All published articles of this journal are available on ScienceDirect.
Content Validation of Lumbopelvic Pain Risk Factors Questionnaire among Women: A Modified Delphi Consensus Study
Abstract
Background:
Lumbopelvic pain (LPP) is a surging problem among women worldwide. The genesis of LPP among women is complex as it constitutes a wide array of gynecological, hormonal, gastrointestinal, and obstetrical factors.
Objective:
The objective was to develop and evaluate the content validity of a questionnaire designed to assess general LPP risk factors relevant to women.
Methods:
The questionnaire was drafted by comprehensively drawing items from the literature. The drafted questionnaire was conceptualized using the modified Delphi method and sent to nine experts for professional opinions. Based on the expert evaluation, the draft questionnaire was modified/revised and again sent for expert responses.
Results:
Overall, three rounds of Delphi were administered to reach a consensus between experts finally. The content validity ratio (CVR) and content validity index (CVI) of the questionnaire was calculated. The newly developed questionnaire constituted 19 items identifying LPP risks in women. The CVI of the overall questionnaire (S-CVI) was 0.99. The questionnaire also reached a universal agreement (S-CVI/UA) of 0.89. In terms of reliability, the internal consistency of the questionnaire was good (Cronbach's alpha of 0.8), with excellent test-retest reliability (intra-class correlation coefficient=0.99). The developed questionnaire has 3 domains: ergonomics, general health & well-being, and gynecology & obstetrics.
Conclusion:
Using the findings of this Delphi study, we contend that the 19 items enlisted in the ‘LPP risk factor questionnaire’ depicts a multiplicity of LPP risk factors in women. This questionnaire would be beneficial for clinicians during the prevention and assessment phase of lumbopelvic pain.
1. INTRODUCTION
For over a decade, the World health organization has been promoting lumbopelvic pain (LPP) prevention programs [1, 2]. The exponential rise in LPP cases has become a major source of disability which has caused a significant expenditure loss of US$ 460 million reported in the period between 2010-2016 [3]. A point prevalence of 11.9% ± 2.0%, particularly among women (7.7% of total years lived with disability) has been reported (global burden of disease survey 2019) [1, 2, 4, 5]. LPP is majorly associated with parturition; hence, researchers focus on pregnancy-associated LPP, inadvertently ignoring women in the non-clinical population [4, 5]. Recently, a high prevalence of LPP has been observed among non-pregnant women (46.7%), which has consequentially impacted their quality of life [6]. Any impairment in the anatomical structures in the lumbopelvic region could develop into LPP. The source of the pain can be restricted to either the lumbar spine and pelvis or it could be a combination of lumbar and pelvic pathology [6, 7]. Some occupations that require repetitive bending and rotation of the spine impose cumulative load on the lumbopelvic structures and eventually develop into LPP [8]. Now, ergonomic hazards are not only attributes of occupational demands but are also evident in the routine habits of everyday life of women. Domestic chores practices in India majorly require squatting, and awkward bending postures; predisposing the spine to injuries [9]. A common example of poor ergonomic practice developing or worsening the LPP among women is wearing high-heeled footwear in their daily routines [10]. Whether it's due to unawareness or personal choice, high-heeled footwear has been significantly observed among women, especially those with LPP [11].
LPP could be a result of a single causative factor like an injury or a spectrum of other risk factors (indirectly related to LPP) that may influence the intensity, prognosis, and duration of pain in women [12]. For instance, the pelvic joint structures undergo a substantial amount of changes to accommodate the needs of childbirth [13, 14]. But sometimes, such physiological changes in pelvic structures develop into LPP and can persist with worsening symptoms even after 11 years [15]. The mechanical support of the respiratory and pelvic continence musculature too gets disrupted during such events of abnormal loading on the pelvic joints [13, 16]. Surprisingly, chronic coughing and sneezing have the potential to disturb the optimal load transfer across the lumbopelvic joints [17]. Hence, LPP is not limited to anatomical origin but is entwined with an array of health conditions [18]. Still, scant literature has explored LPP risks beyond their musculoskeletal features [19]. Focusing on only a single aspect of LPP risks i.e., the anatomical origin of the pain, is likely to miss crucial determinants of LPP in women [4, 15, 18]. For instance, the prevalence of LPP has been postulated to be higher among women experiencing psychological distress [20]. LPP and psychological stress are inextricably linked where women with symptoms of frequent psychological distress invariably experience a high perception of LPP [12, 21].
Preventive measures are suggested to be more rational in treating the rising LPP condition. To gain insights into the factors that favor LPP, one needs to study communities and groups other than individual patients [22]. The researchers in this study had previously interviewed women living in the Indian community. Through this qualitative study, they gained insights into the behaviors of Indian women, which are considered potential LPP risk factors. However, that study focused on exploring LPP care-seeking behaviors and not identifying LPP risk factors among the participating women [11]. Hence, the purpose of this study was to identify general risk factors of LPP relevant to women. LPP is well recognized as a complex interplay of gynecological, obstetrics, psychological, and genitourinary factors [4, 23]. Keeping this in mind, the authors opted for a Delphi technique and engaged experts from various healthcare fields to identify LPP risk factors in women. The objective of the study was to obtain a consensus among multidisciplinary experts for identifying LPP risk factors in the context of women to guide the LPP risk assessment.
2. METHODS
Prior institutional ethical approval was obtained for this study (AUUP/IEC/2021-JAN/02). The study was registered in the Clinical trial registry India (CTRI/2021/06/034233).
2.1. Study Design
A modified Delphi method was adopted for this study to evaluate the content validity of the items of the developing questionnaire [24]. The iterative process involved in the Delphi method converts the experts’ responses into group consensus while maintaining the anonymity of the experts throughout the process [24]. Anonymity allows the free expression of responses without any confrontation from other experts [25].
2.2. Procedure
The study was conducted in three stages: 1) Identification of LPP risk factors, 2) Expert opinion, and 3) Estimation of content validity.
2.2.1. Stage 1: Identifying LPP Risk Factors
The purpose was to draft the LPP risk factors in the form of a questionnaire relevant to women in the general (non-clinical) population. The questionnaire development took place in 3 steps: a) domain identification, b) item generation, and c) instrument formation. Literature on lumbopelvic pain was reviewed. The keywords used in the search process were ‘low back pain’, ‘lumbopelvic pain’, ‘pelvic girdle pain’, ‘chronic pelvic pain’, ‘pelvic pain’, ‘risk factors associated’, and ‘Indian women’. A Boolean search combined keywords with the modifier ‘AND’. The following databases were searched: PubMed, Science Direct, Web of Science, Cochrane Library, and Google Scholar. An updated literature search was done in July 2022. Our search focused on LPP risk factors rather than characteristics of LPP. Studies that used self-administered questionnaires and specific measures to assess the risk factors of LPP were also included [25-27].
The advantage of the literature review was that it provided a theoretical basis for preparing the construct of the questionnaire. The standardized guidelines were followed for questionnaire development [28]. The preliminary version of the ‘LPP risk factors questionnaire’ constituted 20 questions and 3 domains of ergonomics, general health & well-being, and gynecology & obstetrics. The questions were drafted in such a manner that focussed on general LPP risk factors and not on any specific (clinical) cause of LPP. The responses to the questionnaire items were dichotomous (Yes/No).
2.2.2. Stage 2: Expert Opinion
The Delphi rounds took place between September-November 2022. Considering the context of low and middle-economic countries, we purposively recruited experts from India. Nine experts from the field of occupational therapy, physiotherapy, medicine, gynecology, psychology, and community rehabilitation were invited to review the draft questionnaire. The selection criteria of experts [26, 27] were: a) Expertise in the field of lumbopelvic pain, ergonomics, gynecology, medicine, physiotherapy, community health, and health psychology, b) at least 10 years of clinical experience in the respective field, c) involved in clinical/academia/research field.
A formal invitation was given to the experts requesting them to participate. Experts who agreed provided their written informed consent. A cover letter that included an information sheet describing the objective of the questionnaire, the drafted questionnaire, and the response sheet for obtaining the ratings was provided to all the experts. Frequent discussions were undertaken by the researchers to improve the construct of the questions.
2.2.3. Stage 4: Estimation of Content Validity
In this study, we estimated the content validity-related estimates. One approach in content validity assessment is the content validity ratio (CVR), individual item statistics [29]. Once the items were selected for inclusion in the questionnaire, the content validity index (CVI) was evaluated for the entire questionnaire as well as for each item [30]. The experts were asked to evaluate the essentiality (3-point Likert ratings) and clarity (4-point Likert ratings) for each item of the draft questionnaire [31]. The validated ‘LPP risk factors questionnaire’ consisted of 19 questions.
2.3. Pre-testing
The purpose of this step was to check for any difficulties in administrating the questionnaire on the target population. The researchers pretested the language and sequence of items of the questionnaire [28]. Fifteen women were asked to respond to the items of the questionnaire on a dichotomous scale (Clear or Unclear) [28, 32, 33]. None of the participating women expressed any difficulty in understating the items of the questionnaire.
2.4. Estimation of Reliability
The reliability of the newly developed LPP risk factors questionnaire was estimated through the internal consistency measure (Cronbach's alpha) [34] and test-retest reliability (intra-class correlation coefficient). Since this questionnaire targets women in the general population. Reliability measures were evaluated in a sample of 190 women aged above 18 years (target population) [35]. The sample of 190 was estimated, taking reference of 10 participants per item of the 19-item LPP risk factors questionnaire [35, 36]. Test-retest reliability of the questionnaire was evaluated on the same sample at an interval of 14 days [35]. Camps were organized in different regions of Delhi according to the convenience of the researcher. Women from all socioeconomic backgrounds were recruited, which included working women as well as homemakers. Furthermore, women with or without LPP, as well as women who had never experienced LPP, were invited to participate. Pregnant, postpartum (up to 6 months) [37], and also women who had recent injury or surgery in the lumbopelvic region were excluded. Written informed consent was also obtained from all participating women. Statistically, the p-value of <0.05 was considered significant.
3. RESULTS
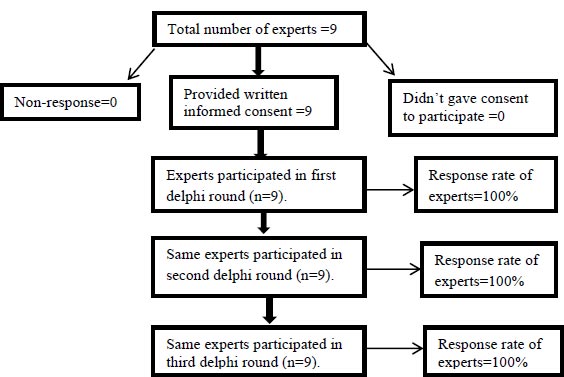
The final expert panel included a gynecologist (n=1), ergonomist expert (n=1), general physician (n=1), physiotherapist (geriatrics & orthopedics) (n=2), occupational therapist (neurology) (n=1), psychology professional (n=1), community health professional (n=1), & pelvic rehabilitation specialist (n=1). Nine experts from various fields of healthcare completed 3 Delphi rounds for this study (Fig. 1).
| Items | Number of Agreements | I-CVI* |
|---|---|---|
| A. Physical activity: | - | - |
| 1. Do you exercise on a daily basis (Excluding walking for work and traveling)? | 5 | 0.55 |
| 2. Does your everyday activities require mostly standing? | 8 | 0.88 |
| 3. Does your everyday activities require mostly sitting? | 9 | 0.99 |
| B. Ergonomics: | - | - |
| 4. Does your everyday activities require bending/ lifting weights? | 9 | 0.99 |
| 5. Do you walk in heels (any type of heels) on a daily basis? | 6 | 0.67 |
| 6. Do you sleep on the floor/ hard mattress/ very soft mattress? | 6 | 0.67 |
| C. General health & well-being: | - | - |
| 7. Do you often suffer from cough/ sneezing/ breathlessness? | 9 | 0.99 |
| 8. Do you often suffer from constipation? | 9 | 0.99 |
| 9. Have you ever previously experienced lower back/ groin/buttocks pain (not menstrual pain)? | 9 | 0.99 |
| 10. Have you experienced uncontrolled dribbling of urine during coughing/ sneezing/ laughing /lifting weights? | 9 | 0.99 |
| 11. In the past month, have you frequently felt depressed/hopeless? | 6 | 0.67 |
| 12. Do you have any kidney problems, diabetes, high blood pressure, or thyroid issues? | 9 | 0.99 |
| 13. Do you have any low bone health issues (Eg. osteoporosis)? | 8 | 0.88 |
| 14. Did you ever have any injury or major surgery in the spine/abdomen/leg? | 9 | 0.99 |
| D. Gynaecology and obstetrics: | - | - |
| 15. Do you have irregular menses/heavy menses/ painful menses? | 9 | 0.99 |
| 16. Have you attained menopause? | 9 | 0.99 |
| 17. Do you have a feeling of heaviness and something coming out of your vagina? | 9 | 0.99 |
| 18. Do you have abnormal vaginal discharge? | 9 | 0.99 |
| 19. Have you ever given birth? | 6 | 0.67 |
3.1. Content Validity-quantitative Analysis (Delphi Round 1)
3.1.1. CVR and I-CVI
In the first round of Delphi, a total of 19 items(questions) were rated for essentiality and clarity for the 9 experts. Except for one, all other items on the scale showed acceptable scores for essentiality and clarity. The experts found Item 1 as ‘not essential’ with CVR =0.55 (less than acceptable CVR critical of 0.78) [29]. Overall, 14 items of the scale showed acceptable I-CVI (0.8 to 1) [36] for clarity. Four items (items 5-6,11, and 19) required revision/modification following (I-CVI=0.67) round 1 (Table 1).
3.1.2. Content Validity of the Overall Questionnaire
The S-CVI/Ave (average proportion) (sum of all I-CVI/total number of items) was 0.90. The universal agreement (S-CVI/UA)(number of items rated ≥3 for clarity by all experts/total number of items) [31] of the questionnaire was 0.67.
3.2. Content Validity-quantitative Analysis (Delphi Round 2)
3.3. Content Validity-quantitative Analysis (Delphi Round 3)
3.3.1. CVR and I-CVI
In round 3, two revised items were sent to the experts. All experts rated these two items as ‘essential’ which reached an I-CVI of 1. Overall, 19 items showed acceptable I-CVI.
3.3.2. Content validity of the Overall Questionnaire
The S-CVI/Ave for the final questionnaire was 0.99 for clarity. The universal agreement(S-CVI/UA) of the questionnaire was 0.89 (Table 2).
3.4. Reliability of the LPP Risk Factors Questionnaire
The questionnaire was administered to 190 women to evaluate the reliability of the questionnaire [37]. The mean± standard deviation (SD) age of participants was 36.7±11.45 years. 26.84% of participants were between 18-27 years of age, 27.3% of participants were between 28-38 years of age, 24.21% of the participants were between 39-49 years of age and 14.21% of participants were ≥50 years old. The body mass index (BMI) of the participating women was 25.89±3.6 kilogram/meter2. 67% (n=129) of the participating women had LPP. The pooled responses from the participants yielded a Cronbach's alpha of 0.8 (Table 3). Hence, the inter-item reliability of the 19-items LPP risk factors questionnaire was good [34].
| Items | CVR | I-CVI |
|---|---|---|
| A. Physical activity: | - | - |
| 1. Does your everyday activities require mostly standing? | 0.99 | 0.88 |
| 2. Does your everyday activities require mostly sitting? | 0.99 | 0.99 |
| 3. Does your everyday activities require bending/ lifting weights? | 0.99 | 0.99 |
| B. Ergonomics: | - | - |
| 4. Do you wear heeled footwear (whether narrow or broad base heels) on regular basis? | 0.99 | 0.99 |
| 5. Do you sleep on a hard (firm) mattress/ floor? | 0.78 | 0.99 |
| 6. Do you sleep on a very soft (sponge/foam) mattress? | 0.99 | 0.99 |
| C. General health & well-being: | - | - |
| 7. Do you often suffer from cough/ sneezing/ breathlessness? | 0.99 | 0.99 |
| 8. Do you often suffer from constipation? | 0.99 | 0.99 |
| 9. Have you ever previously experienced lower back/ groin/buttocks pain (not menstrual pain)? | 0.99 | 0.99 |
| 10. Have you experienced uncontrolled dribbling of urine during coughing/ sneezing/ laughing /lifting weights? | 0.99 | 0.99 |
| 11. In the past month, have you frequently felt stressed/ upset/ irritated? | 0.99 | 0.99 |
| 12. Do you have any kidney problems, diabetes, high blood pressure, or thyroid issues? | 0.99 | 0.99 |
| 13. Do you have any low bone health issues (Eg. osteoporosis)? | 0.99 | 0.88 |
| 14. Did you ever have any injury/major surgery in the spine/abdomen/leg? | 0.99 | 0.99 |
| D. Gynaecology and obstetrics: | - | - |
| 15. Do you have irregular menses/heavy menses/ Painful menses? | 0.99 | 0.99 |
| 16. Have you attained menopause? | 0.99 | 0.99 |
| 17. Do you have a feeling of heaviness and something coming out of your vagina? | 0.99 | 0.99 |
| 18. Do you have abnormal vaginal discharge? | 0.78 | 0.99 |
| 19. How many times have you gone through childbirth (either natural or cesarean delivery)? (None Once More than once) | 0.99 | 0.99 |
| S-CVI/Ave* | - | 0.99 |
| S-CVI/UA** | - | 0.89 |
** Universal CVI.
| - | Scale Mean if Item Deleted | Scale Variance if Item Deleted | Corrected Item-Total Correlation | Cronbach's Alpha if Item Deleted |
|---|---|---|---|---|
| 1. Does your everyday activities require mostly standing? | 25.76 | 15.674 | -.028 | .809 |
| 2. Does your everyday activities require mostly sitting? | 25.19 | 13.607 | .547 | .780 |
| 3. Does your everyday activities require bending/ lifting weights? | 25.53 | 14.452 | .281 | .797 |
| 4. Do you wear heeled footwear (whether narrow or broad base heels) on regular basis? | 25.61 | 15.002 | .145 | .805 |
| 5. Do you sleep on a hard (firm) mattress/ floor? | 25.51 | 14.272 | .328 | .794 |
| 6. Do you sleep on a very soft (sponge/foam) mattress? | 25.52 | 14.833 | .172 | .804 |
| 7. Do you often suffer from cough/ sneezing/ breathlessness? | 25.46 | 13.932 | .414 | .789 |
| 8. Do you often suffer from constipation? | 25.53 | 14.949 | .143 | .806 |
| 9. Have you ever previously experienced lower back/ groin/buttocks pain (not menstrual pain)? | 25.07 | 13.038 | .886 | .763 |
| 10. Have you experienced uncontrolled dribbling of urine during coughing/ sneezing/ laughing /lifting weights? | 25.46 | 13.636 | .500 | .783 |
| 11. In the past month, have you frequently felt stressed/ upset / irritated? | 25.15 | 13.019 | .771 | .766 |
| 12. Do you have any kidney problems, diabetes, high blood pressure, or thyroid issues? | 25.18 | 13.132 | .709 | .770 |
| 13. Do you have any low bone health issues (Eg. osteoporosis)? | 25.48 | 13.690 | .489 | .784 |
| 14. Did you ever have any injury/ major surgery in the spine/abdomen/leg? | 25.33 | 13.673 | .483 | .784 |
| 15. Do you have irregular menses/heavy menses/ painful menses? | 25.56 | 15.189 | .082 | .809 |
| 16. Have you attained menopause? | 25.63 | 14.297 | .373 | .791 |
| 17. Do you have a feeling of heaviness and something coming out of your vagina? | 25.86 | 15.568 | .122 | .802 |
| 18. Do you have abnormal vaginal discharge? | 25.69 | 14.869 | .228 | .799 |
| 19. How many times have you gone through childbirth (either natural or cesarean delivery)? (Noneπ Once π More than onceπ) | 25.28 | 13.948 | .413 | .789 |
The questionnaire was administered to the same participants again after fourteen days, and test-retest reliability was estimated (two-way mixed effects model) with a 95% confidence interval (ICC=0.99). The test-retest reliability was evaluated (ICC=0.99).
4. DISCUSSION
This research reports quantity indices for the content validity of the LPP risk factors questionnaire, which was developed with a concern for identifying LPP risk factors among women. After three rounds of Delphi, 19 items were identified as relevant to be included in the questionnaire. The study outcome (LPP risk factors questionnaire) can be utilized as a reference to identify the risks of LPP among women. As this questionnaire was developed for the general population, thus the questionnaire language was kept in lay terms. With the multidisciplinary panel of experts, the Delphi study could achieve consensus on most of the items in this questionnaire.
An excellent agreement was established between the experts in terms of I-CVI scorings after the final Delphi round. I-CVI scores obtained in this study were way higher than the minimum recommended I-CVI score of 0.78 [38]. The content validity of the overall questionnaire was S-CVI/Avg=0.99, representing an excellent average proportion [38]. The universal agreement of the questionnaire (S-CVI/U) was also high as per recommendation [38]. Ambiguity and complexity of words were the main reasons for item modification in this study. As for the reliability estimation, the questionnaire showed good internal consistency with Cronbach’s alpha of 0.8. Noteworthily, an interval of 14 days between test and retest reliability estimation was chosen so that women would not remember their previous responses. Moreover, the 14 days interval is insufficient for any change to occur as that could otherwise influence the responses [35].
The consensus-establishing approach used in this study identified several LPP risk factors that need to be implemented by healthcare professionals. The first domain of the questionnaire identifies risk factors of LPP linked to routine physical activities. Spending most time of the day sitting (I-CVI=0.99) or standing (I-CVI=0.88) too, received a high rating from all experts. Adopting such passive postures in everyday routine has been found to decrease lumbopelvic stability [39]. The second domain of the questionnaire was about the ergonomic risk factors of LPP. A common women-specific ergonomic risk identified in the literature was high-heeled footwear [10]. Despite awareness about the adverse effect of wrong footwear on spine posture, it has been observed that women choose to wear such footwear because of their liking for fashion trends [11]. In this study, wearing high-heeled footwear achieved a rating of 0.99 by all experts. Since the intensity of pain is mild in the general population, there is a tendency to ignore or cope with LPP through self-help strategies [11, 40]. The cost of this ignorance is the recurring, chronic, and sometimes worse symptoms of LPP. Evidence suggests that pain left untreated has poor outcomes in later life [41].
Owing to its link with several health conditions [4], general health & well-being risk factors of LPP were included in the third domain of the questionnaire. The literature consistently illustrates that every aspect of health, whether physical or mental, is worsened with the presence of LPP [12, 42]. Even though there is no direct association between psychological stress and musculoskeletal impairments, women with LPP have reported worsened pain symptoms when under stress [4, 12, 42, 43]. Psychological stress also influences pain coping where pain catastrophizing has been observed more among women [23]. Moreover, the International Association for the Study of Pain describes pain as a sensory and emotional experience [44]. Lumbar spine pathology is frequently observed among women with metabolic changes [19]. The experts in our study agreed (80% consensus) with the inclusion of the general health & well-being domain as an LPP risk factor. The third domain focussed on the gynecological & obstetric risk factors of LPP. LPP related to pregnancy has been widely described in the literature [15]. We explored gynecological factors beyond the commonly studied pregnancy-associated LPP, like menstrual disturbances, abnormal vaginal discharge, and pelvic organ prolapse [4].
5. STRENGTHS OF THE STUDY
This is the first questionnaire developed on LPP; thereby addressing lumbar as well as pelvic pain. Pelvic pain otherwise is usually examined among pregnant women [45]. Moreover, in some cases, lumbar and pelvic pain can occur in combination [6]. Previous literature has majorly focused on pregnancy-related LPP, inadvertently ignoring the women who are not pregnant [45, 46]. This study is, however, distinctive as it targeted women in the general population (non-clinical). The multidisciplinary panel of experts contributed to the drafting of a multifaceted risk factors questionnaire for LPP. To develop a questionnaire with a high content validity, this study used a combination of literature review and modified Delphi method. Through the Delphi method, the experts provided valuable inputs after every round.
6. LIMITATIONS AND FUTURE RESEARCH
This study focused on estimating content validity, which is one measure of validity. Hence, the limitation was that even though a high consensus was achieved among experts, the findings of this Delphi study need to be corroborated by further validation measures in a large sample. The LPP risk factors questionnaire can be translated into other languages and validated in the respective language.
CONCLUSION
LPP has long-term biological, psychological as well as poor ergonomic causes and consequences which are considered significant in its management and prevention [6]. These risk factors were accurately clubbed in the newly developed ‘LPP risk factors questionnaire’ in the current study and achieved excellent agreement among the experts. Thus, this questionnaire has potential utilization in the healthcare practice at the clinical as well as community level.
LIST OF ABBREVIATIONS
| LPP | = Lumbopelvic pain. |
| CVR | = Content validity ratio. |
| CVI | = Content validity index. |
| S-CVI | = Scale content validity index. |
| U-CVI | = Universal content validity index. |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Prior institutional ethical approval was obtained for this study at Amity Institute of Physiotherapy, Amity University UP (AUUP/IEC/2021-JAN/02).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. The Delphi study followed the equator equator guidelines for Conducting and Reporting Delphi Studies (CREDES).
AVAILABILITY OF DATA AND MATERIALS
The study data will be available upon request from the corresponding author [J.K.C].
ACKNOWLEDGEMENTS
Declared none.


