All published articles of this journal are available on ScienceDirect.
Development of a Conceptual Framework to Guide Uptake of PhD-generated Knowledge by Policymakers
Abstract
Background:
A few frameworks have been developed to guide the translation of research findings into policy in low-resourced countries. However, none of the frameworks are specific for PhD work and this often results in the work not being fully utilized for policy development.
Objective:
This paper aimed to develop a framework tailored to facilitate the uptake by policymakers of knowledge generated from PhD studies in countries with limited resources.
Methods:
Qualitative data were collected from 10 College of Health Sciences Leadership and 4 Department of Health personnel as well as from content analysis of 29 PhD theses. Quantitative data were collected through an online questionnaire administered to 47 PhD, 11 Ph.D final year students and 21 Ph.D supervisors. The framework was inspired by and adapted in part from the KTA framework.
Results:
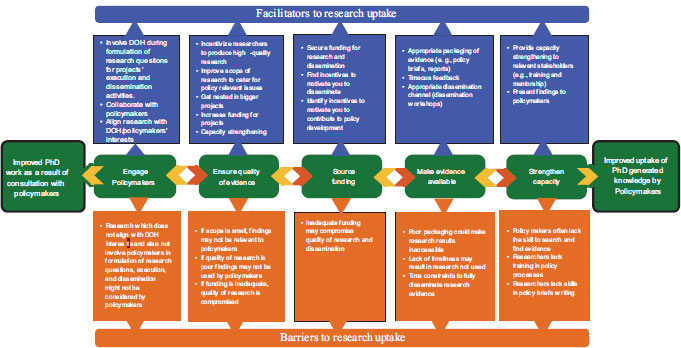
The conceptual framework that emerged from the study consists of three main concepts namely (a) barriers of research uptake, (b) facilitators of research uptake, and (c) stages of knowledge uptake. Each concept has several constructs. For each barrier, there is a facilitator which makes it easy for translation to take place and for each barrier and facilitator, there is a knowledge uptake stage to be followed for translation to take place.
Conclusion:
The framework can be used to facilitate the uptake of knowledge generated from PhD studies by policymakers in the South African context. We consider this framework unique as it is, to our knowledge, the first one that is specific for the translation of Ph.D work.
1. INTRODUCTION
In the last decade, there has been unprecedented global interest in the promotion of the use of research evidence to inform policymaking in the health sector [1]. It is acknowledged that high quality research and the generation and application of knowledge are critical for achieving internationally agreed health-related goals including those contained in the United Nations Millennium Development Goals (MDGs) and, now the Sustainable Development Goals (SDGs), especially in low and middle income countries (LMICs) [1]. Knowledge generated through health research has the potential to improve health outcomes, promote service delivery and strengthen health systems functioning [2, 3].
South Africa is endowed with historically strong research institutions that have platforms for knowledge translation, for example, the Centre for Evidence-based Healthcare at Stellenbosch University, the Knowledge translation unit at the University of Cape Town’s Lung Institute and the South African Medical Research Council which houses the Cochrane African Network (CAN). All these institutions actively focus on the production, synthesis, and use of health research in policy-making and practice [4]. However, despite the huge database of research findings, translation of research findings into health policy has been limited [5]. PhD work which by nature should be innovative and groundbreaking has remained in university libraries and journals with very little being accessed by policymakers. This has created the so-called know-do gap [6].
In response to the know-do gap, many frameworks and models have been developed to guide the uptake of research evidence by policymakers. The Promoting Action on Research Implementation in Health Services (PARIHS) framework was founded in 1998 by Kitson et al. to provide an alternative to existing one-dimensional models of transferring research to practice [7]. PARIHS framework views successful research uptake as a function of the relationships between three domains, namely evidence, context, and facilitation. The CAHS framework which is mainly referred to as the Canadian Academy of Health Sciences (CAHS) Payback Framework was adapted from the payback model developed by Buxton and Hanney in 1996. The framework aims to capture specific impacts in multiple domains, at various levels and for a wide range of audiences to determine how research activity influences decision-making [8]. The IOWA model was founded by a group of nurses from the University of Iowa hospitals, Iowa clinics of Nursing College in 1994. The model is intended to use research findings to improve healthcare quality, monitor healthcare costs and improve nursing practice [9, 10]. The above-mentioned frameworks and models were mostly tailored for use in high-income countries [8-11].
There are, however, some frameworks that are applicable to LMICs. Sigudla and Maritz developed a research uptake model for low-resourced countries experiencing competing priorities [12]. Their model recounts specific behaviours and activities associated with research uptake for individual stakeholders and is also believed to lead to a better working relationship between researchers and research users [12]. Kim et al. developed a four-phase research utilization framework that illustrates the process of translating research evidence into policy [13]. The framework emphasizes evidence use throughout the translation process and is applicable to LMICs. Another notable framework is the Knowledge-to-Action (KTA) framework which was developed in Canada by Graham and colleagues in 2006. The KTA framework is a conceptual evidence-based framework developed in response to the confusion caused by the numerous terms used to describe the process of translating knowledge into action [14]. The KTA framework allows the identification of barriers to the use of knowledge and the transfer of knowledge to action into manageable sections. The KTA framework was included as one of the six pillars of the EcoHealth research approach [15]. However, most of the frameworks are rather academic and too complicated to capture the complexity of the processes involved and hence not user-friendly for policymakers [16-19]. None of the frameworks available have specifically dealt with how work generated from PhD studies can readily be used for policy formulation. Thus, there is need to develop effective and novel frameworks that are appropriate for the uptake of PhD work. To address this gap, we developed a framework specific for uptake of work from PhD studies by policymakers.
1.1. Study Design
The outcomes of a scoping review and three primary data papers contributed towards the construction of the framework. The study adopted a convergent mixed methods design. The process included conducting research and a scoping review and then integrating findings from both components for further analysis and framework development. The framework was informed by key findings from research and the scoping review. The methodology involved extracting and synthesizing key research outputs from the scoping review and research study. A mixed method convergent design was utilized to collect quantitative data using a questionnaire to collect data from 47 PhD graduates, 11 PhD final year students and 21 PhD supervisors, and qualitative data from in-depth interviews with 10 academics and 4 Department of Health (DOH) personnel, and content analysis of 29 PhD theses. A mixed methods approach was implemented to understand participants’ perceptions of the factors that influence the utilization of doctoral research findings in policymaking, to identify the barriers and facilitators of translating doctoral research into policy, and to integrate the data together to provide the broadest possible understanding [20]. Qualitative and quantitative data were collected and analyzed during a similar timeframe.
The two forms of data were analyzed separately and then merged [21-25]. We employed a case study framework in which both qualitative and quantitative data were collected to build a comprehensive understanding of the case [26, 27]. The research strategy includes content analysis of PhD theses, exploratory case studies and a scoping review. Amaratunga and Baldry describe a case study as strategy that focuses on understanding the dynamics present within single settings [28]. A case study is an empirical inquiry that investigates a contemporary phenomenon within its real life context, especially when the boundaries between phenomenon and context are not clearly evident [29]. A distinguishing feature of the case study approach is the comprehension of the study’s processes of occurrence within a given context interviewing participants and providing preliminary answers [30]. We chose to use the approach of synthesizing the evidence from the broader research to develop the framework. Evidence synthesis involves the analysis and compilation of evidence from multiple sources of data which makes findings and discussions richer and broader. Our aim was to bring in all the evidence we gathered quantitatively, qualitatively and through the scoping review published as four separate articles. This framework which we present is a summative outcome of the whole process and hence incorporates ideas from across each article.
2. METHODS
The paradigm of pragmatism guided the study. The study aims at developing a framework to facilitate the uptake of PhD generated knowledge by policymakers with particular emphasis on developing countries; hence, the adoption of the pragmatic approach of ‘what works’ in finding appropriate answers to the research questions [21]. We adopted a pragmatist position because it allowed us to have a pluralistic stance of gathering all sorts of data to best answer the research questions [31]. Qualitative and quantitative data were collected concurrently and analyzed separately in parallel and then merged for a complete understanding of the phenomenon and to compare individual results [31]. The two data sets were integrated to develop results and interpretations that expand understanding, are comprehensive and are validated and confirmed [21]. Qualitative and quantitative findings were integrated at the interpretation and reporting level of research through a staged narrative of the qualitative and quantitative findings [20, 21, 25, 32]. Qualitative and quantitative findings were synthesized through a narrative both in the results and the discussion sections. Findings from the qualitative were merged with the findings from the quantitative study.
The development of the framework for facilitating the smooth uptake of PhD generated knowledge by policymakers adopted a multi-phased approach. The first phase involved extracting and summarizing evidence from a scoping review of the barriers and facilitators of translating health research into policy in sub-Saharan Africa (SSA) [33]. The scoping review identified generalized but critical recommendations emerging from prior studies to improve the translation of research findings into policy in sub-Saharan Africa. The second phase involved generating evidence using a mixed methods approach which involved a document analysis exercise that included reviewing PhD theses and work published by PhD graduates (Damba et al, Unpublished). The third phase involved generating evidence using a quantitative approach and descriptive study design paper (Damba et al., Unpublished). The fourth phase involved the assessment of the perceptions of academics on the factors influencing the translation of Ph.D. generated knowledge into policy using a qualitative approach (Damba et al, Unpublished). The fifth phase involved the integration of findings through merging quantitative, qualitative, and scoping review findings. The sixth phase involved framework development which is the focus of the paper.
2.1. Ethical Considerations
The study was approved by the research ethics committee of the university, the Biomedical Research Ethics Committee (reference number BREC/00001384/2020) and the Kwa-Zulu-Natal Provincial Department of Health (reference number KZ_202008_030). All research was performed in accordance with the ethical standards of the institutional research committee applicable when human participants are involved. Written informed consent was obtained from all the participants in the study.
2.2. Development of a Framework to Facilitate Smooth Uptake of PhD Generated Knowledge by Policymakers
The proposed framework (Fig. 1) is inspired by the KTA framework developed by Graham et al. [14] and utilizes findings from phases 1 to 4. The study did not wholesomely adopt the KTA framework’s guiding statements but adopted some key concepts from it. The KTA framework was used in an integrated way signifying that the KTA framework was used as a guide [34]. The KTA framework was used to organize the concepts that emerged from the analysis of the combined findings from the research study and the scoping review. Key concepts from the Knowledge creation and Action cycle phases were adopted to suit the context of the study. We addressed the criticism of KTA regarding its lack of distinct phases and details on what should be done at each phase. We applied two phases of the Knowledge creation cycle, and these include tailoring knowledge to the needs of the users and the product tools such as policy briefs. At least four of the possible seven phases of the Action cycle were applied and these include: identifying the problem/identify, reviewing, selecting knowledge, adapting knowledge to local context, assessing barriers to local use and selecting, tailoring, and implementing interventions. Our own experience also contributed to the development of a simplified framework that we believe can guide the uptake of PhD-generated work by policymakers.
We developed a new framework inspired by other frameworks. The first step to developing the conceptual framework involved searching and reading some literature on frameworks on research utilization as a guide. The researchers reflected on the proposed components of the various frameworks and discussed how best to capture the components they had identified. This was followed by analyzing the barriers and facilitators of translating doctoral research findings into policy gathered from an analysis of the combined findings from a scoping review and research study. The barriers and facilitators were assessed for duplication and the remaining ones were reviewed and discussed by all the researchers. The researchers deliberated on what could generate a positive result in translating doctoral research into policy. The team made sure that the findings of the scoping review and research study were included so that they did not just base everything on the reviewed literature. The continuous refinement of the findings resulted in the initial draft model that created a foundation for the developing concepts to be included in the conceptual framework.
In the end, the research team evaluated and deliberated on the draft to clarify the specific concepts for inclusion. Researchers’ consensus on the feasible inputs was categorized into three sub-domains namely barriers, facilitators, and stages of uptake. The barriers and facilitators were further categorized based on the stages of knowledge uptake (engage policymakers, ensure the quality of evidence, source funding, make evidence available, and strengthen capacity). As a result, one or more barriers and facilitators were linked to one stage of knowledge uptake. Several changes and modifications were made as a result leading to the second draft of the framework which became the basis of a consultation process with the Department of Health personnel who had participated in the study to obtain further inputs to allow the assessment of the relevance of the framework components. The feedback from the DOH personnel was consolidated into the framework. The intention was to develop a framework appropriate for doctoral work.
We applied design research, also known as design-based research, which is an interactive and participatory research
involving close collaboration and interaction of researchers, innovation designers, and practitioners to amend the framework [35]. Since design-based research is cyclical in nature with more iterations, a single round of amendments could not be adequate [36]. Hence, multiple iterations facilitated improvements and re-evaluation of the framework ensuring that in every iteration, policymakers were involved thus increasing the chances of the intervention to be implemented [36]. We are therefore satisfied that the framework is of good quality for use in the uptake of PhD-generated knowledge.
2.3. Assumptions of the Framework
The development of any guiding principle rests upon the assumption that a gap between research evidence and actual practice can be significantly reduced by implementing evidence-based guidelines [37].
• The model acknowledges that despite the barriers to translation of research into policy, once knowledge is generated translation has to be implemented.
• Without effective strategies to facilitate research uptake, there will always be reliance on unscientific evidence.
• The framework will assist in identifying and managing barriers to research uptake and enable optimal uptake of public health research findings.
2.4. Description of the Conceptual Framework
According to the KTA framework, effective uptake of research findings requires the assessment of barriers to knowledge use as asserted by several scholars that public health research uptake depends on considering several local barriers and applying tailored research uptake strategies to overcome those barriers [38]. The framework that emerged from this study presents the barriers to the uptake of doctoral research findings and facilitators to produce the required outcome of improved uptake of PhD generated knowledge. The framework (Fig. 1) comprises three main concepts which are (a) barriers to research uptake (bottom layer in red), (b) facilitators of research uptake (top layer in blue) and (c) stages of knowledge uptake (middle layer in green). The framework shows the bi-directional movement of arrows in the middle lane indicating that contributions are not only towards the uptake of research findings, but also when considered in retrospect, they can lead to improvement of the quality of studies. In fact, the process can either move from the direction of policymakers influencing research or researchers influencing policy. Hence, one end of the line shows the benefit accrued by policymakers from research while the other end shows the benefit accrued by researchers because of the influence of the policymakers.
Each concept has several constructs which are unpacked later under each main concept. Barriers are what could impede knowledge uptake and the facilitators are what should be done to counter the barriers. For most of the barriers, there is a facilitator which makes it easy for translation to take place. Although there were more barriers than facilitators with respect to the translation of doctoral research findings into policy, it is anticipated that the facilitators will drive the uptake of PhD work and allow the barriers identified to be overcome. Some of the facilitators address more than one barrier, for example, capacity strengthening serves as both a facilitator to ensure that research evidence is of high- quality and as a stage of knowledge translation. Stages of knowledge uptake are the stages that should be followed to facilitate the use of research findings in policymaking.
The framework demonstrates that the translation of research into policy is highly dependent on the identification of the barriers and facilitators that influence evidence-to-policy process, understanding them and knowing how to deal with them [39]. In this framework, the constructs are discussed in more detail below with the barriers to and facilitators of research uptake being discussed under the constructs of the stages of knowledge uptake. It was not practical to discuss them separately as it was going to be a repetition.
2.5. Barriers to Research Uptake
In addition to barriers mentioned in Damba et al., 2022, the research study identified the following barriers: not involving policymakers in the formulation of research questions, research not aligned to DOH/ policymakers’ needs, policymakers not aware of the availability of research findings, researchers’ poor appreciation of giving feedback, little production of policy briefs, lack of timeliness of research results, researchers’ lack of training in policy processes, inadequate funding for the dissemination of research findings, time constraints to fully disseminate research results, limited commitment to disseminate research findings, and lack of incentives to translate research. Barriers must be managed properly for the translation of research findings.
2.6. Facilitators of Research Uptake
In this model, the facilitators for research uptake are involving policymakers in research design, execution and dissemination stage, capacity strengthening for both researchers and policymakers, aligning research with policymakers’ needs, appropriate packaging of research results, use of policy briefs, increased funding for dissemination activities, getting nested in bigger projects, collaboration between researchers and policymakers, timeous feedback, and availability of high- quality usable research.
2.7. Stages of Knowledge Uptake
2.7.1. Engage with Policymakers
Engaging policymakers throughout the research process is critical for building trust, creating demand and ensuring relevance and accessibility of research evidence [40]. Building trust with policymakers can be achieved through responding to their priorities and needs, maintaining continuous and close relationships with them while creating demand for evidence can occur through enhancing awareness of policymakers on the importance of evidence-informed health policymaking, building capacities in accessing and using evidence and engaging policymakers in different steps of the process [40]. Strong networks linking researchers to policymakers are key to enhancing the translation of research into policy [41]. Researchers can effectively engage policymakers if they begin with the basics of understanding the policy community, becoming familiar with a policy institution’s decision-making process to determine the times and places where research is most likely to be used and understanding the policy culture where policymakers turn to information sources they know and trust [42]. Attempts to develop research findings into policy have often failed because researchers tend to decide on the research topic without including policymakers.
Researchers can avoid this pitfall by collaborating with policymakers to conduct a needs assessment to identify relevant research topics and build trust in the research findings [43]. Involving policymakers in prioritizing evidence gaps promotes ownership and political will that increases evidence use [44]. The problems researchers are interested in, do not always align with the priorities of policymakers [45]. Researchers need to know in advance what the needs of policymakers are and direct their research towards answering policy-related questions and making the evidence available in accessible language [46]. Promoting evidence-use requires ongoing engagement between researchers and policymakers and the involvement of relevant stakeholders in developing research agendas which increases the likelihood of evidence use [41]. The benefits of long-term collaboration between researchers and policymakers are that both parties learn to “speak the same language” as well as enabling policymakers to track emerging research findings rather than having to wait for end-of-project dissemination activities [47]. Weak researcher-policymaker linkages hamper the use of evidence [33].
2.7.2. Ensure Quality of Evidence
Ensuring that evidence is of high- quality facilitates the translation of research into policy. Quality of evidence can be enhanced through collaboration between researchers and policymakers, increased funding for research and capacity strengthening of researchers [48, 49]. Inadequate funding will compromise the methodology of the research projects where for example, researchers will have to employ an inappropriate sampling method as a way of saving money. The quality of research evidence can be maintained by improving the scope of research to cater to policy-relevant issues. It is also essential to incentivize researchers to produce research that is of high quality [50].
3. RESULTS & DISCUSSION
3.1. Source Funding
Researchers should source funding to conduct domestically relevant research to facilitate the translation of research into policy. Limited funding for doctoral research results in poor research output [51]. Several studies have identified the inadequacy of funding for research as a major barrier to institutional evidence generation in LMICs [52-54]. Without adequate funding researchers will not be able to fully disseminate research findings to policymakers and other stakeholders. There are various ways in which doctoral students can alleviate the problem of lack of funding for research and dissemination of research findings to relevant stakeholders. Students can source funds from philanthropists and institutions operating locally to sustain homegrown research [55]. Students can also conduct research on an objective of their supervisor’s bigger projects. Students should be able to attract funding by enticing policymakers to co-sponsor research projects. This may be made possible by involving them in the formulation of research topics for the projects. Availability of funding can incentivize researchers to generate evidence knowing that they have adequate financial support [56].
3.2. Make Evidence Available
Making evidence available in accessible formats and appropriate dissemination channels could facilitate policy discussions and improve the use of research [57]. Policymakers should be able to access useful research that is accessible, addresses policy problems and communicate findings persuasively [58, 59]. Policy briefs which are a useful and non-academic knowledge transfer strategy may be a major strategy for facilitating research findings to policymakers and the ability to develop them is essential for researchers to facilitate evidence-use in policy [60, 61]. Policy briefs should be presented in formats and language that policymakers are familiar with ensuring that they offer actionable recommendations [62, 63]. The researchers ‘inability to craft and communicate policy recommendations from research hinders evidence use in policymaking [64]. In Ghana Araujo de Carvalho et al. reported that policy briefs were used to define priority problems and health systems responses to ageing and health [65].
PhD students are not equipped with the skills to develop policy briefs and the inability of researchers to craft and communicate policy recommendations is an obstacle to evidence use [64]. It is essential for researchers to acquire policy brief writing skills to facilitate evidence use in policy [60]. Communication of timely feedback to policymakers has the potential to facilitate the uptake of research evidence [66]. This is made possible through regular interaction between researchers and policymakers as well as dissemination workshops. Dissemination workshops are desired by a multitude of stakeholders as they allow users and researchers to collaborate, ask questions, and inspire the next set of research questions [67]. Research findings can also be made available through a platform that consolidates research evidence to make it more accessible and useful to policymakers [45]. A well-organized repository for research findings can also be used as a channel for disseminating research results.
3.3. Strengthen Capacity
There is a need to strengthen the capacity of policymakers to understand and use research evidence in policy decisions [68]. On the other hand, there is a need to strengthen researchers’ capacity for policy brief writing as well as their capacity to organize policy engagement [41]. Findings from previous reports suggested that among major barriers to the uptake of research evidence into policy is the capacity constraints to acquire, access, adapt, and apply available research evidence into policy [69-71]. Interventions to strengthen capacity include training programmes and workshops, increasing access to research, promoting frequent interaction between researchers and policymakers, and increasing policymakers’ receptivity towards research evidence [72]. Workshops conducted with the goal of fostering mentorship and collaboration between researchers and policymakers are ideal for facilitating uptake [73, 74]. If policymakers have no capacity or competencies to utilize research findings, it is unlikely that even the best available research evidence will be able to inform policies [75, 76]. Our easy-to-use and practical framework is specific for PhD studies. It shows what prevent PhDwork from being translated into policy and what needs to be done.
4. STRENGTHS AND LIMITATIONS
Like any other framework, this one also has limitations. The fact that the study was conducted in a single Public Health School and with a smaller number of participants limits the chances of generalizing the findings to the entire university; the findings are specific to health-related research and are more relevant to health policymakers. The framework still needs to be validated. However, the strength of this framework lies in it being the first framework to be developed for the uptake of health-related Ph.D. work in South Africa.
CONCLUSION
The potential benefits of the framework may extend beyond health researchers, policymakers and KZN-DOH. People from other settings where the study was not conducted may want to read the manuscript since the research is generally valuable and may be used as a basis for the development of similar frameworks for other disciplines of the economy. Since the framework appears to be potentially beneficial and applicable to diverse institutions, we hope that policymakers will apply it, validate its feasibility, assess its utility, and improve it.
AUTHORS’ CONTRIBUTIONS
F.U.D; N.G.M and M.J.C conceptualized the study. F.U.D, N.G.M and M.J.C contributed to data collection, analysis, writing and write-up of manuscript. N.M.G and M.J.C supervised the processes, reading all versions. All authors read and approved the final article.
LIST OF ABBREVIATIONS
| MDGs | = Millennium Development Goals |
| SDGs | = Sustainable Development Goals |
| LMICs | = Low and Middle Income Countries |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Biomedical Research Ethics Committee (reference number BREC/00001384/2020) and the Kwa-Zulu-Natal Provincial Department of Health (reference number KZ_202008_030).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants in the study.
AVAILABILITY OF DATA AND MATERIALS
The datasets analyzed during the current study are not publicly available due to privacy and ethical restrictions, but de-identified data may be available from the corresponding author [F.U.D] on special request and with appropriate institutional approvals.
FUNDING
The study was funded by the College of Health Sciences through a scholarship awarded to FUD by the University of KwaZulu-Natal. The funder had no role in the design of the study, collection, analysis, and interpretation of data and manuscript write-up.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise
ACKNOWLEDGEMENTS
The authors would like to thank the participants who took part in this study and the university for their library resources.


