All published articles of this journal are available on ScienceDirect.
Potential Factors Associated with Stillbirth among Babies Born in Hospitals of North Shoa, Oromia, Ethiopia, 2021 Based on Cross-sectional Study Design
Abstract
Introduction:
Fetal death is one of the common adverse pregnancy outcomes. More than 7178 deaths at 28 weeks of gestation occur every day, making 2.6 million fetal deaths worldwide. The majority of these deaths occurred in developing countries, and 98% occurred in low and middle-income countries. To address the problem of stillbirth, the magnitude and determinants of stillbirth must be understood to help intervention be given to reduce fetal stillbirth. This study was facilitated by obtaining basic data on the factors influencing stillbirth. This will facilitate the development of better public health interventions to reduce these preventable fetal deaths and improve maternal health.
Objective:
This study aimed to assess the determinant factors of still-birth among babies born in hospitals in the North Shoa zone, Oromia, Ethiopia.
Methods:
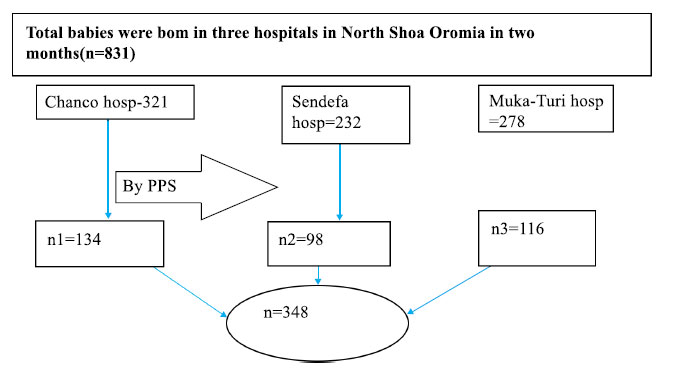
The study was conducted among 348 babies born in the hospital of North Shoa Zone. Study subjects were selected by systematic sampling method from the list of babies born in hospitals in a three-month study period. Data were collected by using a pretested and structured questionnaire. Data were edited, cleaned, coded, entered, and analyzed using SPSS-21 statistical software. Bivariate and multivariate analysis was employed.
Results:
Potential factors were having regular antenatal care, congenital malformation, and having a history of perinatal death, were significantly associated with the stillbirth.
Conclusion:
The risk of stillbirth was associated with both modifiable and non-modifiable factors. Therefore, encouraging regular ANC to follow up, minimizing the formation of congenital malformation, and increasing birth in the history of previous perinatal death prevent the risk of potential stillbirth.
1. INTRODUCTION
Stillbirth or fetal death is defined by the World Health Organization as the death of a baby in utero (antepartum) or during delivery (intrapartum) at 28 weeks or more gestation with a birth weight greater than 1000 g or a body length of less than 35 cm [1, 2]. Fetal deaths happen before the fetus has been completely leaved its mother's womb. Additionally, when a new-born does not show signs of life, such as heartbeat, umbilical cord pulsing, or voluntary muscle activity [2, 3].
Poor service quality in healthcare facilities is one of the factors contributing to the high stillbirth rate, which has remained a problem. Globally, fetal mortality has dropped, but in low- and middle-income countries, it remains unacceptable [1]. Worldwide, there are 2.6 million stillbirths annually, with 98 percent of the deaths occurring in low- and middle-income countries. The poorer nations of Africa account for 10% of stillbirths during intrapartum care, whereas South Asia accounts for 59% [4, 5].
Ethiopia has 258 fetal fatalities daily, ranking 5th among the top ten developing countries in terms of stillbirth rate (at 30 per 1000 live births). Regarding maternal factors which cause stillbirth are (obesity, chronic hypertension, anemia, and sexually transmitted disease); obstetric factors such as antepartum hemorrhage, obstructed labor, and hypertensive disorder of pregnancy and fetal factors such as low birth weight, preterm birth, and prematurity [6].
Sustainable development program involvement, action, and partners recommended a reduction of newborn death and stillbirth to 12 or fewer per 1000 live births in all countries by 2030 [1]. The Ethiopian government, in particular, is working to determine the cause of death information (the application of verbal autopsies) is currently being collected for deaths occurring in health facilities and coded according to the International Classification of Diseases (ICD)10, but no formal application has been made to date [7]. It is crucial to identify the incidence of stillbirth and the factors that influence it in a given situation. However, setup-based data are scarce in the study area. The goal of this study was to determine the rate of stillbirth and the factors that influence it among newborns born in North Shoa, Oromia, Ethiopia.
2. METHODS
2.1. Study Design, Period, and Area
A study was conducted using a cross-sectional study design. The research was conducted from January 1 to March 30, 2021. The population of the North Shoa zone is 1.6 million people. The zone's working language is Afan Oromo. Only Afan Oromo (82.65 percent), Amharic (0.68%), and both languages are spoken in the study area (16.73 percent) [8]. According to the North Shoa zonal health office statistics, there were 4,139 pregnant women every month among the total population. Fiche is the zone's capital and is located 114 kilometers from Addis Ababa. Fiche contains a total of five hospitals and health clinics (64).
There are also 2,420 health professionals on staff, including 213 midwives. This research was carried out at two general and one primary hospital among a total of five hospitals in the zone (Sendefa hospital, Muka turi hospital, and Chancho Hospital). All of the hospitals in this zone provide maternal health services to the neighboring community, including family planning, ANC, delivery, and postnatal care. The hospitals selected have a large number of case fellows.
2.3. Study Population
All Babies had born between January 1 and March 30, 2021, in the three selected hospitals in North Shoa, Oromia, Ethiopia.
2.4. Inclusion and Exclusion Criteria
All babies were born at the three hospitals during the study period.
2.5. Exclusion
Babies had born with severe deformities due to a lack of postmortem evaluation in the institutions.
2.6. Determination of Sample Size
The sample size for the cross-sectional study was estimated with the following parameters: confidence interval =95 percent, power =80 percent, confidence level =5%, and anticipated frequency 71.1 percent using EPI-Info statistical software version 7.1.1 [9].
The overall sample size was 348 based on the above assumptions and a 10% non-response rate.
Systematic sampling technique was used to choose study participants from three public hospitals in the north Shoa zone. Based on a two-month minimum delivery rate in hospitals (August, September, and October) 2020, the entire sample size was allocated proportionally to each hospital. The sampling interval was determined by multiplying the number of mothers who gave birth in the previous three months by the sample size required for each hospital. Data were obtained from each of the two participants. Three hospitals were picked at random for the initial sample unit, while the remainder were chosen depending on the sequence in which they were admitted for labor. Data were obtained in two methods (face-to-face and data review) before participants were discharged from hospitals based on their last menstrual cycle or ultrasound findings. Before the actual data collection, the data collectors were trained for one day. After a minimum of 6 hours after delivery, the data collector collected information from mothers. First and foremost, we shared our pain with the mother of a stillborn child. Then, we gathered information.
2.7. Method and Techniques used for Data Collection
The questionnaire was first composed in English and then translated into Afan-Oromo. Face-to-face interviews and semi-structured questionnaires were used to collect data (9-12) and data that has been recorded (hemoglobin level, syphilis, HIV, and newborn weight). Questioner dependability was measured using Cronbach's alpha, which was found to be 0.78. Three BSc midwife data collectors carried out the data-gathering technique with prior data collection expertise and who spoke Afan Oromo and Amharic languages. Supervisors and the lead investigator did ongoing follow-ups throughout the data collection period.
2.8. Study Variables
2.8.2. Independent Variables
Age, education, residence, religion, ethnic group, and referral are all socio-demographic characteristics. Factors connected to obstetrics and complications: - parity, obstructed labor, ANC history mode of delivery, gestational age (GA) at the commencement of labor, previous delivery history, Preeclampsia/eclampsia, Antepartum hemorrhage, early rupture of membranes, and uterine rupture Anemia, chronic HTN, diabetes, and syphilis are all medical problems to consider. Conditions affecting fetuses and newborns: Prematurity/preterm birth, newborn weight at birth, mal-presentation, and congenital deformity are all examples of prematurity/preterm birth.
Factors affecting health care - the usage of partography.
2.9. Operational Definition
2.9.1. Cause of Fetal Death
Pre/eclampsia, obstructed labor, DM, prematurity, congenital anomalies, low birth weight, antepartum hemorrhage, premature of the membrane [10].
2.10. Stillbirth/Fetal Death
Delivery of the fetus without sign of life. It can occur either antepartum or intrapartum [10].
2.11. Intra-partum
Stillbirths/fetal death that have detectable fetal heart sounds upon admission and thus had an Apgar score of 0 at 1 and 5 min, without signs of maceration or fetal death occurring after the onset of labor and before delivery of the fetus [10, 11].
2.12. Antepartum Stillbirth/Fetal Death
has defined a fetus with an Apgar score of 0 at 1 and 5 min. It has signs of maceration or absent fetal heart sound before the initiation of labor [10, 11].
2.13. Data Quality Control
The questionnaire was developed in English and then translated into Afan-Oromo to help respondents comprehend it better. To preserve consistency, the questionnaires were then translated back into English. Data collectors were provided training. Mothers from outside the study area, specifically Chancho Hospital, were pre-tested on the questionnaire sample. The purpose of the pre-test was to confirm that the questionnaire's clarity, language, logical sequencing, and skip pattern were all in order. A change was made if it was necessary. Afan Oromo speakers make up the majority of the populations in our study, while Amharic speakers are uncommon. Data collectors translated the study's question for Amharic speakers to maintain external validity. Initially, the data collectors were chosen based on their ability to communicate in Afaan Oromo and Amharic and their data collection experience.
2.14. Statistical Analysis
After they were verified for completeness and consistency, all completed questionnaires were coded and data input using Epi-data version 4.6. The data was imported to SPSS version 23 for further analysis. Descriptive statistics, including mean, frequency, and percentage, were generated as part of the univariate analysis. The crude odds ratio was used to assess the relationship between a single independent variable and a dependent variable, and variables with p-values less than 0.25 were included to include sufficient variables, and previous studies have used p-value 0.25 as a cut-off point to select variables for multivariable analysis. Using the entry approach technique, the variables were chosen. The VIF and tolerance tests were used to assess the linear correlation between the various predictors for multi-collinearity. The variables' VIF test values ranged from 1.013 to 1.090, and the tolerance test values ranged from 0.917 to 0.987. The model's fitness was assessed using the Hosmer-Lemeshow and omnibus goodness of fit tests, which yielded a p-value of 0.708, and 0.001, respectively, indicating that the model was adequately fitted later. The 95 percent confidence interval (CI) was used to test the statistical significance of the association between the dependent and independent variables, and the adjusted odds ratio was used to assess the strength of the correlation between the predictor's variable and the dependent variable.
3. RESULTS
3.1. Socio-demographic Characteristics
The study included a total of 348 mothers who gave birth at North Shoa hospitals during the data collection period, with a response rate of (309) 92.8%. The mothers' mean (SD) age was 20.8 (±4.93) years Table 1.
3.2. Obstetric Cause of Fetal Death/Stillbirth
Among women who gave birth in hospitals during data collection were HIV-negative (97.1 percent), whereas 2.9 percent were HIV-positive. When the documents were reviewed, 97.7% of the 309 mothers who were tested for VDRL were syphilis-free, 2.3 percent were syphilis positive, and 1.9 percent were not documented. All of the 2.3 percent of people who tested positive for syphilis before birth were treated. During an ANC visit or before giving delivery, 81.8 percent of women had their hemoglobin levels tested. 85.7 percent of moms had normal hemoglobin levels during their pregnancy, whereas 14.3 percent had anemia. Based on their most recent delivery, 86 percent (27.8%) had a birth gap of fewer than two years, while 223 percent (72.2.0%) had a birth interval of greater than or equal to two years, whereas 2.9 percent were HIV-positive. When the document was reviewed, 97.7% of the 309 mothers who were tested for VDRL were syphilis-free, 2.3 percent were syphilis positive, and 1.9 percent was not documented. All of the 2.3 percent of people who tested positive for syphilis before birth were treated. During an ANC visit or before giving delivery, 81.8 percent of women had their hemoglobin levels tested. 85.7 percent of moms had normal hemoglobin levels during pregnancy, whereas 14.3 percent had anemia. Based on their most recent delivery, 86 percent (27.8%) had a birth gap of fewer than two years, while 223 percent (72.2.0%) had a birth interval of greater than or equal to two years Table 2.
3.3. Medical and Newborn and Health Facility Characteristics/Cause of Fetal Death
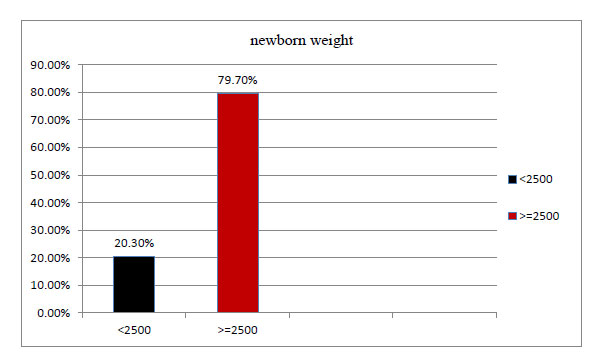
Only 5.7 percent of the 309 individuals had a chronic condition, whereas the majority (94.5%) did. 21.8 percent of the mothers had diabetes mellitus, 15.5 percent had chronic hypertension, and 13.9 percent had anemia (Figs. 1 and 2).
| Variables | Frequency | Percentage % |
|---|---|---|
|
Maternal Age <35 >=35 |
258 51 |
83.5 16.5 |
|
Marital Status Married Single Widowed Divorced |
282 13 14 |
91.3 4.2 4.5 |
|
Occupational Status Farmers Private employee Government employee Laborer/merchant/student |
212 17 32 48 |
68.6 5.5 10.4 15.5 |
|
Religion Orthodox Protestant Muslim |
248 10 51 |
80.3 3.2 16.5 |
|
Ethnicity Oromo Amhara Other |
258 48 3 |
83.5 15.5 1.0 |
|
Educational Status No formal education Primary Secondary and above |
159 108 42 |
51.5 34.9 13.6 |
|
Residence Rural Urban |
147 162 |
47.6 52.4 |
|
Mode of Admission Referred Not referred |
185 124 |
59.9 40.1 |
| Variables | Frequency/Percent | |
|---|---|---|
| Stillbirths | Alive | |
|
Parity (N=309) Prim-Para Multi/grandipara |
12 (9.5%) 31 (16.9%) |
114 (90.5%) 152 (83.1%) |
|
Regular ANC (N=309) Yes No |
21 (10.6%) 22 (19.8%) |
171 (89.4%) 89 (80.2%) |
|
Mode of delivery (N=309) Spontaneous vaginal delivery Instrumental delivery |
36 (18.1%) 7 (7.5%) |
180 (83.3%) 86 (93.5%) |
|
History of perinatal death (N=309) Yes No |
34 (85.01%) 9 (3.4%) |
6 (15.0%) 259 (96.6%) |
|
APH (N=309) yes No |
9 (13.6%) 34 (14%) |
57 (86.4%) 209 (86.0%) |
|
Pre/eclampsia (N=309) yes No |
15 (17.6%) 28 (12.5%) |
70 (82.4%) 196 (87.5%) |
|
Obstructed lab (N=309) yes No |
7 (9.6%) 36 (15.3%) |
66 (90.4%) 200 (84.7%) |
|
PROM (N= 309) yes No |
14 (20.6%) 29 (12%) |
54 (79.4%) 212 (88%) |
During the data collection, 29 (9.4%) of babies born in hospitals were found to have congenital abnormalities, while 280 (90.6%) were not. Male births comprised 179 (57.79 percent), while female babies comprised 130 (42.1%). Of babies delivered in hospitals, 13.6 percent of multi-fetal pregnancies, whereas single-fetal births comprised 96.4 percent. The majority of the babies were born after 37 weeks of pregnancy (87.5%), while the rest (12.5%) were born before 37 weeks.
Table 3.
| Variables | NB Outcome | COR (95%CI) | AOR (95%CI) | p-value | |
|---|---|---|---|---|---|
| SB | Alive | - | - | - | |
|
Maternal age
< 35 ≥35 |
31 | 227 | 0.44(0.32-2.98) | 0.34(0.24-1.16) | 0.1 |
| 12 | 39 | 1 | 1 | - | |
| Regular ANC Yes No |
21 | 177 | 0.48(0.25-0.92) * | 0.46(0.22-0.95) * | 0.003 |
| 22 | 89 | 1 | - | - | |
| Preeclampsia/eclampsia Yes No |
15 | 70 | 1.50(0.76-2.97) | 1.30(0.44-3.85) | 0.09 |
| 28 | 196 | 1 | 1 | - | |
| PROM Yes No |
14 | 54 | 1.90(0.94-3.83) | 3.43 (0.98-12.03) | 0.067 |
| 29 | 212 | 1 | 1 | - | |
| Congenital malformation Yes No |
13 | 16 | 6.77(2.97-15.44)* | 3.39(2.501-13.33) * | 0.002 |
| 30 | 250 | 1 | 1 | - | |
| Hx perinatal death Yes No |
32 | 9 | 3.1(1.98-15.76) * | 2.96(1.59-6.14) * | 0.001 |
| 11 | 257 | 1 | 1 | - | |
| Spontaneous Preterm yes No |
15 | 47 | 2.5(1.24-5.49) * | 3.11(0.86-11.25) | 0.072 |
| 28 | 219 | 1 | 1 | - | |
| Obstructed labour Yes No |
7 | 66 | 0.58(0.25-1.39) | 0.49(0.12-2.05) | 0.096 |
| 36 | 266 | 1 | - | - | |
3.4. Magnitude of Stillbirth
Stillbirths accounted for 43 (13.9 percent) of all infants born in the study area, or 139 per 1000 live births. Stillbirths are the result of these pregnancies (29 and 14 of stillborn were males and females, respectively). The antepartum phase took the lives of 27 stillborn babies, whereas the intrapartum period took the lives of the remaining newborns. The majority of the babies were born after 37 weeks of pregnancy (87.5%), with the remainder (12.5%) born before 37 weeks of pregnancy Table 3.
4. DISCUSSION
4.1. Magnitude of Stillbirth
The fetal death rate is estimated to be 13.9 percent (CI, 10-18), meaning that 13.9 babies out of every 100 are expected to die. This is more than a study conducted in different parts of Ethiopia, such as Tigray's Ayder and Aksum, Southern Ethiopia's Yergalem Hospital, and Northern Ethiopia's Felegete Hiwot Hospital [12-14]. This discrepancy could be explained by a high flow case in the study area and the study's scope.
Furthermore, this result exceeds that of studies undertaken in India, Nepal, South Asia, and Ghana [15-18]. This discrepancy in our stillbirth rates compared to other hospitals could be attributable to a large volume of risky, delayed, and most troublesome cases from diverse distant places. Stillbirth is further increased by a lack of transportation, a lack of understanding of maternal health services, and a delay in seeking and receiving competent treatment [11].
The stillbirth rate in this study is lower than in a prior study in Somaliland [19]. The gap between this research area and Somaliland could be attributed to changes in service offered during antepartum and intrapartum care in the study settings, as well as differences in the early detection of serious diseases and problems, resulting in a lower stillbirth rate [20].
4.2. Factor Associated with Stillbirth
Mothers who give birth between the ages of 19 and 34 have a lower chance of stillbirth, according to this study, which is consistent with research conducted in low and middle-income countries, such as the Aksum General Hospital in Tigray and Anambra, Southeast Nigeria [3, 21, 22]. The reasons for the increase in stillbirth rates as mothers get older are unknown. Even in healthy pregnancies, the mother's age is associated with a higher risk of stillbirth. In older mothers, the rate of stillbirth rises as the gestational age exceeds 37 weeks [23]. They may be adequately informed on the course of pregnancy, labor, and delivery in terms of birth preparedness and complication readiness, as well as recognizing an antepartum fetal complication or pregnancy danger sign [3].
According to this study, mothers who receive regular prenatal care during their current pregnancy have a decreased chance of stillbirth than those who do not. It supports the results of a spatial and multilevel study carried out in JUSH southwest Ethiopia and other parts of Ethiopia [24, 25]. This could be due to a higher chance of detecting high-risk pregnancies throughout the prenatal period and the ability to react quickly and properly to any warning signs. The findings also imply that prenatal care should be prioritized [14].
According to this study, mothers who have had perinatal loss are ten times more likely than mothers who have not had a perinatal loss to have a fetal loss. This matches the findings of a study conducted in West Gojam in 2011 and 2012, as well as a study conducted in Dar Es Salaam's Three Municipal Hospitals [26, 27]. This might be a mother who has recently lost a newborn baby and feels obliged to replace the baby as quickly as possible. By lowering birth spacing, the desire to have another child sooner increases the risk of stillbirth [12, 28].
This research supports the findings of a study conducted in Kenya and Southwest Ethiopia, which found that congenital malformations are significantly linked to stillbirth [18, 29].
The absence of proper screening and diagnosis of congenital disabilities in infants could be explained in part by the lack of screening and detection of the conditions during the prenatal period. If this had happened, patients and clinicians could have been able to make decisions about interventions before the baby was born [30].
In this study, perinatal death was not significantly associated with pre/eclampsia, antepartum hemorrhage, and premature rupture of membranes, preterm birth, obstructed labor, and use of a partograph during labor, lack of formal education, and residency. Differences in sample size, research period, or study methodology could explain the disparity.
4.3. Strength of the Study
In the presence of financial limitation, the study was conducted. This title is very important to show the burden of stillbirth on newborn health, fewer than five children, and maternal health. Another, strength of this study was being a prospective study than a retrospective study.
4.4. Limitations of the Study
The study was limited to institutional delivery, which limits its ability to demonstrate the occurrence of community death because of financial constraints.
Furthermore, utilizing a cohort study design or observation rather than a cross-sectional analysis, we could not identify a cause-effect relationship between risk variables for stillbirth/fetal death.
CONCLUSION AND RECOMMENDATION
Lack of prenatal care, congenital fetal abnormalities, and prior perinatal loss were all significantly associated with stillbirth. Pregnant women should adhere to their prenatal care plan in order to reduce the risk of fetal loss by identifying both modifiable and non-modifiable reasons and treating them appropriately.
To investigate the prevalence of stillbirth in the community, the following researcher should conduct a cohort study that includes moms who give birth both at home and in a medical facility.
LIST OF ABBREVIATIONS
| ICD | = International Classification of Diseases |
| GA | = Gestational age |
| CI | = Confidence interval |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the ethical Review Committee of Haramaya University (Ref.no. IHRERC /021/878/2021.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used by the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013 (http:// ethics.iit.edu/ ecodes/ node/3931).
CONSENT FOR PUBLICATION
Verbal consent was obtained from each participant before the start of actual data collection. The confidentiality, privacy, risks, and being fit for the study were ensured. Furthermore, the participants were informed that they could withdraw from the study at any time.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The Data that supports finding of this study will be available upon reasonable request from the corresponding author [M.B].
FUNDING
None Declared.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We are grateful to Haramaya University for providing us with this opportunity. We'd also like to thank the North Shoa, Oromia Health Bureau. Special thanks go to hospital personnel, data collectors, supervisors, and study participants; without them, the research would not have been possible.


