand STIs, it is essential to involve the parents in sexual and reproductive health education before children reach puberty. The preciousness and usefulness of parent-child interactions for the prevention of STIs were highlighted in 2010 by Deptula et al. [92] who discovered that supportive parent-child interactions are linked to decreased rates of unprotected sex, unwanted pregnancies, and adolescent STIs. Unfortunately, the parent’s role in educating their children about reproductive health remains lacking in Indonesia. Indonesian women, in this context, are characterised as a more closed-personality who are uncomfortable discussing sexual issues with their partner(s), children, family, or even parents [27]. The women’s lack of reproductive health knowledge was a significant cause of such risky behaviour. Indeed, prior qualitative studies demonstrate how Indonesian parents and youth avoid discussing puberty and sexuality because they perceive it to be irrelevant and taboo [27]. It should be encouraged that parental communication is vital for shaping sexual health knowledge and attitudes [80].
Due to the fact in this study that 74% of respondents were mothers, our study is calling out Indonesian women to improve their KAP towards STI and reproductive health to play a better role as educators for their children later. This message should also be directed to the 26% of women who were not childbearing and/or unmarried. Women should be fully provided with adequate KAP on reproductive health to prevent STIs and related problems. Since the need for sex education for young people and women has been articulated, we should also emphasise the need to strengthen the role of community health centres in Indonesia, particularly in urban communities. General practitioners, midwives, clinical psychologists, and nurses must be trained to conduct health counselling about STIs. In more extended action, trained healthcare workers in community health centres could train teachers at school, mothers, peer support, and other volunteers on how to adequately talk about sexuality to their children [77-79].
4.1. Strength and Limitations
Regarding research ramifications, our findings support the urgency and complexity of STI KAP measurements in reproductive-age women in a low-middle-income country. We strive to fill the data gap from Indonesian urban communities and report women of reproductive age's understanding of STIs, which puts them at a disadvantage. We comprehensively analysed the aspect of KAP and discussed relevant issues about the socio-demographic characteristics of urban communities, women’s current challenges, and the stigmatisation of STIs. However, a few drawbacks to our study should be acknowledged, including the cross-sectional baseline data, which restricts claims about causality.
Using this design without observation, especially for the practice aspect, means we cannot prove these variables’ causality. Moreover, since the nature of the survey-based cross-sectional study is sensitive, reporting errors and biases could not be controlled. However, most published KAP studies use this design due to its practicability and time saved. Another caveat of our study is that the sample size was relatively small and calculated based on the minimum requirement due to the study population’s low accessibility and high personal refusal. Therefore, the findings of this study may not be generalisable to the whole urban community of Indonesia. The lack of representativeness of the population in this study might make the findings should be used with care. However, this study is comparable, as most surveys relied on a relatively small number of participants [35,93].
The questionnaire was also self-administered; some questions may be misunderstood, yet we overcame this challenge by accompanying the participants when they gave their responses. We made the direct approach instead of distributing online to ensure that the participants’ accurate impressions could be acquired well. Another limitation was the multiple-choice answers we used in the knowledge aspect, which might allow participants to guess or assume answers. However, this was more applicable to our population to prevent a low response rate primarily observed in the open-question model. Also, in the practice aspect, as this study only assesses four topics, it might be a minimal assessment of practices and behaviours related to STIs. However, these four aspects were the most scrutinised and relevant aspects of STIs.
CONCLUSION AND RECOMMENDATION
This study elucidated the KAP of STIs among women of reproductive age at an urban community health centre in Jakarta, Indonesia. The association between the level of education and knowledge was impressive. The higher the educational attainment, the higher the participants’ knowledge about STIs-related issues. It has also been confirmed that the level of knowledge and attitudes related to STIs is correlated and gives a high probability of having a positive attitude when the baseline of knowledge is good. However, there was no statistically significant relationship between knowledge and attitudes towards behaviours assessed in this study (abstinence, using and giving recommendations about condoms, and stigmatisation of PLWHA). It was discovered that better practice tends to result from promoting good knowledge and positive changes in attitudes. Existing educational policies should integrate into sex education and modify message delivery to improve the knowledge and attitude, but also emphasise the proper applicable practice in preventing STIs.
In order to combat constrictive and prejudiced STI norms, our findings also suggest that public health initiatives should target not only reproductive-age women, but also their societal surroundings (such as parents, adolescents, teachers, and community members) [94]. It is imperative to support women in their reproductive years in their crucial roles as mothers or future mothers who will play a significant role in educating their children about sexuality and reproductive health and as wives who should be aware of their reproductive health. To address underlying societal norms in urban cities that cause women to be reluctant, multi-component and multi-level interventions are requires [95]. The aforementioned suggested interventions can be implemented while promoting more extensive structural reforms and collaborating with families, cross-sectoral groups, and community health centres.
Simple solutions based on the interactions between KAP are constantly desired; however, this study reveals that data was sparse. Further studies will be critical to better understanding STIs among urban, suburban, and rural areas of Indonesia involving larger sample sizes, multi-level, and geospatial analysis [96,97]. These analyses could provide a more specific direction for mapping health disparity in Indonesia and thus may help design more directed and targeted interventions. We also urge Indonesian researchers to keep exploring STIs across the stages of life using representative samples from various socioeconomic and cultural contexts. Lastly, STI risk and vulnerability across Indonesia’s diverse population should be reduced through collaboration among policymakers, health service providers, families, the community, and people at high risk.
AUTHORS’ CONTRIBUTIONS
HW and MH were the principal investigators of this study. HW acquired funding, controlled the decision to publish, and accepted full responsibility for the overall content of the work. MH conceptualised the study, investigated, designed the methodology, provided the resources, collected the data and did the project administration. HW and MH contributed to the analysis and drafted the paper. MH was entirely responsible for software utilisation, data cleaning, and visualisation of research findings. HW, FK, KHN, TDA, TWU, ADP, and DMS supervised the study process thoroughly and validated all data analyses. All authors critically revised the manuscript for important intellectual content, and all authors gave final approval for the version to be published.
LIST OF ABBREVIATIONS
| AIDS | = Acquired immunodeficiency syndrome |
| HIV | = Human immunodeficiency virus |
| HPV | = Human papillomavirus |
| JHS | = Junior high school |
| KAP | = Knowledge, attitudes, and practices |
| PLWHA | = people living with HIV/AIDS |
| SHS | = Senior high school |
| STIs | = Sexually transmitted infections |
| TPB | = Theory of planned behaviour |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Board of the Faculty of Medicine, Universitas Indonesia, with the ethical clearance number: KET-237/UN2.F1/ETIK/PPM.00.02/2020.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The relevant additional data is available from the corresponding author upon reasonable request, given approval provided by our university’s institutional review board.
FUNDING
None.
CONFLICT OF INTEREST
The authors certify that they have no financial or other conflicts of interest.
ACKNOWLEDGEMENTS
We want to thank all subjects who participated in this research.
SUPPLEMENTARY MATERIALS
Supplementary material is available on the Publisher’s website.


