All published articles of this journal are available on ScienceDirect.
The Utilization of Antenatal Care Services among the Pregnant Women in Somalia: A Scoping Review
Abstract
Background:
Women in Somalia suffer from one of the highest maternal mortality rates in the world. The good utilization of antenatal care (ANC) services significantly minimizes maternal and child mortality. The study aimed to identify the utilization of antenatal care services among pregnant women in Somalia.
Methodology:
We performed a scoping review based on the York methodology. This methodology entails a thorough search of published academic articles, conference proceedings, and grey literature via PubMed, Scopus, Google, and Google Scholar, focusing on English-language material.
Results:
Findings revealed that a significant number of Somali pregnant women utilize the ANC services, though not to the required number of visits as recommended by the WHO. Financial constraints, poor attitude of the healthcare providers, partner's attitude toward ANC services, lack of accessibility due to ANC services being far away, long waiting times, family matters, lack of awareness or media exposure, gravida, parity, and a good number of them believing that ANC is not necessary for their health were among the reasons given for an inadequate visit or non-utilization of the ANC services.
Conclusion:
The motivation to utilize ANC services, the initiation of visits within the early stages of pregnancy, and the completion of the required number of visits during pregnancy are crucial in preventing pregnancy-related issues and reducing maternal mortality. This must be encouraged among Somali women.
1. INTRODUCTION
About 303,000 women died in 2015 because of pregnancy and childbirth complications. Most maternal deaths occur in middle and low-income countries [1, 2]. Sub-Saharan Africa accounts for more than half of the cases [3]. Although maternal mortality rates have decreased globally, they remain too high, particularly in developing nations [4-11]. The main cause of death and disability in women of reproductive age is complications during pregnancy and childbirth [5, 6, 12-15]. Simple, affordable maternal care services, such as antenatal care (ANC), competent birth attendants, and postnatal care, might stop these pregnancy-related deaths [16-21]. Even though the use of ANC in underdeveloped nations has significantly increased, only a small percentage of pregnant women attend up to four ANC consultations [4, 22-26].
Between 2000 and 2017, maternal mortality decreased by over 38% globally, although the rate of maternal fatalities in sub-Saharan Africa is still high [5, 27]. About two-thirds of maternal deaths worldwide in 2017 [5] occurred in the sub-region. Records show that eight of the 15 nations regarded to be hotspots for maternal mortality were in sub-Saharan Africa. Somalia, the Central African Republic, the Democratic Republic of the Congo, Chad, Guinea, Zimbabwe, Nigeria, and Ethiopia are among these nations [5, 28]. Somalia was placed last out of 178 countries in the Save the Children Fund's 2014 annual worldwide report. According to the most recent estimates of the Somalia Health Indicators Report [29], the maternal mortality rate in Somalia in 2016 was 732 maternal deaths per 100,000 live births, ranking it among the highest in the world despite a decline from 1,044 in 2012 [29]. In addition, Somali women have been identified with an increased risk of adverse pregnancy outcomes, such as stillbirth and infant death [30, 31]. The UN interagency group's most recent estimates show that 69,000 Somali children and 4,800 mothers die each year due to poor health and ineffective healthcare systems [32].
In Somalia, antenatal care services utilization is very low; an average of 26.0% of pregnant women receive at least one antenatal visit during their last pregnancy [32]. Antenatal care (ANC) significantly minimizes maternal and child mortality through effective and appropriate screening, preventive, or treatment interventions [2]. In low and middle-income countries, ANC services significantly improve birth outcomes and lead to long-term reductions in child mortality and malnutrition [33]. Despite the vast maternal and child mortality in Somalia, there is minimal literature on the specific factors associated with mothers’ utilization of ANC and its consequences in Somalia. This study aimed to identify the utilization of antenatal care services among pregnant women in Somalia.
2. METHODOLOGY
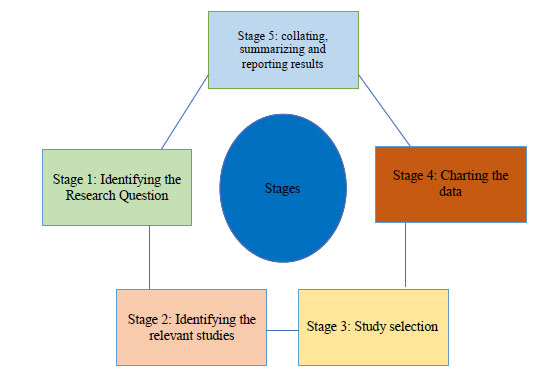
This review was performed based on the York methodology [34]. The York framework suggests five stages that we have followed for this review (Fig. 1).
2.1. Search Strategy
An initial search was conducted from February to June 2022 to identify the utilization of antenatal care services among pregnant women in Somalia. The comprehensive search of published academic articles, conference proceedings, and grey literature was conducted on Pubmed, Scopus, Google, and Google Scholar, focusing on English-language material [35, 36]. Additionally, grey literature search was done carefully from the relevant sources to identify published and unpublished studies not identified in the scientific databases. In the literature search, many articles were found from different sources. However, the titles and abstracts were screened against the established inclusion and exclusion criteria. The relevant full-text citations were retrieved and screened from the duplicates for final inclusion, and the discrepancies were resolved through the discussion.
2.2. Study Selection and Eligibility Criteria
The studies were included in this scoping review considering the criteria mentioned as follows: data on the utilization of antenatal care services in Somalia from 2012 onwards; any research articles or published relevant reports containing valuable information; and all studies (such as randomized controlled trials, quasi-experimental studies, cohort studies, case-control studies, cross-sectional studies, case reports, qualitative studies, etc.) containing information about the utilization of antennal care services in Somalia. We excluded all data older than ten years, non-English data, and information from countries other than Somalia. Restrictions were placed on publication dates to identify the most recent or current scenario for using antenatal services.
2.3. Synthesis
We analyzed and explored the utilization of antenatal care services among pregnant women in Somalia. The information on utilizing ANC services was gathered from the search sources, and the information was checked carefully to avoid duplications. The discrepancies were resolved through discussion. Finally, all results were summarized and reported.
3. RESULTS
Evidence reports more than 70-90% of Somali pregnant women to visit healthcare facilities at different stages of their pregnancy [4, 37, 38], with very few expectant mothers attending their first ANC during the first trimester of gestation [32]. Approximately, 50% of these women have been reported to observe their first ANC during the second trimester, while 25% during the third trimester of gestation [32]. It is established that more than half of the expectant women manage four visits, with approximately 2 to 3 visits, and less than 30% of them still requiring antenatal care services. Of the few who have not attended ANC, reasons given by them for the low number of visits or non-utilization of the ANC services include financial constraints, poor attitude of the healthcare providers, partner's attitude toward ANC services, lack of accessibility due to ANC services being far away, long waiting times, family matters, lack of awareness or media exposure, gravida, and parity; also, a good number of them believe that ANC is not necessary for their health.
It was identified in a recent study that few women could not afford to pay for ANC’s services. In addition, approximately 30% of pregnant women complained of extended waiting hours before being attended. Women who have experienced this in a previous pregnancy were discouraged from attending ANC services when getting pregnant again. However, women who were satisfied with the quality of ANC services were observed to have a high level of utilization of ANC services (five times more likely to utilize ANC services), which was found to be significant (OR: 5.1, P<0.05) [32]. On the other hand, approximately 20% reported poor services and attitudes of healthcare personnel [4].
Healthcare facilities at different levels (primary healthcare centers, hospitals, or private facilities) were found to be easily accessible to most Somali pregnant women with a distance range of fewer than 30 minutes to 1 hour [38] or less than 5KM [2]. However, most expectant mothers preferred private facilities. A discouraging element for some pregnant women was that most needed to travel on foot to get these services, and a few used public or private transportation [38].
Studies have shown marital status, living in a family, and source of income to be significantly associated with ANC services utilization of women, as mothers living with others have been reported to be more likely to utilize services compared to mothers staying alone (OR: 4.3, P<0.05). Furthermore, of the women who attended ANC, only a few decided on their own to attend ANC. At the same time, most of them were advised or motivated by their husbands or family members as well as encouraged by friends [38].
In addition, several pregnancies (gravida) were associated with the level of utilization of ANC services. Mothers who had more than 6 previous pregnancies were twice more likely to utilize ANC services than women with less than 5-(OR: 2.2, P<0.05) [32]. Of interest is that older women (≥25 years) mostly completed the recommended number of ANC visits (OR: 3.02; CI: 1.264-7.207). Other obstetric factors, such as the number of children (parity), were not significantly associated with the level of utilization of ANC services [32].
One of the significant factors that promotes the non-utilization of ANC services among Somali pregnant women is a lack of knowledge on the importance of ANC services and inadequate information on the required number of visits for ANC services. In addition, of course, educational status has been correlated with the utilization of ANC services. One of the significant consequences of the non-utilization of ANC services is the risk of losing the baby (perinatal mortality) or the mother during birth (maternal mortality) or both, as most pregnant women in this category tend to have home delivery. In addition, hemorrhage has been reported as the most common cause of death in these women, with approximately 40% of deaths occurring due to it [3].
4. DISCUSSION
The utilization of ANC services among Somali women has been found to be adequate. More than half of the expectant women have been reported to manage four visits; however, most have been observed to follow approximately 2 to 3 visits, thus not following the WHO's recommendations of a minimum of four ANC visits, with early commencement of the first visit within the first 12 weeks of the gestational period. This is despite the fact that healthcare facilities are accessible to most Somali women for gaining ANC services. This aspect was also emphasized in an earlier study [37]. This research stated that approximately 80% of the study participants lived within a distance of 5 kilometers or below from the healthcare facilities. However, a discouraging factor is that most women needed to travel on foot to get these services [38]. Also, most of these women preferred private facilities [2]. This observation is also similar to the study conducted earlier [37], which observed that approximately 60% of the women preferred a private facility. This may be ascribed to healthcare workers' adequate facilities and attitudes within the private facility.
Unaffordability of the ANC services, the attitude of health workers, and at most times, extended waiting hours are factors affecting the utilization of ANC services by a few pregnant women in Somalia, which is consistent with earlier reports [4, 37]. However, Abdillahi et al. [37] stated that drugs and transportation costs are affordable. Marital status, living with family, source of income, parity, and gravida were observed to be key contributors to the utilization of ANC services of women, in accordance with the previous findings [4, 16, 39].
Though it was documented that older women (≥25 years) and mothers who had more than six pregnancies mainly utilized and completed the recommended number of ANC visits, this did not follow the report provided by Mouhoumed & Mehmet [4], which stated the primigravida mothers to have undergone more ANC visits than multigravida mothers. A few Somali pregnant women reported the non-utilization of ANC services due to a lack of knowledge on the importance of ANC services and inadequate information on the required number of visits for ANC services. Furthermore, a significant association was recorded between knowledge (awareness) and utilization of ANC services [4, 40].
CONCLUSION
Findings generally suggest an adequate utilization of the ANC services among Somali pregnant women. Though, the reasons given by the few for non-utilization of the antenatal care services were partner’s attitude towards ANC services, affordability issues, non-attainment of education, maternal age, parity, wealth index, birth order, and non-media exposure, non-accessibility, and attitude of healthcare providers, among others. The initiation of ANC visits within the early stages of pregnancy and the completion of the required number of visits during pregnancy are essential in preventing pregnancy-related complications and reducing maternal mortality, which must be encouraged among Somali women.
RECOMMENDATIONS
The Ministries of Health at all levels and non-governmental organizations should develop sustainable efforts towards enhancing more utilization of the ANC services through media, including health talks, health education, and health promotion. Furthermore, the number of ANC visits should be enhanced by constructing more healthcare facilities within reach and, more so, improving clinical services and the attitude of healthcare personnel.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study was funded by Pan African university life and earth science, Funder ID. PAULESI/REG/21/116, Awards/Grant number. 2020/2021 scholarship scheme.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This paper is part of the partial fulfillment of a Ph.D. in reproductive health from the Department of Obstetrics and Gynecology, Pan-African University of Life and Earth Science Institute (PAULESI), University of Ibadan, Nigeria. The main author is grateful to the African Union for finding her worthy to be sponsored for the program. In addition, she wishes to extend her profound gratitude to the co-authors for their time and effort in making this piece of work a reality. This research will be supported by PAULESI and the African Union for African population studies.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


