All published articles of this journal are available on ScienceDirect.
The Economic Crisis (2008-2019) and Health Care in Zimbabwe: A Structured Literature Review
Abstract
Background:
The multi-prolonged nature and severity of the economic crisis (2008-2019) in Zimbabwe provided a distinct prospect to analyse the impact of economic crisis on the healthcare system. According to the System Model, the possible effect on health infrastructure, material resources, human resources, and financial resources is relevant.
Aim:
The structured literature review aimed to conduct an analysis of available evidence referring to the impact of economic crisis on health care in Zimbabwe between 2008 and 2019.
Methods:
A search of publications in English with inclusion criteria of timeframe between January, 2008 and December, 2019 that referred to the effect or impact of the economic crisis on health care was conducted utilising databases, such as Google Scholar, EBSCOhost, Pubmed, and UNISA repository. A thematic analysis for data extraction and synthesis was carried out. Exclusion criteria referred to irrelevance to the objectives and inappropriateness.
Results:
A total of 87 research publications were identified on various databases for analyses, 75 were excluded at different stages of screening, and 12 were included in the study. The thematic analysis, conducted according to the steps explained by Tesch (in Creswell 2014), revealed economic effects on health care in four themes: public health infrastructure, health workers, medical drugs, and public health expenditure and management, which were affected by an economic crisis.
Conclusion:
The effects of the economic crisis were evident in terms of negative changes in the healthcare delivery system, including a reduction in medical drug supply, loss of human resources, reduced financial resources, and an increase in the disease burden.
1. INTRODUCTION
Zimbabwe has been affected by a political crisis that translated into the most severe economic crisis in its history from 1999 to 2008, which led to the signing of the Government of National Unity in 2008 [1]. One researcher experienced this crisis personally as a Zimbabwean, thus becoming the motivation and support for this review. After the dollarizationin 2009, Zimbabwe felt an economic rebound that lasted until 2012 before the economy started dwindling [2]. The negative effects on health care resources in Zimbabwe were evident as the population failed to receive health care services [3, 4]. The economic crisis resulted in the deterioration of health infrastructure, such as health facilities, resulting in the closing of some public health facilities, either due to a lack of medical supplies and health workers or financial resources for the maintenance of health facilities [5, 6].
Health facilities that were able to function experienced shortages of medical drugs and material resources, such as cotton wool, bandages, sutures, and medical needles, which are crucial in the offering of quality healthcare [5, 7].
Zimbabwe lost, during this time, large numbers of healthcare workers, including professional nurses and physicians [8, 9]. Zimbabwe has 1.6 physicians for every 10,000 people, against World Health Organization (WHO) recommendations of at least one physician per 1000 population needed to meet the Sustainable Development Goals [10]. Professional nurses (State Registered Nurses (RGN) and State Certified Nurses (SCN)), the key human resources for offering health care in rural areas of Zimbabwe, were not spared, as the many RGNs left Zimbabwe in search of better opportunities [8]. The nurse ratio per 1000 of the population decreased from 2.5 in 2017 to 1.95 in 2019 [9]. The numbers are expected to decline due to economic hardships, forcing nurses to look for other opportunities [10]. In addition, the healthcare system was overwhelmed by intermittent strikes by health workers due to low remuneration and poor working conditions, including a lack of medical equipment [3, 11]. The disease burden increased, including a Cholera outbreak in 2008, where 98,585 cases were recorded, with a 4.1% fatality rate, contributing to the loss of 4,000 lives [9]. The Covid-19 pandemic that started in 2020 could not have been any less devastating to the economy of Zimbabwe. The exposure to public health risks in Zimbabwe already contributed to high maternal mortality rates of 651 per 100,000 live births [12].
The decline in vital health statistics was a sign of a reduction in the allocation of financial resources for health care, contributing to an increase in household and individual expenditure on health care [13] and negatively affecting access to health care for those who cannot afford it [14]. Literature provided evidence on the healthcare effects of economic decline in other countries [15]. However, very few focused exclusively on the ongoing economic crisis in Africa, particularly Zimbabwe.
Therefore, this structured literature review aims to provide evidence from published literature pertaining to the effects of the economic decline in Zimbabwe on health care without appraising the quality of the methodologies followed but focusing on the criteria for inclusion determined by the researchers, as explained below. The objective was to review the published literature on the economic crisis and healthcare decline in Zimbabwe and its effects on physical, human, and financial resources. Access to healthcare is a basic human right that needs investigation if it becomes limited or negatively affected.
2. METHODS
A structured review, defined as a review of an evidently framed question that methodical and reproducible approaches to ascertain, choose and analytically evaluate all relevant research [16, 17], was carried out. The structured review of published literature related to the consequences of the economic crisis on health care performed with specific reference to the economic crisis in Zimbabwe was done in 2020. Usually, because of the heterogeneity of the applicable literature that addresses economy, different from clinical trials, such reviews depend on a qualitative analysis of the related studies compared to a meta-analysis [17]. The data collection and analysis were in accordance with the steps provided by Armitage and Keeble-Allen [17], which are (1) an electronic literature search, (2) the selection of papers corresponding with the criteria identified by the researcher, (3) the extraction of data from the selected papers, and (4) the analyses of the selected papers.
2.1. Search Strategy
Online databases, namely the UNISA repository, Google Scholar, PubMed, and EBSCOhost, were searched by the researcher. The keywords used to search the database were 'economic decline and Zimbabwe', 'economic crisis in Zimbabwe’, 'economy crisis and health care’, as well as 'health effects and economic crisis’. Several references, referred to in the found publications, were hand searched to find other possible publications. The original search was conducted by a librarian appointed as the subject specialist.
2.2. Inclusion and Exclusion
Articles published in English between January, 2008 and December, 2019 were selected. The time frame chosen was specifically due to the political environment that led to the economic crisis. Editorials, commentaries, and correspondence that reported on the effects of the economic crisis on health care were also considered acceptable for inclusion.
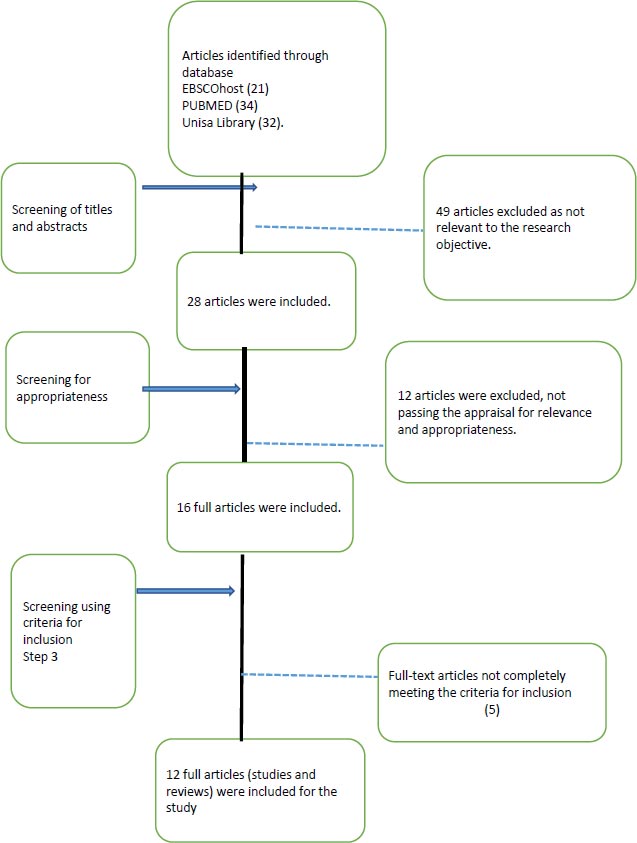
The decision on the inclusion or exclusion criteria was based on the principle of including all studies of relevance to the economic crisis and was broadly defined to avoid the probability of excluding hypothetically relevant studies [18]. Considering the relevance, 86 publications were reviewed by title and abstract by researchers interested in health research in developing countries to contribute to the rigor of the selection (Fig. 1).
Forty-nine (49) articles were excluded during the first review by title and abstract, leaving 27 for further screening. The researcher and 2 co-researchers individually did a full article review on these 27 articles for appropriateness, after which 12 articles were excluded. The review and selection process for the remaining 15 published articles was conducted using the inclusion criteria determined by the researchers, as proposed by Armitage and Keeble-Allen [17], to be considered appropriate and relevant for the study. This led to the inclusion of a final 12 articles after an agreement between the three researchers. This was after they individually and then jointly assessed the relevance and appropriateness of the selected articles (Table 1). In a structured literature review, quality is not always considered, as articles are selected based on relevance [17]. Therefore the quality of the articles per se was not the ultimate goal for inclusion in the review.
3. DATA EXTRACTION
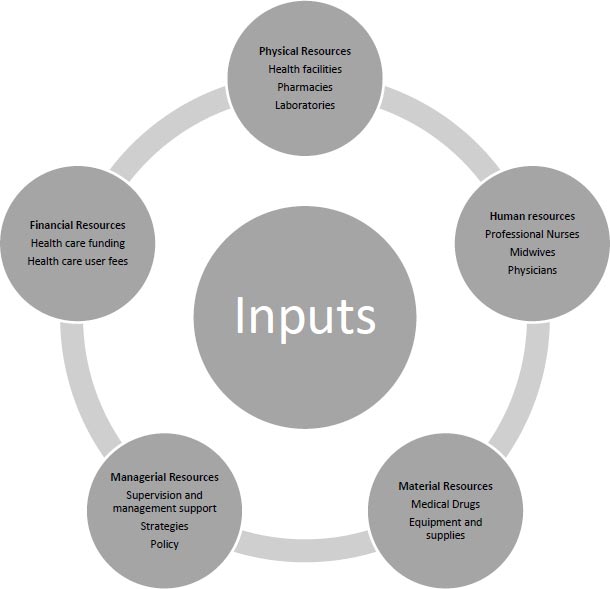
Data extraction and analysis were based on the inputs needed for enhancing access to healthcare as indicated within the Systems Model as described by Van Olmen et al. [19]. The researchers extracted the main outcomes of all the selected studies using a structured process following the Systems Model inputs. The extracted data was based on the settings, methodology, participants, aims of the research studies and reviews, and main findings (Table 2).
A healthcare system depends on well-organized inputs like physical, material, human, financial, and managerial resources (System Model Inputs) [19]. These inputs are key to enhancing access to health care; thus, researchers found it appropriate to use the System Model (Fig. 2) inputs as the basis for the thematic analysis of the findings and discussions of the selected articles (Table 3).
| Publication | Overall Quality | Aims and Objectives | Ethical Clearance | Data Gathering and Analysis | Findings and Conclusions | |
|---|---|---|---|---|---|---|
| 1 | Faramarzi et al. 2018 | Good | Yes | Not included | Yes | Yes |
| 2 | Levy and Sidel. 2009 | Good | Yes | Not included | Yes | Yes |
| 4 | Suhrcke et al., 2011 | Good | Yes | Yes | Yes | Yes |
| 5 | Karanikolos et al., 2013 | Good | Yes | Not included | Yes | Yes |
| 6 | Leach-Kemon et al., 2011 | Good | Yes | Yes | Yes | Yes |
| 7 | Kirigia et al., 2011 | Good | Yes | Not included | Yes | Yes |
| 8 | Modrek et al., 2013 | Good | Yes | Yes | Yes | Yes |
| 9 | Nunes et al., 2015 | Good | Yes | Not included | Yes | Yes |
| 10 | WHO 2014 | Good | Yes | Yes | Yes | Yes |
| 11 | Simou and Koutsogeorgou, 2013 | Good | Yes | Yes | Yes | Yes |
| 12 | Chimhowu et al., 2010 | Good | Yes | Not included | Yes | Yes |
| 13 | Tapera et al., 2019 | Good | Yes | Yes | Yes | Yes |
| Publication | Country/Settings | Methods | Participants | Aim/Purpose | Findings |
|---|---|---|---|---|---|
| Faramarzi et al., 2018 | Eastern Mediterranean countries | Literature and narratives | Literature and narratives from researchers | To assess the association between healthcare resources and economic crisis. | The economic crisis led to a significant reduction in healthcare resources in countries dependent on “out-of-pocket” financing. |
| Levy and Sidel., 2009 | Global | Literature and narratives | Literature and narratives from researchers | To determine the relationships between the economic crisis and public health. | The financial crisis contributed to challenges faced by the health sector due to the limited allocation of resources. |
| Suhrcke et al., 2011 | Globally | Literature and narratives | Literature and narratives from researchers | To gain a better understanding of the interrelationships between economic crises and infectious disease. | The long-term impacts of economic crises on infectious disease are inevitable as considerable evidence suggests that the magnitude of the effect depends significantly on government budgetary reactions. |
| Karanikolos et al., 2013 | Europe | Literature and narrative reviews | Literature and narratives from researchers | Impact of the financial crisis in Europe. | The financial crisis poses risks to health care, but the fiscal austerity leading to economic shocks and weak social protection needs controlling to reduce the impact on health and social crises in Europe. |
| Leach-Kemon et al. 2011 | Global (developing countries) | Literature and narratives | Literature and narratives from researchers | To determine the impact of the financial crisis on global funding to developing countries for health improvement. | The growth of funding slowed down due to the economic crisis, affecting funding for healthcare systems in developing countries. |
| Kirigia et al., 2011 | WHO Africa Region countries | Cross-sectional survey | Ministry of health directors | To determine if the economic crisis can influence health outcomes through the social determinants of health. | The economic crisis contributed to inefficiencies in the use of resources allocated to health facilities for the purchase of medical drugs and the misuse of global health funds at the expense of the healthcare system. |
| Modrek et al., 2013 | Global | Literature and narratives | Literature and narratives from researchers | To determine the effects of recessions on the health care system. | There was evidence that recessions had an impact on health infrastructure leading to the outbreak of infectious diseases and communicable diseases (basic public health infrastructure breaks down). |
| WHO. 2014 | Europe | Literature and narratives | Literature and narratives from researchers | To review the health implications of the financial crisis. | The economic crisis has negative health effects on resources, such as material resources (medical drugs), human resources (health workers), and those who lose their jobs. This would result in inaccessibility to health care. |
| Nunes et al., 2015 | Portugal | Literature and narratives | Literature and narratives from researchers | The main goals of this study were to reflect on the economic recession and its impact on health care. | The authors concluded that health care depends on economic redistribution and, in this context, needs to be equitable and fair. |
| Simou and Koutsogeorgou, 2014 | Greece | Literature reviews | Literature and narratives from researchers | To present a systematic overview of the effects of financial crisis on health and healthcare. | Factors associated with the financial crisis and the effects on health care were identified, focusing on reductions in public health expenditure and changes in healthcare services and the pharmaceutical market, with an increasing number of admissions in the public healthcare sector. |
| Chimhowu et al., 2010 | Zimbabwe | Literature and narratives | Literature and narratives from researchers | To assess the impact of economic decline on health care in Zimbabwe. | The economic decline contributed to the inaccessibility of health care by the majority of impoverished Zimbabweans. |
| Tapera et al., 2019 | Zimbabwe | Literature and narratives | Literature and narratives from researchers | Investigate health system constraints, affecting treatment and care by women in Zimbabwe. |
The economic challenges contributed to limited affordability and availability of drugs and accessibility of treatment facilities that challenged the accessibility of health facilities. |
| Theme | Category | Subtheme |
|---|---|---|
| Physical resources | Health facilities Road maintenance |
• Inaccessibility to health facilities in Zimbabwe due to the distance between villages and health facilities. • Status of existing health facilities, either functioning or non-functioning. • The status of the infrastructure. • The status of the conditions of the roads. • Unavailability of bridges along the roads. |
| Material resources | Medical drugs Medical equipment |
• Unavailable medical drugs at the health facilities. • Lack of adequate supplies of medical drugs. • Unaffordability of medical drugs by health care users. • Non-functioning of available medical equipment. • Unavailability of medical equipment. • Poor maintenance of medical equipment. |
| Human resources | Health workers | • Decreased in numbers of: ♦ Professional nurses ♦ Midwives ♦ Physicians |
| Financial resources | Public health expenditure and management | • Limited annual health budg et al. location below the 15% threshold agreed upon during the Abuja Declaration of 1979. • Non-prioritisation of the health budg et al. location during annual budget planning. |
From the 87 publications (21 in EbscoHost, 34 PubMed, 32 in Unisa library) that were originally identified using the electronic search process and research platforms (Fig. 1), twenty-eight (28) articles were selected for possible inclusion. A step-by-step process was followed, as indicated in Fig. (1), to ascertain the final 12 articles for inclusion.
3.1. Summary of the Included Studies
All twelve (12) publications included addressed the economic crisis and its implication on the health care resources, namely on the physical resources, material resources, human resources, and financial resources that could be impacted by the economic crisis.
In the publication by Faramarzi et al. [20], an analysis of the economic crisis as an essential socio-economic factor for healthcare resources and its association with several health outcomes was described. Unemployment rates and out-of-pocket expenditure were taken as important predictors of accessibility of health care (financial resources input). The economic crisis contributed to a decrease in health care resources for Eastern Mediterranean countries as economic decline affected employment, which, in turn, affected health funding. During the economic decline, the out-of-pocket contributions by the health care users were financing 58% of the health care services, resulting in a negative impact on health outcomes.
Levy and Sidel [21] indicated that healthcare budgets were cut due to the economic crisis, affecting access to health workers, availability of medical drugs, and accessibility of private and public health facilities. The economic crisis resulted in reduced financial support for public health care programs, affecting the control of diseases and mortality rates negatively in 2008 in the United States of America. The economic crisis contributed to unemployment, affecting access to affordable medical care insurance by healthcare users.
In the study by Suhrcke et al. [22], it is described that the economic crisis affected most of the System Model inputs. The authors mentioned the cut in the health budget that affected the availability of health infrastructure. Pharmaceutical companies reported a decline in sales and production of medical drugs; thus, health facilities failed to access medical drugs. Health workers were downsized, and available health workers failed to take sick days, affecting quality health care delivery. The financial support was cut from both internal and external funding sources, risking disruption of treatment and/or the exacerbation of drug resistance as medical drugs were unavailable.
Karanikolos et al. [23] revealed that the economic crisis in Europe resulted in changes to public health expenditure, affecting human resources and the availability of medical drugs and medical supplies. For example, some countries like Cyprus, Greece, Ireland, Lithuania, Portugal, and Romania stopped the recruitment of health workers and froze salaries of health workers, leading to a brain drain. Some health facilities were closed, and reductions in the number of hospital beds and working hours were recorded in some countries like Catalonia. In addition, the price of medical drugs increased, making it merely impossible for pensioners and those who lost employment to afford health care, and default rates increased, particularly for chronic patients.
Leach-Kemon et al. [24] mentioned that the global financial crisis affected internal health funding in most countries, despite increased bilateral donors of 4% funding for health care during the economic crisis between 2008 to 2011. The amount of health resources available and the financial support for medical drugs and medical equipment that contributed to both public and private health institutions between 1990 and 2011 were described in this publication. The UN funding for health stagnated between 2008 and 2011, while malaria and tuberculosis stopped affecting healthcare resources in developing countries. These might have prompted bilateral donors to increase funding to developing countries. The financial resources were inadequate to address the effects of economic crisis on health facilities, human resources as well as material resources needed for quality health care.
Kiriga et al. [25] found ample evidence that in Asia and Latin America, the economic and financial crisis resulted in cuts in expenditures on health care, lowering the utilisation of health facilities, loss of health workers, reduction in maintenance of medical equipment, reduced access to medical drugs and other operating expenditures related to disease surveillance or supervision. In 2008, 15 of the 46 countries in the WHO African Region devoted less than 5% of their gross domestic product (GDP) to health. While five countries were above 9% of their GDP, total government expenditure on health in the region varied from 11% downwards, and five countries met the Abuja target of allocating at least 15% of the government budget to health. The reduced GDP available for health implied cutting budg et al. location to health worker remunerations, medical drugs, health facility renovations, and medical equipment and supplies with devastating effects on health care.
In a study by Modrek et al. [26], the consequences of the economic crisis on health indicated consistent evidence that recessions led to unemployment, which, in turn, significantly affected access to health workers, affordability to access medical drugs, and accessibility to health facilities for young men. The healthcare budget was cut, affecting the maintenance of hospitals and rural health facilities negatively. It was noted that the economic crisis contributed to a rise in mortalities because of infectious diseases, which could not have been treated effectively due to a lack of medical drugs, health workers, and financial resources to access health care.
Nunes et al. [27] reflected on the economic crisis and its impact on health care, demonstrating the influence of nursing on the sustainability of health care. The economic crisis limited the capacity of health workers to develop and deliver high-quality care due to a lack of material resources and financial resources, thus negatively affecting their performance.
Economou et al. [28] indicated that an economic crisis negatively affected public health care as financial resources were reduced, affecting healthcare activities and resources that facilitate healthcare delivery. In most developing countries, the health care budget is vulnerable and is normally the first to be affected during an economic crisis, leading to overstretching of the public health care system. In times of economic crisis, accessibility to healthcare services is reduced while demand increases, health workers are overloaded and medical drugs are in short supply. A significant increase in people reporting unmet medical and dental needs was noted due to dwindling financial resources for health.
Simou and Koutsogeorgou [29] presented a systematic overview of the consequences that the financial crisis has had on health and health care in Greece. Reduction in public health expenditure was associated with reduced access to health care services, access to medical drugs, and an increase in hospital admissions. The reductions in healthcare budgets after 2009 resulted in more people failing to access healthcare. The remuneration of the health workers was cut by 15%, and health workers resigned, creating shortages and overloading of available health workers. This affected operations at the primary healthcare level. Some health facilities were closed in Greece, and prices of medical drugs were also increased, affecting access by the unemployed.
Chimhowu et al. [1] found that the allocation of the health budget was virtually worthless, and people were struggling to access health care in Zimbabwe. The economic crisis affected health infrastructure capital investment while the population was increasing. As lower-level health facilities were closed, referral centres like provincial and central hospitals were used as the first referral centres, causing congestion and a fall in the quality of health care services offered. Medical drug supply and health workers became scarce. The cost of medical drugs increased, and health workers continued to leave Zimbabwe for other countries.
Tapera et al. [30] mentioned that the economic crisis constrained the healthcare delivery system as there was a lack of human resources and limited access to physical resources as some health facilities closed. A lack of treatment and care due to the unavailability of medical drugs and overburdening of patients due to reliance on out-of-pocket funding for treatment services were discussed. It was found that the economic crisis affected the availability of medical equipment needed to provide quality health care.
4. RESULTS
The thematic analysis, conducted according to the steps explained by Tesch (in Creswell [31]), revealed four themes based on the literature reviewed: (1) physical resources (public health infrastructure), (2) human resources (health workers), (3) material resources (medical drugs), and (4) financial resources (public health expenditure and management) that were affected by an economic crisis (Table 1).
4.1. Physical Resources (Public Health Infrastructure)
There was growing evidence that the decline in the economy in most countries affected the physical resources available, resulting in the deterioration of the health facility infrastructure [20, 32]. According to Chimhowu via et al. [1], the Ministry of Health [33] and various media released reports that the economic crisis in Zimbabwe was no exception to this tendency. An economic crisis made it impossible to access health facilities due to the deteriorating physical infrastructure, roads in bad condition [28], rare ambulances functioning, and broken communication equipment [5]. The rural population failed to access health care at the closest health facilities and bore the cost of traveling long distances to other health facilities run by missionaries at the district level and in cities [25].
Long distances between villages and health facilities, especially in resettlement areas as a result of land reform, poor road conditions in rural areas, where potholes were not mended, non-maintenance of bridges that affected the transport system between health facilities and villages [34, 35], ultimately negatively affected the availability of material resources like medical drugs at the rural health facilities.
4.2. Material Resources (Medical Drugs)
An economic crisis affects the supply of medical drugs in public health facilities [22]. In Zimbabwe, the economic crisis affected the capacity of the health sector to purchase medical drugs. The majority of the health facilities in rural areas had limited access to medical drugs [36]. The health care users had to purchase medical drugs from private health facilities and pharmacies at high costs, similar to what was found in Greece [29] and eastern Mediterranean countries [20]. Healthcare facilities were running below 30% of their capability, with chronic shortages of drugs due to the economic crisis [14]. The prohibitive price of medical drugs from private suppliers meant healthcare users had limited access to healthcare for curable ailments that were often fatal [30, 36].
In Zimbabwe, the economic crisis negatively impacted the availability of medical supplies like blood transfusions, sutures, needles, and candles. Patients were asked to buy their own from expensive private pharmacies unavailable in rural areas [36]. For example, pregnant women had to provide their own delivery sets, including suturing materials [36-38], making it difficult for health workers to perform their duties.
4.3. Human Resources (Health Workers)
Human resources, essential in the delivery of quality health care, were most affected by the economic changes, as salaries were changed from united states dollars to bonds and open vacancies froze in 2015 [29], health workers resigned, and the workload increased for those remaining [5, 39]. This worsened the existing challenges of shortage of health workers. In Portugal, Nunes et al. [27] found out that the economic crisis limited the capacity of health workers to develop and deliver high-quality care due to a lack of financial resources.
4.4. Financial Resources (Public Health Expenditure and Management) Affected by an Economic Crisis
The economic crisis affected the financial resources, which impacted not only human resources but overall health expenditures on health care delivery. Evidence in some articles indicated that in 2008, 15 of the 46 countries in the WHO African Region devoted less than 5% of their GDP to health. While five countries were above 9% of their GDP, and total government expenditure on health in the region varied from 11% downwards, with only five countries meeting the Abuja target of allocating at least 15% of the government budget to health [40]. Zimbabwe was and is facing financial challenges as evidenced by the allocation of only 10.1% of the total annual budget to health in 2020, and although it was increased from 7%, allocation in 2019 was still far below both the 13% Sub-Saharan Africa average health care annual expenditure and Abuja declaration target of 15% [41]. Zimbabwe spent an average of US$18.26 health capita in 2019, which was lower than the recommended WHO target of US$34, and the Southern Africa Development Community (SADC) average of US$145.29 [41].
The impact of the economic crisis on accessibility to health care was worse in areas where poor people were selling their livelihoods in order to afford the health care user fees and obtain access to health care, driving them into poverty [14]. User fees’ spending was a challenge to the health care users as it increased disparity to poorer health outcomes [4]. Healthcare services improved from 2009 to 2012 due to funding received from Global Fund. However, the phasing out of the Global Fund supporting the Health Retention Scheme in 2013 left a funding gap of USD 4 million in 2013 and USD 22 million in 2014 [42]. This contributed to the government cutting payment of retention allowances and further losing professional nurses.
5. DISCUSSION
There is growing evidence that the economic crisis alluded to financial constraints that affect governments’ ability to fund public health systems, thus restricting poor people’s access to health care [40]. The healthcare resources affected are physical (health facilities), material (medical drugs and equipment), human (health workers), and financial resources, all “inputs” as indicated in the System Model [43]. These health resources are critical to the effective functioning of the healthcare system [26].
A healthcare system deals with the diagnosis and treatment of ailments, the promotion, protection, and preservation of the health of the people [44, 45], and the offering of essential social services aimed at protecting the health of a country [44]. Health care requires distinct steps that include accessing a health facility (physical resource), finding a health care provider (human resources), accessing medical drugs (material resources), and getting money (financial resources) to access treatment [46].
The economic decline affects these health resources as it is characterised by both cuts in internal funding and cessation of external funding. The reduction contributes to the failure to upgrade and rehabilitate health facilities, thus decreasing the quality of health care in the public health sector [4, 32]. Another vital aspect was infrastructure, where roads were not maintained, limiting access to ambulance services and public transport, hence reducing access to health facilities [47]. Despite putting in place Results Based Financing (RBF) in Zimbabwe for promoting and supporting the rehabilitation of health infrastructure, there was no evidence of infrastructure improvements due to low budg et al. location for capital expenditure and a lack of political will to prioritise health infrastructure [46].
In areas where health facilities exist, access is restricted by shortages of medical drugs as the economic crisis affects the prices, availability, and delivery of medical drug supplies; thus population in both urban and rural areas find it challenging to access health care and obtain prescribed medical drugs [6]. To worsen the situation, the disease burden increased, such as cancer, typhoid, and tuberculosis, as healthcare users failed to get treatment [30, 48].
The economic crisis also contributed to the loss of health workers who resigned due to cuts in remunerations and allowances, further overburdening the few remaining health workers [27]. The cessation in recruitment led to unemployment among professional nurses who opted to emigrate, and as retired professional nurses were not replaced [2], a critical shortage of professional nurses was created. The situation was further worsened by striking health workers. For example, in 2018, there was an increase in the mortality rate at public hospitals from 50% to 70% during 31 days of industrial action strikes by health workers [5].
The shortages affected the availability of essential skills and competencies needed to provide primary healthcare services, such as prevention, early diagnosis, and the control of diseases in rural areas [49]. The health outcomes were affected, in particular, by vital health statistics like the targets of the millennium development goals and sustainable development goals [4]. This mentioned deterioration was also observed and documented in Zimbabwe, where the nurse ratio to 1000 persons fell from 2.5 in 2017 to 1.9 persons in 2019 and a strike by doctors and nurses in 2018 [4].
Statistics that provide evidence of the influence of economic decline in Zimbabwe include a high maternal mortality rate (MMR) of 651 per 100,000 in 2017, a child mortality rate of 900 per 100,000 live births in 2017, and tuberculosis at 782 per 100 000 people [12].
Due to the crippled health sector, the contribution of household and individual expenditure on health increased ranging between 67% in 2007, 87% in 2016, and 90% in 2018, respectively of total private health spending [49]. This was despite the fact that the income levels for the majority of the working group ranged from US$20 to $100, which was far below the monthly family food basket of $500 for a family of five. This led to limited access to health care for those who could afford the fees and exposed the poor to potentially high, unexpected costs and death. These people, mostly in rural areas, turned to traditional healers, failing to get the most needed modern health care, thereby contributing to high mortality rates [30].
CONCLUSION
The economic decline, fueled by politics, had a detrimental effect on health care in Zimbabwe, similar to the evidence provided in the structured review as described. Assuming the fact that the resources for health care are not only an internal affair but also a multi-lateral experience with the global economy, involving international and regional factors, among others, this paper has argued that a unified policy approach is best suited for providing a long-term solution to a declining health care system. More detailed research is needed on how other countries have managed to overcome the effects of economic decline that can be applied to other contexts. In the context of economic recession and austerity, Zimbabwe has to find alternative financing sources to improve the efficiency of the healthcare system [50, 51]. Resuscitating the global fund to assist in the payment of health worker retention allowances could overcome the professional and ethical challenges to funding for health [42]. Funding for healthcare in Zimbabwe needs further investigation to expand, as this structured review revealed funding challenges.
An action plan to address the challenges and improve access to health care in Zimbabwe is crucial if the life, health, and welfare of the population are to be guaranteed and sustained. Zimbabwe needs to be consistent with health worker policies, such as the deployment and bonding policy introduced in 2010 but dropped in 2012. This policy contributed to retention for at least a year for every graduating nursing student and improved the availability of these posts in health facilities [29]. Adherence to economic blueprints like the Transitional Stabilization Program (TSP) and other policies will enhance the achievement of sustainable development goals set by the United Nations in 2015. Thus, reforms in the geopolitical environment, government, and Ministry of Health and Child Care in Zimbabwe are needed. Of concern is the impact of the COVID-19 pandemic globally, which might further negatively impact access to rural health in Zimbabwe [3].
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


