All published articles of this journal are available on ScienceDirect.
Investigating the Reasons for the Unwillingness to Get Vaccinated against COVID-19 in the General Population
Abstract
Aim:
This study sought to identify barriers to COVID-19 vaccination uptake among the general population in Khaf, eastern Iran.
Background:
The sudden emergence of COVID-19 reaffirmed that prevention is preferable to treatment. It is difficult to achieve the goal of widespread COVID-19 vaccination if the general population is reluctant to be vaccinated against it.
Methods:
This study is a cross-sectional analysis of 412 individuals over the age of 18 who were selected via convenience sampling from the general population in 2022. A researcher-made questionnaire was utilized to collect information regarding COVID-19 vaccination hesitancy from the target population over the phone. The questionnaire covered three domains: personal reasons, concerns about the vaccine, and concerns about the Ministry of Health's performance. The collected data were analyzed with SPSS version 22 statistical software using one-sample t-test and multiple linear regression. The level of significance was established at p <0.05.
Results:
This study examined 133 females and 279 males. The highest mean score of COVID-19 vaccination reluctance was associated with the performance of the Ministry of Health (3.77 ± 0.79) and the lowest with personal reasons (2.51 ± 0.57).
Conclusion:
COVID-19 vaccination reluctance was associated more with the performance of the Ministry of Health and the nature of the COVID-19 vaccine. Hence, the Ministry of Health must intervene directly to ensure the success of public vaccination by informing people about the vaccine and alleviating mistrust in society.
1. INTRODUCTION
Since its inception, the global health system has placed prevention ahead of treatment. The sudden emergence of the COVID-19 epidemic strengthened this priority. The burden of diagnosing, treating, and coordinating care for the affected populations is extremely high. Producing effective vaccines to prevent and respond to this situation is essential because of the
severe consequences and costs imposed by this disease on the economies of affected countries [1-3]. Countries with a long history in vaccine production, such as France and the United States, and other countries, mobilized resources to prepare a vaccine for this purpose [4, 5].
Governments have made numerous efforts to control and eradicate this disease, including public education, social distancing policies, screening tests, and vaccine development measures [6]. Vaccination is among the most important global strategies for controlling the COVID-19 pandemic. It is the most effective approach to preventing infectious diseases, particularly in high-risk populations. In addition to preventing disease and lowering mortality rates, vaccination reduces medical expenses and pharmaceutical costs, thereby reducing economic costs [7].
The COVID-19 vaccine has been developed so that COVID-19-specific immunity can be acquired. As a result of previous efforts to develop vaccines against coronavirus diseases such as Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome, we now have a deeper understanding of the structure and function of coronaviruses. Researchers utilized this data to design and develop multiple vaccines that combat COVID-19 more effectively than conventional vaccines [8].
The national immunization campaign in Iran began on February 21, 2019. The first group to receive vaccinations was the medical staff, followed by older adults, individuals with chronic diseases, pregnant women, nursing mothers, and children [9]. Successful immunization programs are those that have broad public acceptance and engagement. As a result, the availability of safe and potent vaccines is not sufficient per se. Vaccines should be broadly embraced by the general population [10, 11]. Even though the success of vaccination depends on public acceptance of the vaccine, studies indicate that public confidence in vaccines is declining [12].
Vaccination hesitancy is defined as delayed acceptance of vaccines, refusal of vaccines, or vaccine acceptance with doubts about its efficacy and safety [13]. Even though the public is aware of the risks and mortality associated with the COVID-19 pandemic, a sizeable proportion of the worldwide population is unwilling to be vaccinated [14]. The World Health Organization ranked vaccination reluctance among the top 10 global health threats for 2019 [15].
Vaccine acceptance is affected by several factors [16], including cognitive, psychological, socio-demographic, and cultural factors [17, 18]. People's health beliefs (e.g., perceived risk and severity of disease, the perceived need for vaccination, and self-efficacy for vaccination) and their assessment of the risks and benefits of vaccination influence their vaccination behavior [19]. Some research findings indicate that vaccination reluctance is influenced by concerns about vaccine efficacy and safety, as well as fake news on social media and the Internet [20, 21]. A lack of trust in vaccines, a negative view of the rapid pace of vaccine development, and unwanted side effects all contribute to a general aversion to getting vaccinated [22]. This is especially true in the context of social media, where anti-vaccine activists have been spreading false and misleading scientific results [23].
Sixty-six percent of Japanese respondents in Yoda and Katsuyama's (2021) study on COVID-19 were eager to get vaccinated, while 22% were unsure, and 12% had no intention of doing so. Eighty-six percent of those who intended to be vaccinated believed the vaccine would protect them from COVID-19, whereas more than sixty percent of those who were unsure expressed doubts. They, especially women, mentioned adverse effects and concerns about vaccine safety [24]. A negative perception of vaccine developers (“They are only motivated by profit”) leads to distrust in vaccines [25, 26]. China and South Korea ranked higher on a global survey of possible acceptance of the COVID-19 vaccine [25]. In recent years, public confidence in the government's capacity to deal with crises and implement coherent policies has declined in many countries [27]. Soares et al. (2021) investigated the variables associated with COVID-19 vaccine skepticism. They found that 56% of people were either behind on receiving the COVID-19 vaccine or refused to undergo vaccinations altogether. Several factors, including young age, loss of income during the epidemic, low confidence in the COVID-19 vaccine, a negative view of the government's actions, and the publication of contradictory information regarding the safety and efficacy of the vaccine, were influential in refusal and delay in vaccination [28].
Paul et al. (2021) explored attitudes toward COVID-19 vaccination in Italy. Only 14% of respondents planned to get vaccinated against COVID-19, and 16% expressed serious doubts about the vaccines. According to the findings of this study, public distrust in vaccines and worries about future side effects are significant barriers to attaining population immunity against COVID-19 through vaccination [29].
There has been a rise in mistrust of the government and its perceived values as a result of factors such as the prevalence of the Internet and social media, the prevalence of anti-vaccine beliefs, low trust in health institutions [21], unpleasant decisions made by government officials without adequate justification [30], and the performance of the health care system. Each element of (dis)trust can affect others [31]. People who are mistrustful of the government, for example, may also distrust vaccines produced by pharmaceutical companies and question their motivation (i.e., profit) [26,32].
Inadequate vaccination coverage and the emergence of mutant virus strains are two of the most important factors that can reduce the effectiveness of the COVID-19 vaccine in a population [17, 18]. Population vaccination may be insufficient if community members are unwilling to inject the vaccine. COVID-19 vaccination hesitancy can be caused by a variety of factors, which ultimately result in a lack of disease control and an increased burden on the healthcare system.
The public's reluctance to get immunized against COVID-19 hampers efforts to achieve public health ends. Vaccination against COVID-19 is one of the most fundamental approaches to preventing COVID-19 infection and reducing mortality. Therefore, understanding the reasons for the general population's reluctance to receive the COVID-19 vaccination can be one of the most effective means of achieving the goals of mass vaccination. Since no previous research has looked into the reasons why the general population of Khaf is unwilling to get vaccinated against COVID-19, this study was created and carried out as an innovation to address this knowledge gap.
2. MATERIALS AND METHODS
This study employed the survey method, which permits the extrapolation of the results to the entire population of interest. This study is cross-sectional because it was conducted during a specific period of time (the second quarter of 2022). The statistical population comprised residents of the city of Khaf aged 18 years and older. According to the 2015 general population census, the total population of Khaf is 33,189. Cochran's formula and a 5% significance level were used to determine the sample size for this study. Attrition of nearly 10% brought the total sample to 412. The main formula for calculating Cochran's sample size is as follows:
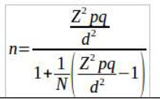 |
n: the size of the statistical sample
N: the size of the statistical population
d: permissible error (considered equal to 0.05)
Z: the value of the normal variable with confidence level α-1. the z value for the 95% confidence level is 1.96
p: Proportion of possessing the desired attribute
q=(p-1): the ratio of not having the desired attribute. p and q are considered 0.5.
After the research ethics committee approved the research protocol, the researcher was given a formal introduction letter from Mashhad University of Medical Sciences to present to the appropriate officials in Khaf's health network.
Participants were recruited using the convenience sampling method. The two comprehensive health services centers in Khaf (Center 1 and Center 2) were chosen as research sites. Reviewing information on the Sinai System (Integrated Information System) at these health centers helped identify unvaccinated individuals. Eligible persons were randomly selected from half of the research population at each center and contacted via phone. Approximately 20 minutes were required to complete the questionnaires over the phone. Thus, participants who met the inclusion criteria were contacted via telephone and asked to complete the questionnaires.
To be eligible for the study, participants had to provide informed consent, not have received the COVID-19 vaccine, be in good mental and emotional health, and be self-reliant and able to make their own decisions. People with organ transplants, advanced cancer, tuberculosis, COVID-19, those taking immunosuppressant drugs, and those who did not fill out the entire questionnaire were excluded.
Data were collected using a researcher-made questionnaire, which included two sections. The first section asked about demographic characteristics (age, gender, occupation, education level, marital status, history of COVID-19 infection with a positive PCR test, history of chronic disease in the respondent or family members, history of infection or death due to COVID-19 among family or friends). The second section asked about reasons for refusal to receive COVID-19 vaccination. There were 18 statements in the questionnaire, broken down into three domains: personal reasons for not desiring to have the COVID-19 vaccine injected (statements 1-8), concerns related to the nature of the COVID-19 vaccine (statements 9-12), and reasons pertaining to the performance of the Ministry of Health with regard to COVID-19 vaccination (statements 13-18). The statements were scored on a 5-point Likert scale ranging from very low (score 1) to very high (score 5). The score for each domain was calculated by summing the statements on that domain and dividing by the number of those statements. The total score of the questionnaire was calculated by dividing the total number of statements by 18. Therefore, the overall score of the questionnaire, as well as the score of each domain, would range from 1 to 5, with a score of 3 representing the mean.
This questionnaire had 8 items regarding personal reasons for not desiring to inject the COVID-19 vaccine: (1) knowledge of the side effects of vaccine injection in others and avoiding potential risks; (2) neglect of referral to vaccination centers; (3) the presence of an underlying disease or a physician's recommendation that prohibited vaccination; (4) limited time to refer for vaccination; (5) non-availability of the preferred vaccine in the country and waiting for a better vaccine; (6) a lack of confidence in the efficacy of the COVID-19 vaccine; (7) the belief that receiving the COVID-19 vaccine would make the person a carrier or infected with COVID-19; and (8) feeling no need to receive the COVID-19 vaccine due to full compliance with health protocols.
There were four concerns associated with the nature of the COVID-19 vaccine listed on this questionnaire: (1) a lack of faith in the vaccines currently on the market; (2) conflicting reports about the vaccine's efficacy and the absence of a scientific metric for its success; (3) a lack of familiarity with the vaccine's composition; and (4) extreme apprehension about the outcomes of the vaccine.
Six statements asked about the reasons related to the performance of the Ministry of Health regarding the COVID-19 vaccine: (1) dissemination of anti-vaccine information in cyberspace and even national media; (2) inadequate training and information provided by health system personnel; (3) non-mandatory COVID-19 vaccine injection; (4) the inability of health system authorities to adequately respond to the statements of anti-COVID-19 vaccination groups; (5) the absence of social restrictions for those who refuse to receive the vaccine; and (6) free and readily available COVID-19 vaccine.
Six experts examined and validated the questionnaire developed by the researchers. Cronbach's alpha test was also used to evaluate the questionnaire's reliability, yielding an alpha coefficient of 0.83; hence, adequate reliability.
The present study complied with ethical standards in two ways: first, all participants gave informed consent to participate; and second, participants were assured that their information would be treated confidentially and that only abstract results would be shared publicly.
Table 1.
| Variable | Frequency | Percent | |
|---|---|---|---|
| Gender | Female | 133 | 32.3 |
| Male | 279 | 67.7 | |
| Marital status | Single | 280 | 68 |
| Married | 132 | 32 | |
| Age (year) | < 30 | 73 | 17.7 |
| 31-35 | 133 | 32.3 | |
| 36-40 | 74 | 18 | |
| > 40 | 132 | 32 | |
| Education level | Illiterate | 78 | 18.9 |
| Non-tertiary | 249 | 60.4 | |
| Tertiary | 85 | 20.6 | |
| Occupation | Homemaker or student | 203 | 49.3 |
| Non-healthcare personnel | 91 | 22.1 | |
| Healthcare personnel | 41 | 10 | |
| Others | 77 | 18.7 | |
| History of COVID-19 infliction | No | 207 | 50.2 |
| Yes | 205 | 49.8 | |
| History of COVID-19 in family | No | 74 | 18 |
| Yes | 338 | 82 | |
| History of chronic disease | No | 260 | 63.1 |
| Yes | 152 | 36.9 | |
| History of chronic disease in the family | No | 168 | 40.8 |
| Yes | 244 | 59.2 | |
| History of COVID-19-related death in family or friends | No | 338 | 82 |
| Yes | 74 | 18 | |
| Variable | Mean | Standard Deviation | Skewness | Kurtosis | Independent Sample t-test | |
|---|---|---|---|---|---|---|
| T Parameter | P-value | |||||
| Personal reason | 2.51 | 0.57 | 1.71 | 1.21 | 17.33 | <0.001 |
| Concerns about the vaccine's nature | 3.69 | 0.98 | 0.34 | -1.77 | 14.17 | <0.001 |
| Reasons associated with the performance of the Ministry of Health | 3.77 | 0.79 | -0.04 | -1.02 | 19.85 | <0.001 |
| COVID-19 vaccination reluctancy in total | 3.19 | 0.67 | -0.34 | -0.79 | 5.79 | <0.001 |
The data were analyzed with SPSS version 22 statistical software using a one-sample t-test (to determine COVID-19 vaccination reluctance) and multiple linear regression (for the effect of demographic variables on such reluctance). The significance level was set to p<0.05.
3. RESULTS
This study examined 412 individuals from the city of Khaf, including 133 (32.3%) females and 279 (67.7%) males. The majority were singles (n=280, 68%), those aged 31 to 35 (n=133, 32.3%), those without a college degree (n=249, 60.4%), and homemakers or students (n=203, 49.3%). Two hundred-five individuals (49.8%) had a history of COVID-19, whereas 152 individuals (36.9%) had a history of chronic disease. Among the respondents, 338 individuals (82%) reported a history of COVID-19 infection in family members, 244 (59.2%) reported a history of chronic illness in their family members, and 74 (18%) reported a history of COVID-19-related death in their family or friends (Table 1).
Given that the skewness and kurtosis coefficients for all variables fell within the interval (2, 2), the data were deemed to have a normal distribution. A study was conducted on the performance of the Ministry of Health regarding COVID-19 vaccination (3.77 ± 0.79), with personal reasons accounting for the lowest average (2.51 ± 0.54). The mean COVID-19 vaccination reluctance score was 3.19 ± 0.67, and the one-sample t-test revealed that the mean score of the personal reasons domain was significantly lower than the average score of reluctance. The mean scores for COVID-19 vaccination reluctance in general, concerns related to the nature of the vaccine, and reasons related to the performance of the Ministry of Health were significantly higher than the theoretical mean score (i.e., 3) (Table 2).
| Variable | Non-standard Coefficient | Standard Coefficient | T Value | Significance Level | Correlation Coefficient | Coefficient of Determination | ||
|---|---|---|---|---|---|---|---|---|
| B Value | Standard Error | β Value | ||||||
| Constant | 3.84 | 0.05 | - | 72.44 | <0.001 | - | - | |
| Gender | -43.0 | 0.07 | -0.30 | 6.29 | <0.001 | 0.30 | 0.09 | |
| Marital status | -0.90 | 0.06 | -0.63 | 16.25 | <0.001 | 0.63 | 0.39 | |
| Age (year) | 31-35 | -0.32 | 0.07 | -0.22 | 4.45 | <0.001 | 0.69 | 0.47 |
| 36-40 | -0.64 | 0.08 | -0.36 | 7.82 | <0.001 | |||
| > 40 | -1.22 | 0.07 | -0.85 | 17.03 | <0.001 | |||
| Education level | Non-tertiary | 0.43 | 0.08 | 0.31 | 5.32 | <0.001 | 0.41 | 0.17 |
| Tertiary | -0.24 | 0.10 | -0.14 | 2.45 | 0.02 | |||
| Occupation | Non-health care personnel | -0.69 | 0.07 | -0.43 | 10.11 | <0.001 | 0.60 | 0.36 |
| Healthcare personnel | -1.14 | 0.09 | -0.51 | 12.24 | <0.001 | |||
| Self-employed | -0.65 | 0.07 | -0.38 | 8.99 | <0.001 | |||
| History of COVID-19 infection | -0.36 | 0.06 | -0.26 | 5.54 | <0.001 | 0.26 | 0.07 | |
| History of COVID-19 in family members | -0.44 | 0.08 | -0.25 | 5.19 | <0.001 | 0.25 | 0.06 | |
| History of chronic disease | -0.22 | 0.07 | -0.16 | 3.25 | 0.001 | 0.16 | 0.02 | |
| History of chronic disease in family members | -0.31 | 0.07 | -0.22 | 4.65 | <0.001 | 0.22 | 0.05 | |
| History of COVID-19-related death in family or friends | 0.03 | 0.09 | -0.02 | 0.36 | 0.72 | 0.02 | 0.01 | |
Multiple linear regression was used to examine the impact of demographic variables on COVID-19 vaccination reluctance, and Duming Coding was employed to incorporate qualitative variables into the model. The test results indicated that COVID-19 vaccination reluctance was significantly and negatively associated with gender, marital status, and age. Indeed, the reluctance to get vaccinated against COVID-19 was significantly higher in women than in men and in single people compared to married people; however, the COVID-19 vaccination reluctance score decreased significantly with age in the studied subjects. In addition, the results revealed that the reluctance score for COVID-19 vaccination was significantly higher among those with non-tertiary education than among those with illiteracy and significantly lower among those with tertiary education than among those with illiteracy. Homemakers and students were significantly less willing to receive the COVID-19 vaccine than other respondents (p <0.001) (Table 3).
According to the results, people with a history of COVID-19 or chronic disease were significantly less reluctant to vaccinate against COVID-19 than those without a history. Similarly, it was significantly lower among individuals with a family history of COVID-19 or chronic disease than those without it (p <0.001). However, there was no significant correlation between the history of COVID-19-related deaths in the family or friends and the score of COVID-19 vaccination reluctance (p = 0.72) (Table 3).
4. DISCUSSION
Vaccination and immunization against diseases are among the greatest achievements of public health. Vaccination programs have decreased the death rate and spread of infectious diseases worldwide [33]. National vaccination programs must be bolstered in order to reduce vaccine-preventable diseases. The high vaccination rate of 70% provides indirect protection for unvaccinated individuals and direct protection for those vaccinated [34]. As there is no specific treatment for the COVID-19 pandemic, the entire globe continues to be under intense pressure [35]. Due to the global spread of COVID-19, mass vaccination is regarded as one of the most effective methods for combating the pandemic. Nevertheless, despite the safety and efficacy of immunization measures, reluctance to vaccinate against COVID-19 has emerged as one of the top 10 threats to global health in 2019, according to the World Health Organization [16, 20].
This study was conducted to determine the reasons behind the reluctance of the general population to be vaccinated against COVID-19. Previous studies have examined knowledge and attitudes regarding the COVID-19 vaccine, whereas the present study examined the reasons for the general population's reluctance to receive the vaccine. Results indicated that the greatest reluctance to receive COVID-19 vaccination was related to the Ministry of Health's performance (3.77 ± 0.79) and the composition of the COVID-19 vaccine (3.69 ± 0.98). The lowest mean score for COVID-19 vaccination reluctance was attributable to personal reasons (2.51 ± 0.57). Understanding people's knowledge, attitudes, practices, and concerns about the COVID-19 vaccine is crucial to increasing its uptake, which is influenced by several factors. This phenomenon has a multifaceted nature. For this reason, it is crucial to comprehend cognitive, psychological, socio-demographic, and cultural factors in order to comprehend the reasons behind it.
According to current findings, the performance of the Ministry of Health and the composition of the COVID-19 vaccine play the most significant roles in the reluctance to receive the COVID-19 vaccination. Concerns about COVID-19 vaccines among the general public have been attributed to a number of factors, including the novelty and lack of information surrounding the vaccine, the perceived risks of vaccines in comparison to the risks caused by the pandemic, and the lack of a safe and approved vaccine on a global scale. Since the beginning of the outbreak, there have been numerous contradictions concerning masks, various drugs, and vaccines, among others. In addition, no credible scientific sources are demonstrating the efficacy of COVID-19 vaccines and no credible sources confirming 100 percent acceptance and vaccination by medical personnel.
Our findings are consistent with those of Verger et al. [36], Kotter et al. [37], and Al Amr et al. [38], who report that people's skepticism about the COVID-19 vaccine stems in part from the healthcare system and the vaccine's experimental nature. Personal concerns were found to play a minor role in explaining why people were reluctant to get the COVID-19 vaccine in the current study. This research finding cannot be compared to other studies due to the absence of a comparative study. Indeed, research suggests that demographic characteristics such as age, gender, occupation, level of education, marital status, access to free vaccinations, race, health insurance, income, number of children, trust in doctors and the Ministry of Health, confidence in the efficacy of the vaccine, fear of vaccine side effects, acceptance or rejection of false beliefs, and past experience with the COVID-19 virus all play a role in whether or not people choose to get vaccinated.
The present study revealed that the mean score of COVID-19 vaccination reluctance was significantly higher for women than for men and for unmarried individuals than for married individuals. In some countries, men work outside the home more than women, which can be mentioned to explain this research finding. Because of their working conditions, men tend to congregate more frequently, which increases their risk of contracting SARS-CoV-2. Therefore, men are more likely than women to desire vaccination against COVID-19. By this finding, Kashmiri et al.'s study on adults over the age of 18 in the city of Bushehr revealed that men were more receptive to the COVID-19 vaccination [39]. Elimat-El's study in Jordan revealed that men were 2.5% more likely than women to receive the COVID-19 vaccine [40]. In a study conducted in the United Kingdom, Freeman et al. found a correlation between gender and vaccine reluctance [26]. In India's urban and rural communities, Danabal's research revealed that women are highly mistrustful of vaccines [41]. In addition, according to two 2020 studies conducted by Galbage et al. and Askarian et al., COVID-19 and death occurred more frequently in men than in women, which may explain why men are more likely to be vaccinated [42, 43].
In the current study, singles were significantly more hesitant to receive the COVID-19 vaccine than married individuals. Married individuals feel more connected to their families and are more willing to receive the COVID-19 vaccine. Alongside this, the studies conducted by Khubchandani et al. [44] and Bartovic et al. [45] corroborate the present study's findings.
The results of the current study indicated that the mean scores of COVID-19 vaccination reluctance in general and its domains vary significantly by age, education level, and occupation among the studied subjects. The mean score of reluctance significantly decreased as the age of the subjects increased. The mean score of COVID-19 vaccination reluctance was significantly higher among individuals with non-tertiary education than among illiterate and tertiary-educated individuals, as well as among homemakers and students compared to other individuals. The results of this study highlight the importance of education as a means of acquiring knowledge.
There is a role for it about health, as it can influence a person's decision to get vaccinated or not. Likewise influential is how people's jobs expose them to COVID-19. The likelihood of contracting the SARS-CoV-2 virus increases with age, and older adults often tend to have a greater sense of responsibility for themselves and others. Since they are more susceptible to contracting the SARS-CoV-2 virus and undergoing its symptoms, they are more likely to get vaccinated against it. The results of this study are comparable to those of Ansari Moghadam et al. [46] and Walid et al. [47].
The mean score of reluctancy was greater among those without a history of coronavirus or chronic disease, as well as those with a history of coronavirus or chronic disease in their family. Those who did not report this history had significantly higher reluctance rates than those who did. Findings from this study suggest that social media has contributed to a heightened awareness of the disease among older adults and those with underlying (chronic) conditions. This population has been prioritized for vaccine administration. As a result, people with chronic diseases and those whose family members suffer from chronic diseases have been more receptive to the vaccine.
People are also more aware of COVID-19 and its risks if they or a family member have previously contracted SARS-CoV-2. Indeed, people tend to seek information in stressful situations because of their anxiety. This reduces their stress because they are aware of it and attempt to understand how to cope. Therefore, people who have already been infected with COVID-19 or who have a history of COVID-19 in their families are more likely to get vaccinated against COVID-19 after receiving more detailed information and understanding of the risks involved.
Similar results were found in the study by Rahimi et al. [48]. Their research revealed that people's knowledge and attitude toward the disease change significantly after a close family member is infected with or dies from COVID-19. Those who have lost a family member due to COVID-19 are more familiar with the disease than those who have not. Individuals infected with COVID-19 or who have lost a family member due to COVID-19 have a more positive attitude toward receiving the COVID-19 vaccine after learning more about it.
Numerous studies corroborate the present study's findings, revealing that a desire to get vaccinated is directly correlated with a positive COVID-19 history [37], contact with patients with COVID-19, and a desire to protect others by getting vaccinated [49, 50].
CONCLUSION
Understanding what influences people's willingness to get vaccinated is crucial to stop the spread of the COVID-19 pandemic. The highest mean score of COVID-19 vaccination reluctance in this study was attributable to the performance of the Ministry of Health and the nature of the vaccine. There are a set of measures that can be taken to improve vaccination acceptance among the general population, including improving public trust in society by involving the Ministry of Health, elucidating policies and laws, providing mass education, particularly by health workers, encouraging people to get vaccinated, and adequately communicating the safety and effectiveness of vaccination to control the COVID-19 pandemic.
LIMITATIONS OF THE STUDY
The disease prevalence justifies the use of a telephone survey as the primary data collection method in this study, which is the primary limitation. It is suggested that future studies be conducted over a longer period and with a larger sample size.
AUTHORS' CONTRIBUTIONS
S.T. and K.H. participated in the conceptualization, design, literature search, data collection, and manuscript drafting. M.Z. and S.S. contributed to statistical analysis and manuscript drafting. R.R. reviewed the manuscript and performed the interviews. The final manuscript was read and approved by all authors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The current study complied with ethical standards in two ways: first, all participants voluntarily agreed to take part in the study; second, participants were assured that their information would be kept private and that only abstract results would be shared with the public. The Biomedical Research Ethics Committee of Mashhad University of Medical Sciences approved this study and issued the study's code of ethics (IR.MUMS.REC.1400.371).
HUMAN AND ANIMAL RIGHTS
No animals were used for the studies that are the basis of this research. All human procedures were per the guidelines of the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
To comply with the ethical considerations in this research, the information of the participants was kept confidential, and other people could not access this information. The names and surnames of the participants were not used for data collection, and data collection was performed after obtaining the code of ethics from Mashhad University of Medical Sciences.
STANDARDS OF REPORTING
COREQ guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting this study's findings are available from the corresponding author [R.R] upon reasonable request.
FUNDING
This article has been performed with the financial support of the Vice-chancellory for Research and Technology of Mashhad University of Medical Sciences (Funder Id /Grant No. 4001509).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This article reports the results of a research project approved by Mashhad University of Medical Sciences. We wish to express our sincere gratitude to the honorable Vice-chancellory for Research and Technology of Mashhad University of Medical Sciences, the honorable officials of the health network of Khaf, the participants, and all those who helped us in conducting this research.


