All published articles of this journal are available on ScienceDirect.
Use of Female Sterilization and associated Factors among Women of Reproductive Age in Malawi
Abstract
Background:
Malawi has witnessed an increase in the uptake of female sterilization, making it one of the few countries having a high prevalence of female sterilization on the continent. The factors responsible for the high uptake of female sterilization are not known.
Objective:
The main objective of this study was to establish the factors associated with the use of female sterilization in Malawi.
Methods:
In the study, the 2015-16 Malawi Demographic and Health Survey has been used. The chi-square test and multivariate binary logistic regression were used to explore the factors influencing the uptake of female sterilization in the country.
Results:
Results showed the prevalence of female sterilization to be 18.1% as a method of contraception. Women residing in the Northern Region (OR=1.587, 95% CI=1.276-1.972; p=0.000) and the Central Region (OR=2.387, 95% CI=2.084-2.734; p=0.000), with no education (OR=2.102, 95% CI=1.634-2.703; p=0.000) and primary education (OR=1.488, 95% CI=1.206-1.835; p=0.000), who had not been visited by a field worker in the last twelve months (OR=2.252, 95% CI=1829-2.774; p=0.000) or had not visited a health centre in the last twelve months (OR=1.860, 95% CI=1.634-2.117; p=0.000), had higher odds of being sterilized. While women who were not working (OR=0.771, 95% CI=0.664-0.894; p=0.000), aged 30 years or less (OR=0.104, 95% CI=0.0.79-0.136; p=0.000), poor (OR=0.599, 95% CI=0.510-0.704; p=0.000), having middle wealth status (OR=0.744, 95% CI=0.626-0.883; p=0.000), having no child (OR=0.163, 95% CI=0.119-0.223; p=0.000) or 1-2 children (OR=0.408, 95% CI=0.352-0.473; p=0.000), and not being aware or having heard regarding family planning from television (OR=0.769, 95% CI=0.603-0.981; p=0.000), had lower odds of using female sterilization.
Conclusion:
According to African standards, the use of female sterilization in Malawi is high. The factors associated with the use of female sterilization include a high level of education, residing in the Central or Northern Region, aging 30 years and above, having been visited by a field worker in the past 12 months, having visited a health facility in the past 12 months, having heard regarding family planning on TV in the past few months, work status, wealth, and children ever born. These factors should be considered when planning future contraceptive strategies to improve the uptake of female sterilization. Family planning programs should also aim at economic empowerment for women.
1. INTRODUCTION
Female sterilization is a permanent contraceptive method used by women who do not wish to have more children. Globally, female sterilization is the most common contraceptive method used by women. In 2019, 23.7% of the 219 million women using contraception relied on female sterilization [1].
The advantages of using female sterilization as a method of contraception include safety, effectiveness, and no additional cost or medical check-ups [3]. One of the disadvantages associated with female sterilization is that it does not protect against STIs, which are not easily remedied and, hence, the use of condoms is still advocated. The permanent nature of the method is one of the barriers to its uptake.
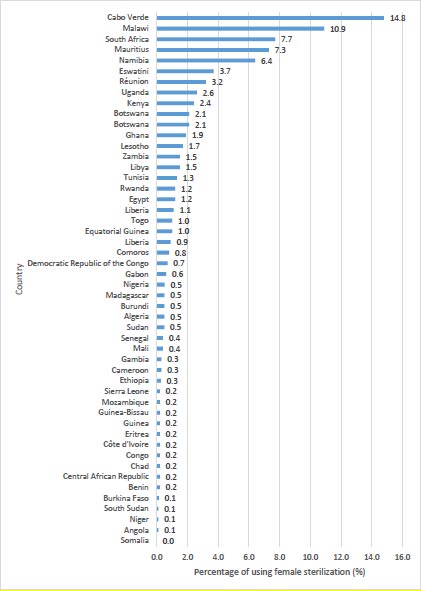
Globally, there exist continental and regional differences in the use of female sterilization [1]. According to United Nations data on contraceptive use compiled in 2019, the use of female sterilization has been reported as highest in Southern Asia1 (28.9%), Eastern Asia (26.6%), Latin America, including the Caribbean (25.9%), Northern America (28.9%), Oceania (13.9%) South-eastern Asia (7.2%), and Western Asia (4.4%), and lowest in Africa (1.6%) and Central Asia (1.4%) [1]. The countries having a high prevalence of female sterilization include India (37.9%), Colombia (35%), and El Salvador (36.8%) [1]. Within Africa, studies have indicated the uptake of female sterilization to be highest in Southern Africa (13%), followed by Eastern Africa (1.9%), Northern Africa (1.4%), and Middle Africa (0.5%), and lowest in Western Africa (0.4%) [1]. No country in Africa has been reported with a prevalence of female sterilization higher than 15%. As highlighted in Fig. (1), Malawi is one of the few countries in Africa that has the highest prevalence of female sterilization [9].
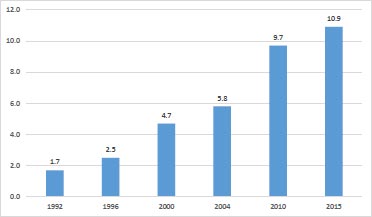
In comparison to other African countries, Malawi has witnessed a tremendous increase in contraceptive use. The contraceptive prevalence rate, as shown in Fig. (2), has increased from 7% in 1992 to 22% in 2004, 46% in 2010, and 59.2% in 2015 [2-6]. An unmet need for family planning has declined from 36.3% in 1992 to 29.7% in 2000, 27.6% in 2004, and 26.1% in 2010, reaching 18.7% in 2015 [2-6]. Furthermore, since the adoption of the national family planning program in the 1990s, the contraceptive mix has changed significantly. The most used methods in 1992 were pills (2.2%) and rhythm method (2.2%), while in 2000, the most used methods were injections (13.9%), followed by female sterilization (4.8%). In 2004, the most used methods were injections (29.7%). Followed by implants (12.3%) and female sterilization (10.9%). In 2010, the most used methods were injectables (25.8%), female sterilization (9,7%), traditional methods (3.8%), pills (2.5%), and male condoms (2.4%). The prevalence of female sterilization has increased from 1.7% in 1992 to 4.7% in 2000, 5.8% in 2004, 9.7% in 2010, and 10.9% in 2015 (Fig. 2).
1 The percentage of contraceptive use is the percentage of women of reproductive age who are currently using the method. This is calculated as the number of women aged 15-49 who are currently using any method divided by the number of women of reproductive age, multiplied by 100.
Studies in Malawi have mostly examined social and economic factors that influence modern contraceptive use in the country [7-12]. These studies have shown that contraceptive use in the country is significantly associated with the women’s level of education, wealth status, religion, age, number of surviving children, and exposure to the media [7, 13, 14]. The use of maternal health services, including skilled delivery care and timing of post-delivery care, has also been shown to influence contraceptive use in Malawi [15, 16]. Other studies have focused on specific segments of the Malawian population, such as young people [8, 17, 18], the male population [19], and individual districts [20]. However, no study has explored the determinants of female sterilization despite this being a popular method of contraception in the country. The aim of this study was to explore the factors associated with the uptake of female sterilization in Malawi.
2. MATERIALS AND METHODS
2.1. Source of Data
This study used data from the 2015–16 Malawi Demographic and Health Survey (MDHS). This was the fifth survey conducted by the National Statistical Office with technical support from ICF International to collect data on demographic and health indicators. The 2015-16 MDHS was a nationally representative cross-sectional survey of women in the reproductive age. The survey used a two-stage cluster sampling procedure. The first stage involved the selection of clusters or enumeration areas, whereas in the second stage, households from each cluster were selected [6]. The 2015–16 MDHS interviewed 24,562 women aged 15-49 years. However, the sample for this study population was 11,287 women who were using any contraceptive method. Women not currently using any of the mentioned methods and all missing cases were removed from the study.
2.2. Variable Selection and Measurements
The dependent variable was the use of female sterilization. This variable was derived from responses to the questions “are you or your partner doing something or using any method to delay or avoid getting pregnant” and “which method are you using?” Women who answered “yes” to the first question were asked the second question. The possible responses to the second question were female sterilization, male sterilization, IUD, injectables, implants, pills, condom, female condom, emergency contraception, standard days method, lactational amenorrhea method, rhythm method, withdrawal, and other modern and traditional methods. The responses were re-coded as follows: women who used female sterilization were coded as 1, while women using other contraceptive methods were coded as 0.
The independent variables used in this study included the age of the respondent, level of education, place of residence, region, wealth status, work status, marital status, type of marriage, number of children ever born (CEB), age at first sex, age at first marriage, age at first birth, media exposure, having heard regarding family planning on the radio in the last few months, having heard about family planning on TV in the last few months, having read regarding family planning in the newspaper/magazine in the last few months, having heard about family planning by text messages on mobile phone, and having been visited by a field worker or having visited a health facility.
The independent variables included in the study were based on prior studies [21-23] and their assumed association with sterilization uptake. Some of the independent variables were regrouped to facilitate easy analysis and interpretation. The variable age of the respondents, classified into five age groups, was regrouped into two groups, with 1 = less than 30 years and 2 = 30 years and older. For the highest level of education attained, two groups, “secondary” and “higher”, were merged. Marital status was regrouped into 3 categories as 0 = never in union, 1 = married, and 2 = formerly married. Wealth status was regrouped by combining poorest and poorer to form a group of poor and richer and richest into rich, and the re-coded groups were 1 = poor, 2 = middle, and 3 = rich. For the number of CEB, the categories were re-grouped as 0, 1-2 CEB, 3-4 CEB, and 5+ CEB. Age at first sex, age at the birth of first child, and age at first marriage were all considered continuous variables and were dichotomised at 18 years, i.e., 18 years and younger and older than 18 years. The independent variables were checked for multi-collinearity before performing multiple logistic regression modelling.
2.3. Data Analysis
A descriptive summary indicating the frequency distribution of women by socio-demographic characteristics was provided. Secondly, Pearson’s chi-square test was used to analyse the association of female sterilization use during the period compared to each explanatory variable. The following logistic regression model was used to establish factors associated with the use of female sterilization in Malawi:
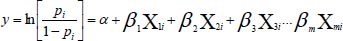 |
Where, pi is the probability of using the female sterilization contraceptive method based on the respondent’s demographic and socioeconomic characteristics, and 1 − p is the probability of not using sterilization. Xi refers to independent variables, a is a constant, and bi represents coefficients associated with the independent variables. Due to the complexity of the sampling design used in DHS, some areas were more likely to be under-sampled or over-sampled. The data were weighted due to the complex nature of the sampling design. Sample weight was applied by dividing the individual women's sample weight by 1,000,000 (v005/106).
2.4. Ethical Consideration
Permission was obtained from Measure DHS to access and use the 2015-16 MDHS dataset for this study. Ethical review and approval for procedures and questionnaires for standard DHS surveys have been provided by the ICF Institutional Review Board and National Health Sciences Research Committee in Malawi [6]. All respondents gave their informed consent for inclusion before they participated in the study [6].
3. RESULTS
3.1. Characteristics of the Study Population
Table 1 shows the percentage distribution of a weighted sample of 11287 women aged 15-49 years with respect to selected background characteristics. The results in Table 1 indicate that the majority (48.5%) of the women were younger than 30 years, while 51.5% were aged 30 years and older. In terms of region of residence, 45.4% resided in the Central Region of Malawi, 43.4% resided in the Southern Region, and 11.2% resided in the Northern Region. Most of the respondents (82.3%) were rural dwellers. Table 1 also indicates that nearly two-thirds (64.4%) of the women had attained a primary level of education, while 22.7% had attained at least a secondary level of education. In terms of wealth status, the majority (42.0%) of the women were from rich households, 38.5% were from poor households, and 19.5% of them belonged to the middle class. The results presented in Table 1 also indicate that the majority (71.1%) of the women were working, while 28.9% were not currently working. With regards to marital status, results show that the majority (84.6%) of the women reported that they were currently married and, of these, 87.9% were in monogamous marriages. Slightly over half of the women (55.1%) had their first sex before the age of 18 years, whereas 66.4% of the women were married before 18 years, and 81.6% of the women had their first born before the age of 18 years. Over one-third (34.4%) of the women had 12 CEB, 31.1% had 3–4 CEB, 31.8% had 5 or more CEB, and 2.8% had no CEB.
| Background Characteristics | Frequency | Percentage (%) |
|---|---|---|
| Age (years) | - | - |
| ≤30 | 5475 | 48.5 |
| >30 | 5812 | 51.5 |
| Total | 11287 | 100.0 |
| Region | - | - |
| Northern region | 1265 | 11.2 |
| Central region | 5123 | 45.4 |
| Southern region | 4899 | 43.4 |
| Total | 11287 | 100.0 |
| Urban | 2001 | 17.7 |
| Rural | 9285 | 82.3 |
| Total | 11286 | 100.0 |
| Education | - | - |
| None | 1452 | 12.9 |
| Primary | 7268 | 64.4 |
| Secondary+ | 2568 | 22.7 |
| Total | 11288 | 100.0 |
| Wealth | - | - |
| Poor | 4346 | 38.5 |
| Middle | 2201 | 19.5 |
| Rich | 4740 | 42.0 |
| Total | 11287 | 100.0 |
| Work status | - | - |
| No | 3259 | 28.9 |
| Yes | 8028 | 71.1 |
| Total | 11287 | 100.0 |
| Marriage | - | - |
| Never married | 499 | 4.4 |
| Currently married | 9552 | 84.6 |
| Formerly married | 1235 | 10.9 |
| Total | 11286 | 100.0 |
| Type of marriage | - | - |
| Monogamy | 8400 | 87.9 |
| Polygamy | 1153 | 12.1 |
| Total | 9553 | 100.0 |
| Age at first sex (years) | - | - |
| <18 | 6042 | 55.1 |
| ≥18 | 4929 | 44.9 |
| Total | 10971 | 100.0 |
| Age at first marriage | - | - |
| <18 (years) | 7161 | 66.4 |
| ≥18 | 3627 | 33.6 |
| Total | 10788 | 100.0 |
| Age at the birth of first child (years) | - | - |
| <18 | 9200 | 81.6 |
| ≥18 | 2074 | 18.4 |
| Total | 11274 | 100.0 |
| Children ever born | - | - |
| 0 | 316 | 2.8 |
| 1–2 | 3880 | 34.4 |
| 3–4 | 3507 | 31.1 |
| 5+ | 3584 | 31.8 |
| Total | 11287 | 100.0 |
| Media | - | - |
| No exposure | 4664 | 41.3 |
| Exposure | 6623 | 58.7 |
| Total | 11287 | 100.0 |
| Heard about family planning on the radio in the last few months | - | - |
| No | 6314 | 55.9 |
| Yes | 4972 | 44.1 |
| Total | 11286 | 100.0 |
| Heard regarding family planning on the TV in the last few months | - | - |
| No | 10133 | 89.8 |
| Yes | 1154 | 10.2 |
| Total | 11287 | 100.0 |
| Read about family planning in the newspaper/magazine in the last few months | - | - |
| No | 10265 | 91.0 |
| Yes | 1021 | 9.0 |
| Total | 11286 | 100.0 |
| Heard about family planning by text messages on mobile phone | - | - |
| No | 10647 | 94.3 |
| Yes | 639 | 5.7 |
| Total | 11286 | 100.0 |
| Visited by a field worker in the last 12 months | - | - |
| No | 9694 | 85.9 |
| Yes | 1593 | 14.1 |
| Total | 11287 | 100.0 |
| Visited a health facility in the last 12 months | - | - |
| No | 9694 | 85.9 |
| Yes | 1593 | 14.1 |
| Total | 11287 | 100.0 |
| Region | Not Sterilized | Sterilized | Chi-square | P-value |
|---|---|---|---|---|
| Northern region | 83,5 | 16,5 | 177.504 | 0.000 |
| Central region | 76,7 | 23,3 | - | - |
| Southern region | 86,9 | 13,1 | - | - |
| Type of residence | - | - | 6.040 | 0.014 |
| Urban | 83,8 | 16,2 | - | - |
| Rural | 81,5 | 18,5 | - | - |
| Heard about family planning on the radio in the last few months | - | - | 0.174 | 0.676 |
| No | 81,8 | 18,2 | - | - |
| Yes | 82,1 | 17,9 | - | - |
| Heard about family planning on the TV in the last few months | - | - | 3.743 | 0.053 |
| No | 81,7 | 18,3 | - | - |
| Yes | 84,0 | 16,0 | - | - |
| Read about family planning in the newspaper/magazine in the last few months | - | - | 16.668 | 0.000 |
| No | 81,4 | 18,6 | - | - |
| Yes | 86,6 | 13,4 | - | - |
| Heard about family planning by text messages on mobile phone | - | - | 7.991 | 0.005 |
| No | 81,6 | 18,4 | - | - |
| Yes | 86,1 | 13,9 | - | - |
| Visited by a field worker in the last 12 months | - | - | 89.135 | 0.000 |
| No | 80,5 | 19,5 | - | - |
| Yes | 90,3 | 9,7 | - | - |
| Visited a health centre in the last 12 months | - | - | 159.962 | 0.000 |
| No | 80,5 | 19,5 | - | - |
| Yes | 90,3 | 9,7 | - | - |
| Marriage | - | - | 113.184 | 0.000 |
| Never in union | 99,0 | 1,0 | - | - |
| Currently in union/living with a man | 81,5 | 18,5 | - | - |
| Formerly in a union/living with a man | 77,8 | 22,2 | - | - |
| Type of marriage | - | - | 36.674 | 0.000 |
| Monogamy | 82,4 | 17,6 | - | - |
| Polygamy | 75,0 | 25,0 | - | - |
| Work status | - | - | 109.926 | 0.000 |
| No | 87,6 | 12,4 | - | - |
| Yes | 79,6 | 20,4 | - | - |
| Age (years) | - | - | 1974.096 | 0.000 |
| ≤30 years | 98,5 | 1,5 | - | - |
| >30 years | 66,3 | 33,7 | - | - |
| Age at first sex (years) | - | - | 2.868 | 0.090 |
| <18 | 81,4 | 18,6 | - | - |
| ≥18 | 81,4 | 18,6 | - | - |
| Age at first marriage (years) | - | - | 2.525 | 0.112 |
| <18 | 80,7 | 19,3 | - | - |
| ≥18 | 81,9 | 18,1 | - | - |
| Age at birth of first child (years) | - | - | 0.005 | 0.944 |
| <18 | 81,6 | 18,4 | - | - |
| ≥18 | 83,2 | 16,8 | - | - |
| Children ever born | - | - | 2053.574 | 0.000 |
| 0 | 99,4 | 0,6 | - | - |
| 1–2 | 97,9 | 2,1 | - | - |
| 3–4 | 86,0 | 14,0 | - | - |
| 5+ | 58,9 | 41,1 | - | - |
| Education | - | - | 374.093 | 0.000 |
| None | 66,4 | 33,6 | - | - |
| Primary | 81,8 | 18,2 | - | - |
| Secondary+ | 90,8 | 9,2 | - | - |
| Wealth | - | - | 37.526 | 0.000 |
| Poor | 84,6 | 15,4 | - | - |
| Middle | 81,2 | 18,8 | - | - |
| Rich | 79,7 | 20,3 | - | - |
| Media | - | - | 1.847 | 0.174 |
| No exposure | 81,3 | 18,7 | - | - |
| Any exposure | 82,3 | 17,7 | - | - |
3.2. Association between Female Sterilization use and Women’s Background Characteristics
Table 2 indicates a relationship between female sterilization and background variables. The variables, age, region, type of residence, education, work status, wealth status, marital status, type of marriage, having read regarding family planning in the newspaper/magazine in the last few months, having heard about family planning by text messages on mobile phone, having been visited by a field worker, and having visited a health facility were significantly associated with the uptake of female sterilization.
The percentage of female sterilization was higher among women aged 30 years and older (33.7%) than among women younger than 30 years (1.5%) (p=0.000). The percentage of women being sterilized ranged from 13.1% in the Southern region to 16.5% in the Northern region and 23.3% in the Central region (p=0.000). With respect to the place of residence, the study results indicated that 18.5% of the women who reported that they resided in rural areas were sterilized compared to 16.2% of their urban counterparts (p=0.014).
Furthermore, the percentage of sterilization was 33.6% for women who had no education, 18.2% for those who had attained primary education, and 9.2% for those who had attained at least a secondary level of education (p=0.000). The percentage of women who reported having been sterilized decreased with an increase in the level of education attained.
In terms of work status, the percentage of sterilization was 20.4% for working women and 12.4% for women who were not working (p=0.002). The percentage of women being sterilized increased with the rising wealth status. 15.4%, 18.8%, and 20.8% of women in poor, middle, and rich classes, respectively, had been sterilized (p=0.000). The results also showed that the prevalence of female sterilization was highest among formerly married women (22.2%), followed by currently married women (18.5%), and it was lowest among those never married (1.0%). The relationship between marital status and female sterilization was significant (p=0.000) at a 5% level of significance. Furthermore, female sterilization was higher among women in polygamous unions (25.0%) than those in monogamous marriages (17.6%) (p=0.000).
Pertaining to the number of CEB, the prevalence of female sterilization was positively related to CEB. The percentage of sterilization was 0.6% for women with no CEB, 2.1% for women with 1–2 CEB, 14.0% for women with 3–4 CEB, and 41.1% for women with 5 or more CEB (p=0.000).
The percentage of sterilization was higher among women who did not read about family planning in newspaper/magazine in the last few months (18.6%) than those who have read about it in the newspaper (13.4%). The percentage of sterilization was higher among women who did not hear about family planning by text messages on the mobile phone (18.4%) than those who had heard about it by text messages on the mobile phone (13.4%). The percentage of sterilization was higher among women who had not been visited by a field worker (19.5%) than those who had been visited by a field worker (9.7%). The percentage of sterilization was higher among women who did not visit a health facility (19.5%) than those who had visited a healthy facility (9.7%).
3.3. Predictors of Female Sterilization Uptake
Table 3 presents the results of the logistic regression modelling. On the one hand, the variables, age, wealth status, work status, education, region of residence, total number of CEB, visited by a field worker in the past twelve months, and visited a health facility in the past twelve months, were significantly related to the use of female sterilization. On the other hand, place of residence, age at first sex, age at first marriage, age at the birth of first child, media, and marital status did not have a significant influence on female sterilization.
| - | 95% CI | ||
|---|---|---|---|
| Variables | OR | LB | UP |
| Region | - | - | - |
| Northern region | 1.587*** | 1.276 | 1.972 |
| Central region | 2.387*** | 2.084 | 2.734 |
| Southern region (R) | - | - | - |
| Urban | 1.013 | 0.835 | 1.229 |
| Rural (R) | - | - | - |
| Heard about family planning on the radio in the last few months | - | - | - |
| No | 0.921 | 0.801 | 1.058 |
| Yes (R) | - | - | - |
| Heard about family planning on the TV in the last few months | - | - | - |
| No | 0.769* | 0.603 | 0.981 |
| Yes (R) | - | - | - |
| Read about family planning in the newspaper/magazine in the last few months | - | - | - |
| No | 0.985 | 0.750 | 1.295 |
| Yes (R) | - | - | - |
| Heard about family planning by text messages on mobile phone | - | - | - |
| No | 0.985 | 0.750 | 1.295 |
| Yes (R) | - | - | - |
| Visited by a field worker in the last 12 months | - | - | - |
| No | 2.252*** | 1.829 | 2.774 |
| Yes (R) | - | - | - |
| Visited a health centre in the last 12 months | - | - | - |
| No | 1.860*** | 1.634 | 2.117 |
| Yes (R) | - | - | - |
| Marriage | - | - | - |
| Never married | - | - | - |
| Currently married | - | - | - |
| Formerly married | - | - | - |
| Work status | - | - | - |
| No | 0.771*** | 0.664 | 0.894 |
| Yes (R) | - | - | - |
| Age (years) | - | - | - |
| ≤ 30 years | 0.104*** | 0.079 | 0.136 |
| > 30 years (R) | - | - | - |
| Age at first sex (years) | - | - | - |
| <18 | 0.983 | 0.815 | 1.186 |
| ≥18 (R) | - | - | - |
| Age at first marriage (years) | - | - | - |
| <18 | 1.098 | 0.935 | 1.290 |
| ≥18 (R) | - | - | - |
| Age at birth of first child (years) | - | - | - |
| <18 | 1.101 | 0.947 | 1.281 |
| ≥18 (R) | - | - | - |
| Children ever born | - | - | - |
| 0 | 0.163*** | 0.119 | 0.223 |
| 1–2 | 0.408*** | 0.352 | 0.473 |
| 3–4 | - | - | - |
| 5+ (R) | - | - | - |
| Education | - | - | - |
| None | 2.102*** | 1.634 | 2.703 |
| Primary | 1.488*** | 1.206 | 1.835 |
| Secondary+ (R) | - | - | - |
| Wealth | - | - | - |
| Poor | 0.599*** | 0.510 | 0.704 |
| Middle | 0.744*** | 0.626 | 0.883 |
| Rich (R) | - | - | - |
| Media exposure | - | - | - |
| No exposure | 0.952 | 0.826 | 1.097 |
| Any exposure (R) | - | - | - |
| Type of marriage | - | - | - |
| Monogamy | 1.038 | 0.877 | 1.229 |
| Polygamy (R) | - | - | - |
Women aged 30 years and older were more likely to undergo female sterilization compared to those younger than 30 years. The odds of being sterilized were lower among women younger than 30 years of age than those older than 30 years (OR=0.104, 95% CI=0.079-0.136, p=0000). Women residing in the Northern region were 1.587 times more likely than those residing in the Southern region to use female sterilization (OR=1.587,95% CI=1.276-1.972, p=0.000). Women residing in the Central region had 2.387 higher odds compared to those residing in the Southern region (OR=2.387, 95% CI=2.084-2.734, p=0.000). The odds of being sterilized for women who had not heard about family planning on the TV in the past few months were 0.769 times lower than those who had heard about family planning on the TV (OR=0.769,95% CI=0.603-0.981, p=0.034). The odds of being sterilized were 0.163 times lower for women who had no CEB compared to their counterparts with 5 or more 0–3 CEB (OR=0.163, 95% CI=0.199-0.223, p=0.000). The odds of being sterilized were 0.408 times lower for women who had 1–2 CEB compared to their counterparts with 5 or more CEB (OR=0.408, 95% CI=0.352-0.473, p=0.000). The odds of being sterilized for women who had no education were 2.102 times higher than those who had secondary and higher education (OR=2.102,95% CI=1.634-2.703, p=0.000). The odds of being sterilized for women who had primary education were 1.488 times higher than those who had secondary and higher education (OR=1.488, 95% CI=1.206-1.835, p=0.000). The odds of being sterilized for women who were poor were 0.599 times lower than those who were rich (OR=0.599, 95% CI=0.510-0.704, p=0.000). The odds of being sterilized for women in the middle wealth category were 0.744 times lower than those who were rich (OR=0.744, 95% CI=0.626-0.0.883, p=0.001).
4. DISCUSSION
The findings of this study have revealed the age of women to be significantly related to female sterilization. Female sterilization was higher among older women (>30 years) than younger women. This result is in agreement with the findings from other studies, including Columbia [24], Ethiopia [25], India [26], Uganda [22], Pakistan [27], and Bangladesh [23]. This may be because a sizeable proportion of the younger women have not yet started childbearing and are yet to implement their fertility desires and aspirations. They may choose short-term reversible methods that are suitable for spacing between childbirths over those that limit childbirths.
This finding may also be linked to differences in onset and intervals of childbearing between young and older women. Older women are more likely to have exceeded their ideal number of children, whereas young women are just beginning their childbearing careers and have been recently exposed to contraceptive knowledge and services. In addition, the finding that female sterilization was high among old women may be attributed to some service providers who feel that a woman should have permanent contraception after a certain age bracket. Furthermore, older women are likely to have explored all other temporary contraceptive options and experienced adverse effects, yet they harbour no intentions of bearing more children, compared to their young counterparts who may want to have space for a short time. In some communities, women are afraid to undergo sterilization for fear that if they are divorced and remarry, the new husband may want to have a child with them, and if they are sterilized, then this may not be possible. This hindrance may be more serious among younger women than older women who may consider themselves to be outside the marriage market.
The number of CEB was found to be associated with female sterilization uptake. This finding is in agreement with results from other studies, including Brazil [28, 29], Columbia [24], Ethiopia [25], India [30, 31], Nigeria [32], Uganda [22], Pakistan [27], Iran [33], and Bangladesh [23]. This may be probably because the use of female sterilization is based on the achieved fertility. Given that female sterilization is permanent and irreversible, women who have not yet accomplished their desired or wanted fertility are less likely to use it. Furthermore, women with many children may decide to stop childbearing and choose to use sterilization. It is perhaps not very surprising since most users of female sterilization are those who do not wish to have any more children.
This study has also revealed the relationship between female sterilization and wealth status to be positive and significant. With the rising wealth status of women, the uptake of female sterilization also increases. This finding is consistent with results from Bangladesh [23], Ethiopia [34], and Zambia [35], but in opposition to findings from Uganda [22] and India [26, 30, 36] that have shown a higher use of female sterilization among poor than rich women. Earlier studies in Malawi have shown the importance of wealth status in influencing the contraceptive use [7, 14]. A study conducted in Zambia claimed that the positive relationship between female sterilization and wealth status could be explained in terms of the theory of wealth flow, which argues that in poor communities, wealth flows from children to parents, whereas in rich societies, the opposite is true. In such cases, among rich families, women are more likely not to desire more children and, as such, resort to using female sterilization. In addition, women from rich households tend to have bigger aspirations; they enter marriages late and delay childbearing probably because they are in school or busy looking for jobs and money. On the other hand, women from poor households enter marriages early and also begin childbearing early and desire more children. It is poor women who are likely to regard children as a source of wealth and a means of old age security.
The uptake of female sterilization was also found to be significantly related to the work status of women in this study. The use of female sterilization was observed to be higher among working women than non-working women. This is consistent with findings from other studies [23, 30, 34]. One possible explanation may be that childbearing and rearing compete with work aspirations. As such, working women would rather use female sterilization to limit the number of CEB in order for them to concentrate on their careers and work. Working women are also likely to have financial and material resources that they can use to access female sterilization. Another factor could also explain this relationship, that is, high-status women have easy access to family planning methods, including female sterilization, compared to low-status women who may have financial constraints.
This study has also found a negative significant relationship between education and female sterilization. The prevalence of female sterilization has been found to be higher among women with no education than women with some education and, as female education has increased, the uptake of female sterilization has been found to decrease. This is rather unexpected, but it has been found in other studies [24, 29, 31, 33, 36]. One possible explanation could be the consequence of the design of family planning programs, which tend to target underprivileged communities. It is also possible that women who are educated are not only knowledgeable of various types of contraceptives and their merits, but also use other methods.
The study has also found the use of female sterilization to be high among women who have not been visited by a field worker in the past twelve months. In addition, the use of female sterilization has been found to be high among women who have not visited a health facility in the past twelve months. These results are unexpected since one would expect the uptake of sterilization to be high among those women who may have been visited by a field worker in the past twelve months, or women who had visited a health facility in the past twelve months. It is possible that these women were not visited by field workers or they did not visit a health facility simply because they were sterilized. Often, when one is using female sterilization, the cost of accessing a health centre is minimised.
Region of residence has been observed to be one of the factors influencing the use of female sterilization. Women residing in the Central region and the Northern region were more likely to use female sterilization than their counterparts in the Southern region. Regional differences in the use of female sterilization have also been reported in other countries, including Bangladesh [23], Brazil [28, 29], India [30, 36], and Zambia [35]. This could be attributed to the distribution of health facilities and the characteristics of the population residing in each region. Studies indicate that in most developing countries, there are regional disparities in the distribution of medical and health facilities. In Malawi, in the 70s and 80s, the distribution of health facilities was better in the Northern region, followed by the Central region, and worst in the Southern region. The regions that are better served with medical and health facilities tend to have a higher use of female sterilization than their counterparts. In addition, other characteristics of the region of residence may help to increase the use of female sterilization. A study in India reported a higher contraceptive use in the more developed and urbanized state of Andhra Pradesh (63%) than in Uttar Pradesh, one of the most economically and socially underdeveloped states [36].
Lastly, the study found media exposure to not be significantly associated with the uptake of sterilization. The same can be said for such variables as having read regarding family planning in the newspaper and having heard about it on the radio. However, having heard about family planning on the TV in the last few months was marginally associated with the uptake of sterilization. Exposure to media has been shown in previous studies to have a positive association with the uptake of sterilization [26]. However, in this study, the fact that over 82.2% of the women resided in rural areas, where access to media is hard and not sustainable due to the costs involved, might partly explain the non-significant findings. The finding of the high use of female sterilization among those who had heard about family planning on the TV in the last few months could be attributed to the high association of TV ownership with other social and economic factors.
5. STRENGTH AND LIMITATIONS
One strength of this study is that the analysis used the nationally representative data from the latest round of MDHS, which has enabled to understand the association of female sterilization with selected social and economic factors. However, there are some limitations associated with this study. First, the study did not collect information on the attitudes towards female sterilization and why women decided to use this method. Second, although there are certain variables that could have been used to enrich this study, such variables, like women's autonomy and decision-making power in this aspect, were excluded. Third, given that contraceptive use is still a sensitive subject in Malawi, there may be a high likelihood of underreporting, as it cannot be denied that some women may refuse to divulge their responses on this topic.
CONCLUSION AND FUTURE IMPLICATIONS
The use of female sterilization has increased among women in Malawi over the past two decades (1992–2016). However, there is still a need for efforts to increase contraceptive prevalence in the country in order to allow women to meet their fertility desire and improve their quality of life. The findings indicate that while female sterilization uptake in Malawi is low by global standards, it is high with respect to African standards. The uptake of female sterilization has been found to be higher among older women, women with more CEB, women residing in the Central region and Northern region, uneducated women, rich women, women who had not been visited by a field worker, and women who had not visited a health facility. Age, number of CEB, region of residence, education, wealth status, having been visited by a field worker, and having visited a health facility in the past twelve months have been observed to be significant predictors of sterilization uptake among the women. These significant factors need to be considered in designing programs to strengthen the existing national family planning program. For instance, the findings of this study suggest targeted interventions, such as facilitating access to female sterilization of women younger than 30 years of age, especially those who have achieved the desired family size, and improving the regional health services of the Southern region to improve access to sterilization and quality of family planning. The government and other implementing partners should offer awareness campaigns and counselling services related to female sterilization targeting higher parity women (4+ CEB) residing in under-served areas, such as the Southern region. In order to promote the use of female sterilization, there is a need for integrating economic empowerment activities and family planning services. There is also a need for a qualitative study to determine the characteristics of users of female sterilization and the factors related to high sterilization prevalence in Malawi.
NOTES
1 The percentage of contraceptive use is the percentage of women of reproductive age who are currently using the method. This is calculated as the number of women aged 15-49 who are currently using any method divided by the number of women of reproductive age, multiplied by 100.
LIST OF ABBREVIATIONS
| CEB | = Children Ever Born |
| CI | = Confidence Interval |
| DHS | = Demographic and Health Survey |
| ICF | = Inner City Fund |
| IUD | = Intra-uterine Device |
| OR | = Odds Ratios |
| TV | = Television |
| MDHS | = Malawi Demographic and Health Survey |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE.
Permission was obtained from Measure DHS to access and use the 2015–16 MDHS dataset for this study. Ethical review and approval for procedures and questionnaires for standard DHS surveys have been provided by the ICF Institutional Review Board and National Health Sciences Research Committee in Malawi [6].
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All human procedures followed were in accordance with the guidelines of the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
All respondents provided their informed consent for inclusion before they participated in the study [6].
AVAILABILITY OF DATA AND MATERIALS
The source of data that support the findings of this article are available in the DHS archive at https://dhsprogram.com/data/datasett/Malawi_Standard-DHS_2015.cfm?flag=0. Additional information about the data and conditions for access is available upon registration and request to DHS program- http://dhsprogram.com. Permission from the DHS program is required to access the data.
ACKNOWLEDGEMENTS
Declared none.


