All published articles of this journal are available on ScienceDirect.
Profile of Women Seeking an Intra-uterine Contraceptive Device at a Community Health Centre in Pretoria, South Africa
Abstract
Background:
An upsurge in demand for intra-uterine contraceptive devices (IUCDs) has led to this study, which focuses on the profile of women seeking IUCDs at a community health centre in Pretoria, South Africa.
Aim:
The study aimed to determine the profile of women seeking IUCDs at a Pretoria community health centre.
Setting:
The setting was Temba Community Health Centre in region 2 of Tshwane health district, South Africa.
Methods:
A descriptive quantitative study with a cross-sectional design was conducted using a piloted questionnaire.
Results:
Among the 129 participants, the mean age was 35 years (minimum 17 years, maximum 46 years). High participation was noted in the age group of 30–39 years (57.4%), single women (42.6%), those unemployed (54.3%), those with a secondary education (69%), and those with two children (62.8%). The decision to use an IUCD was based on its invisibility, lack of daily or sexual activity-related reminders, and lengthy device lifespan (100%). Before using an IUCD, many participants (32.6%) used condoms, and they were well versed in the IUCD. The primary source of knowledge on the IUCD was healthcare professionals.
Conclusion:
Women seeking IUCDs at a Pretoria CHC were mainly in the age range of 30–39 years, single, unemployed, with two children, using condom, and knowledgeable about the IUCD. The decision to choose an IUCD was backed by three key factors: it is invisible, there is no need for a daily or sexual activity-related reminder, and it lasts a long time without requiring a visit to the doctor. Healthcare professionals were the primary source of knowledge about IUCDs, and the knowledge regarding the device was scored as good among users at Temba CHC.
1. INTRODUCTION
1.1. Background
An intra-uterine contraceptive device (IUCD) is a T-shaped piece of equipment made of copper and plastic, which is meant to be inserted into the uterus in order to serve as a contraceptive. It is a commonly used form of reversible contraception that lasts for at least five to ten years. After being inserted into the uterus, the device's two threads pass through the cervix and remain in the vagina, making it simple to remove [1, 2]. The two primary types of IUCDs are non-hormonal metallic (copper) and hormonal levonorgestrel-releasing intra-uterine systems, such as the Mirena and Jaydess [3].
The mode of operation of the copper IUCD is that it releases copper ions into the uterine cavity, which are harmful to sperm entering the uterus and fallopian tubes [4, 5]. Levonorgestrel, a hormone secreted daily by the hormonal IUCD, thickens cervical mucous and lowers sperm motility and viability. Prior to the ovum entering the uterus, early in the reproductive cycle, the IUCDs largely impede fertilisation [4]. IUCDs cause a significant inflammatory response in the uterus. The presence of macrophages, leucocytes, prostaglandins, and other enzymes in both uterine and tubal fluid impairs the transfer of spermatozoa and ova [3, 6]. IUCDs are safe and appropriate for almost all women, including those who are married or otherwise, who do or do not have children, and who are young or older than 40. However, an IUCD is medically contraindicated in some circumstances, such as when active sexually transmitted diseases and pelvic inflammatory disease are present or cervical or uterine cancer [1, 5-7].
The South African primary healthcare facilities that provide the copper-T IUCD comply with the country's national clinical requirements. This contraceptive approach is inexpensive and has a low dropout rate. The use of IUCDs is comparatively low in low- and middle-income countries [8]. The use of IUCDs varies by country, with about 14.3% of women of reproductive age worldwide using IUCDs. However, the reasons for the variations are not well documented [9]. According to the United Nations (UN) and a study done in Nigeria, the number of women worldwide who rely on IUCDs increased from 133 million in 1994 to 159 million in 2019 [10, 11]. Some significant changes in methods occurred among women using some form of contraception during 2008–2014, with the largest change occurring among long-acting reversible contraceptive users [12]. While only 6% of women on contraception used an IUCD or subcutaneous implant as their primary method in 2008, this increased to 12% in 2012 and 14% in 2014 [12].
In India, more women who used IUCDs were unemployed; although the association between contraceptive use and employment was heterogenous considering the methods and sectors, there was no relationship between contraceptive use and a lower likelihood of employment [13]. Data from Demographic Health Surveys conducted between 1996 and 2000 in the 22 sub-Saharan African countries between 2010 and 2016 showed contraceptive use among married women to be increased in all of these countries. In the first period, the prevalence of IUCD use was less than 10% in 14 countries, and the mean for all countries was 11%. By the second period, IUCD use was lower than 10% in only four countries (Benin, Chad, Guinea and Mali), and the mean had risen to 24%, in part because of steep increases in most of the East African countries [14]. When assessing the profile of IUCD users in Nigeria, the participants’ ages ranged from 15 to 50 years, with most (56.4%) aged between 25 to 34 years and a mean age of 33.66 years. Most of the IUCD seekers were multiparous women (62.9%), 95.7% were Christian, and 95.7% were married [15]. Most (98.9%) of the respondents had formal education; 74.9% had a secondary level of education, 19.3% had tertiary education, and 4.7% had primary levels of education. With the majority having had secondary education, it was concluded that educated participants are more likely to accept the IUCD compared to those without secondary education [15]. A survey conducted in Ethiopia showed 3.1% of the IUCD users to be younger than 20 years, and most (93.8%) were married. More than three-quarters (79.6%) were Christian, while about 5.5% were found to be illiterate, and 40% had three or more births [16]. In South Africa, only about one-third of women aged 15–19 years used some form of contraception, with oral contraception accounting for 5.0% of use and IUCDs accounting for 0.4%, according to a national household survey conducted to evaluate contraceptive coverage among 6 296 women aged 15–49 years [17].
A study on the profile of IUCD users in Southern Nigeria showed that 77.9% of women obtained their information about contraception from clinical personnel, 9.7% from friends and relatives, 4.0% from community health workers, and 2.5% from print and media [3]. Radio/television and outreach contributed less as sources of information about contraception, at 1.8% and 1.5%, respectively [3]. In Ethiopia, the partner or husband’s approval (23.4%) as well as the service provider’s choice (33.6%) were the main factors supporting the use of IUCDs among many women [15]. Among Ethiopian women who had just delivered (they were in the early postpartum period), almost 42.6% showed good awareness of the IUCD [2]. In this group, 29.2% were informed by the media, 25.1% by healthcare professionals, 14.5% by family members/friends, and 4.3% by their husbands [2]. Another study carried out in Addis Ababa, Ethiopia, showed that 71.4% of the participants had information about the IUCD, and of those women, 32.1% reported having a husband, family and/or friend opposed to the utilisation of an IUCD. However, the source of information about IUCDs for the majority of the respondents was healthcare professionals (63.8%) [11]. In another Ethiopian study, conducted in Ambo, knowledge of IUCDs was assessed in women who had the intention to use a postpartum IUCD (PPIUCD), and 49% were found to have good knowledge of PPIUCD [2]. While 38.6% of the participants knew that a PPIUCD could prevent pregnancies for more than ten years, about 34.9% replied that they are not appropriate for women at high risk of contracting sexually transmitted infections (STIs) [2]. Only 24.1% had knowledge that the PPIUCD does not interfere with sexual intercourse or desire, and most (41.9%) knew that it could be removed at any time that they want it to be [2]. In addition, 61.2% believed that the PPIUCD does not move through the body after insertion, while 35.4% felt that the PPIUCD can interfere with sexual intercourse [2]. The majority (56.3%) of those polled disagreed that a PPIUCD could harm a woman's womb, while 27.5% believed that it does not cause cancer [2]. The knowledge and attitudes about IUCDs among reproductive-aged women in Saint Louis, Missouri, USA, were assessed, which showed that they had moderate knowledge on IUCDs. Most (98%) knew that STIs are not prevented by IUCDs. Conveniency (36%), pregnancy prevention (59%), and minimal side effects (28%) were the three most frequently cited reasons for using an IUCD [18].
In South Africa, in a study carried out to assess the quantity and quality of knowledge about the IUCD and to evaluate its acceptability for future use, even individuals who were aware of the existence of IUCDs had a lack of general information about them [19]. There was also a clear link between education and knowledge, with patients who had completed Grade 12 or higher being significantly more likely than those with lower levels of education to be aware of the IUCD. Several true or false questions demonstrated a lack of comprehension as well as myths about the IUCD in South Africa. The IUCD was thought to cause cancer by a third of participants (33.1%), and it was thought to move around in the body by 38.3%. About 41% of patients had no idea how long it would take to work [20].
When assessing the knowledge of contraceptives in Nepal, the majority of the participants (92.3%) had heard about contraception, whereas 7.70% had not [21]. The most well-known type of contraception was the injection (Depo-Provera – 92.7%), while pills and condoms were known by 91.7% and 89.6%, respectively. The IUCD was known by 69.4% of participants, while the implant, female sterilisation, and male sterilisation were known by 69.4%, 62.7%, and 57.5% of clients, respectively. Furthermore, abstinence was known as a contraceptive method by 39.4% of participants, withdrawal by 35.2%, the rhythm method by 11.4%, lactational amenorrhea by 8.8%, and EC by 23.3% [21]. IUCD users in Lagos University Teaching Hospital, Nigeria, showed that they had used other contraceptive methods before using the IUCD. Condom use accounted for 16.2% of users, the IUCD for 44.8%, oral contraceptives for 17%, injectable contraceptives for 19.5%, and sub-dermal implants for 2.5% [11]. Participants in a study, with respect to the knowledge of IUCDs and other contraception in South Africa, indicated that they had heard about tubal ligation (73.5%), male sterilisation (23.3%), the IUCD (49.2%), oral contraceptives (91.7%), and the progesterone-only pill (1.6%) [20]. Among others, 47.7% had heard about EC, 97.9% about the injection (Depo-Provera/Nur-Isterate), 99.5% about the male condom, 76.7% about the female condom, 1.6% about spermicides/jelly, 1.0% about the diaphragm/cap, 10.9% about hormone implants, and 6.2% about natural methods [20]. At Jubilee Hospital, Pretoria, it was found that the male condom was the most well-known contraceptive technique (98.4%), followed by the female condom (96.8%), the pill (96%), and the subdermal implant (82.9%) [22]. The least known method was the vaginal ring (6.40%), followed by the patch (11.10%), vasectomy (20.60%), calendar method (20.63%) and sterilisation (69.80). Among other methods that were known were the loop (73.00%) and withdrawal (79.37%) [22]. Regarding the IUCD, knowledge was assessed among women in more than 30 clinics of two South African provinces and found to be little, and emphasis was placed on educating women on this particular contraceptive method [17]. In Cape-town, South Africa, while assessing the awareness of and interest in the use of an IUCD in a population of HIV-infected women, it appeared that awareness in the chosen sample was around 37%. After an IUCD information meeting, more than 34% showed interest in the use of the device; this interest was inversely linked with the age of the participants and slightly related to existing menses complaints [23].
1.2. Aim and Objective
The aim of the study was to determine the profile of women seeking to use IUCD at a Pretoria community health centre (CHC). The study's objectives included identifying the socio-demographic characteristics of the participants, their motivations for choosing the IUCD, the sources of information they used to learn about the device, their prior use of contraceptive methods, and their knowledge of the IUCD.
2. MATERIALS AND METHODS
2.1. Study Design
A descriptive quantitative study was carried out with a cross-sectional design using a piloted questionnaire.
2.2. Population Sample and Sampling Size
From June 2021 to December 2021, all women seeking an IUCD at Temba CHC were considered for the study. The sample was drawn from those who signed assent (under 18 years of age) and consent (above 18 years). The Temba CHC registration data show that every week, roughly five women request an IUCD. After six months, a sample size of 120 was estimated; however, a higher number of participants was received during data collection, with a 10.8% increase in sample size (n=129).
Inclusion criteria were women of childbearing age (15–49 years) requesting an IUCD at Temba CHC during the data collection period. Exclusion criteria were sick and mentally disturbed women who need urgent medical care and virgin women.
2.3. Data Collection
The researcher trained a retired female nurse who had previously worked in Temba CHC's mother and child section to be a research assistant (RA). The RA was based at the designated unit from the start of the data-collecting period until its conclusion, per the agreement. Her responsibility was to describe the study's aim and objectives to all women seeking an IUCD. She helped them to sign the consent forms (for those who consented) and got in touch with parents or guardians so that assent could be signed for minors who agreed to participate in the study. The two languages that are used in the Temba community, Setswana and English, allowed the RA to express herself. The researcher created the questionnaire in English, and the RA gave it to the study participants who consented. The questionnaire was divided into five sections: socio-demographics, motivation for choosing IUCD, source of information on IUCD, previous contraceptive methods used, and knowledge of IUCD. Before being used in the current survey, this questionnaire underwent testing in another CHC situated about 65 km from Temba CHC.
2.4. Reliability and Validity
To ensure reliability in the current research study, the questionnaire was tested for stability using a test-retest. The same questionnaire was given to the same participant more than once under similar circumstances. During the pilot study, a few candidates (n= 6) who came to the pilot center to book for IUCD insertion completed the questionnaire, and when they came back a week later for the IUCD insertion, they were given the same questionnaire to complete. Their answers were similar to the ones they had provided a week previously. This was taken as evidence of the consistency and that the questionnaire should provide the same outcomes if repeated in similar circumstances.
In addition, content validity, as well as face validity, was assessed. In terms of content validity, the questionnaire covers all aspects of IUCDs as presented in the objectives of the study. After the pilot study, the questionnaire was restructured by the two supervisors to match the different objectives of the study. Regarding face validity, the questionnaire was peer-reviewed by two family physicians who are not part of the current study project.
The pilot study was conducted in Phedisong 4 CHC, which is 65 km away from Temba CHC in Ga-Rankuwa. The researcher made an effort to reduce data contamination by keeping this distance. It is a CHC like Temba, and the majority of its users speak Setswana and English. They also share the same culture, food, and languages as the Temba locals.
2.5. Data Analysis
The information from the completed questionnaires was captured on an Excel spreadsheet. Coding of data was done in order to use only numerical data in the statistical analysis. Data were imported into the Statistical Package for the Social Sciences (SPSS) software version 27 for descriptive analysis. Results of this analysis are presented in tables and Figs. (1-3).
2.6. Ethical Considerations
Before starting data collection, the researcher secured a letter of approval from the Temba CHC Operational Manager and an ethical clearance certificate from the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC/M/32/2021: PG). The Tshwane District Research Committee also granted permission to conduct the study (project number 13/22). Anonymity and confidentiality were maintained throughout the entire research procedure. No proof of identification was required. Before enrolling a participant, their written assent or consent was required. The study's participants were informed about their right to leave the study at any point if they felt uncomfortable; however, no participants dropped out.
3. RESULTS
Among the 129 participants, the mean age was 35 years (minimum age 17 years, maximum age 46 years). High participation was noted in the age group of 30–39 years (57.4%). Most participants were unemployed (54.3%), with a secondary education level (69%), single (42.6%), and having two children (62.8%) (Table 1).
| Age (in years) | Percentage |
|---|---|
| < 20 | 2.3 |
| 20–29 | 16.3 |
| 30–39 | 57.4 |
| >39 | 24.0 |
| Total | 100.0 |
| Employment Status | |
| Employed | 45.7 |
| Unemployed | 54.3 |
| Total | 100.0 |
| Education Level | |
| No formal education | 2.3 |
| Primary education | 5.4 |
| Secondary education | 69.0 |
| Tertiary education | 23.3 |
| Total | 100.0 |
| Marital Status | |
| Single | 42.6 |
| Married | 37.2 |
| Divorced | 12.4 |
| Widow | 7.8 |
| Total | 100.0 |
| Number Of Children | |
| No children | 6.2 |
| One child | 10.8 |
| Two children | 62.8 |
| Three or more children | 20.2 |
| Total | 100.0 |
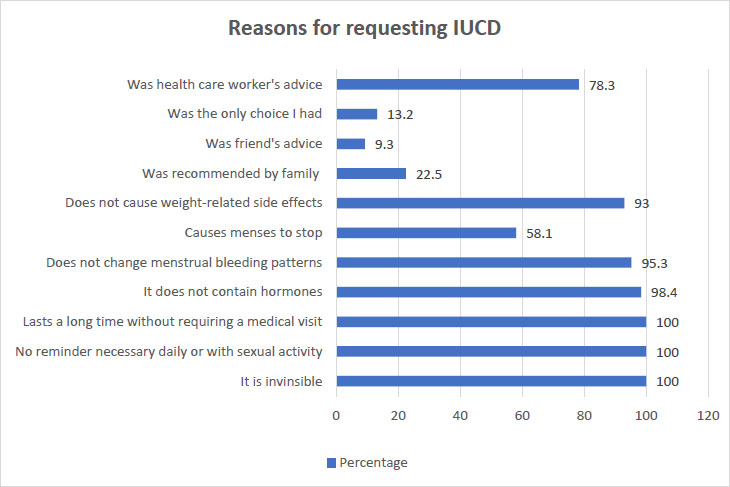
The majority of the participants chose an IUCD because it is invisible, does not need daily reminders, and lasts for a long time without requiring a medical visit (129 or 100% for all three reasons).
| Aspect of knowledge of IUCD | Yes | No | Not sure |
| 1. Does not cause weight-related side-effects | 98.4% | 1.6% | 0% |
| 2. Cause mood changes | 98.4% | 1.6% | 0% |
| 3. It is invisible | 96.9% | 2.3% | 0.8% |
| Increase the risk of contracting sexually transmitted infections, including HIV | 100% | 0% | 0% |
| 4. Cause infertility in women | 93.0% | 3.9% | 3.1% |
| Can be used by women of any age, who have children or who have not | 87.5% | 10.9% | 1.6% |
| 5. No daily or sexual activity reminder needed | 100% | 0% | 0% |
| 6. Can cause cancer | 86.8% | 9.3% | 3.9% |
| 7 .Does not move to the brain or heart | 73.6% | 17.1% | 9.3% |
| 8. Does not cause discomfort or pain to the woman or the man during sex | 65.9% | 31% | 3.1% |
| 9. Lasts long without requiring a medical visit | 96.9% | 3.1% | 0% |
| 10. Does not change menstrual bleeding patterns | 97.6% | 0.8% | 1.6% |
| Total in percentage | 91.3% | 8.7% | |
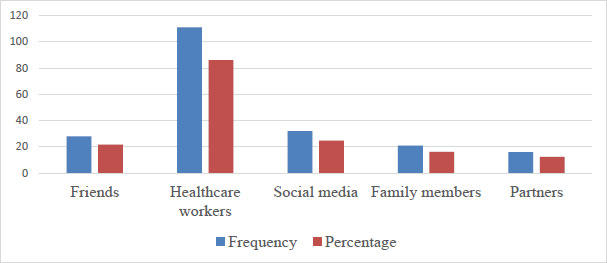
The majority of the participants obtained their information about the IUCD from healthcare workers (86.0%), while 24.8% got it from social media.
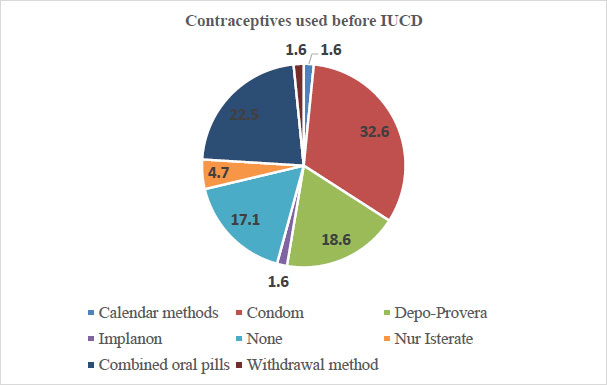
The most previously used contraceptive was the condom (32.6%), followed by combined oral contraceptives (22.5%) and the Depo-Provera injection (18.6%).
In this study, knowledge of the IUCD was assessed based on the 12 elements presented in Table 2. A response of ‘Yes’ expressed the participant’s knowledge of the element; for instance, all of the participants (100%) knew that the IUCD needs no daily or sexual activity-related reminder.
In terms of knowledge scores, two groups were created from the three columns of participant responses: the ‘Yes’ responses made up the first group, while the ‘No’ and ‘Not sure’ responses made up the second group. The combined ‘No’ and ‘Not sure’ answers were viewed as being a poor knowledge score, while all ‘Yes’ responses were good and made up a good knowledge score. The total of all ‘Yes’ responses was 91.3%, while the total of all ‘No’ and ‘Not sure’ responses was 8.7% (Table 3).
| Knowledge Scores | Percentages |
|---|---|
| Good | 91.3 |
| Poor | 8.7 |
4. DISCUSSION
Even if not all of the statistics for IUCD is the same across the world, the differences between them are not very large. For instance, the average age of device users is consistent across studies, including in the current study and that conducted in Southern Nigeria, despite disparities in the age groups that use the device around the world [15]. The UN disproved the idea that there is a relationship between women's marital status and gadget use by finding that single women appeared to use the device more frequently than their married counterparts [10, 15, 17]. This conclusion seems to be in line with the Temba findings, given that almost half of the participants were unmarried. Since the findings are not linked to particular causes [9], additional investigation is recommended to ascertain the reason for these consistencies. Contrary to the current study and that carried out in Nigeria, users of the gadget in Ethiopia were younger and married; however, there was consistency in terms of parity because many participants in all of these studies had one or more children [16]. More unemployed women were reported to request for the IUCD at the Temba CHC, as demonstrated in the findings. This is consistent with the findings of a study conducted in India [13]. In South Africa, this should not be an issue since the government provides the device free of charge; therefore, unemployment cannot be a barrier when a woman requests the IUCD.
Regarding the participants' educational background, more South African women had a secondary school education, as shown in the current study and the Free State survey [17]. This finding may be connected to what Van der Westhuizen and Hanekom (2016) found in a different South African study, which indicated that there is still a significant lack of qualitative knowledge [20]. As a result, education about contraception is crucial to ensure that all women, regardless of their educational background, are aware. Since the device is also the source of myths, as another South African study noted (Hlady, 2011) [18], this education can address the general public's lack of understanding of the IUCD. For instance, women in this study thought the gadget to cause cancer, while another group of South African women discussed how it moved through the body [18].
The majority of Temba women gained knowledge on the IUCD firstly from the healthcare professionals and secondly from social media. However, in other countries, such as Ethiopia, the partners played a great role in the matter [2]. There has been no consistency observed regarding the source of knowledge on the IUCD [16], and the choice in Temba was influenced by a number of factors, such as the fact that it is invisible, does not need reminders (unlike the pill and injectables), and lasts for a long time. The strength of this study lies in its findings, which are based on primary data that reflect how the participants felt about the IUCD. However, since not all Temba women of reproductive age participated, the study cannot claim to represent a complete picture of IUCD use in the community.
CONCLUSION
Women seeking IUCDs at a Pretoria CHC were mainly in the age range of 30–39 years, single, unemployed, with two children, using condom, and knowledgeable about the IUCD. The decision to choose an IUCD was backed by three key factors: it is invisible, there is no need for a daily or sexual activity-related reminder, and it lasts a long time without requiring a visit to the doctor. Healthcare professionals were the primary source of knowledge about IUCDs, and the knowledge regarding the device was scored as good among users at Temba CHC.
RECOMMENDATION
The main source of information on the IUCD has been identified as the healthcare professionals; therefore, ongoing education of patients by healthcare professionals will significantly improve the usage of the IUCD and dispel common misconceptions about the device in other health facilities with poor uptake. Additional platforms may also be used to convey information on IUCDs, such as social media and workshops for women at various venues, such as secondary schools, at various organisations that employ women, at various clinics and CHCs, and the like.
LIST OF ABBREVIATIONS
| IUCDs | = Intra-uterine Contraceptive Devices |
| CHC | = Community Health Centre |
AUTHORS’ CONTRIBUTIONS
AMM and TB shared all tasks from the conceptualisation through protocol development, pilot study, and data gathering, to article writing.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The researcher secured a letter of approval from the Temba CHC Operational Manager and a clearance certificate from the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC/M/32/2021: PG). The Tshwane District Research Committee also granted permission to conduct the study (project number 13/22).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the human procedures used were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Informed consent was sought from the participants before participating in the study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Sr Seleka TJ from Temba CHC, who assisted with data collection.


