All published articles of this journal are available on ScienceDirect.
A Monitored Self-isolation Model for Asymptomatic COVID-19 Patients to Prevent the Family-based Transmission
Abstract
Background:
Systematic effort and sustainable systems are highly suggested to avoid new family clusters of COVID-19 in a community. It was challenging that self-isolation should be monitored and evaluated to prevent the transmission.
Purpose:
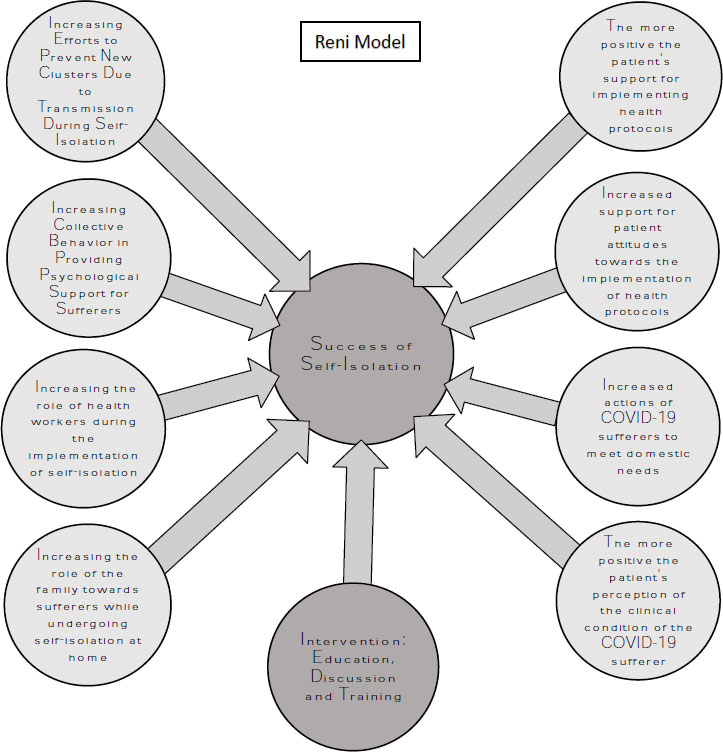
This study aimed to develop and evaluate a monitored self-isolation model, named the “Reni-Model,” for asymptomatic COVID-19 patients to prevent family-based transmission.
Methods:
A mixed-methods approach with an embedded design was employed. The Reni-Model incorporated a moderating factor of patient empowerment through education, participatory discussions, and training. The model was developed through an analysis, design, development, implementation, and evaluation process. The study population was COVID-19 patients, their family members, healthcare workers, and the community in Deli Serdang Regency, North Sumatra Province, Indonesia, in 2022. The respondent characteristics correlated to the self-isolation model's success are gender, education, occupation, and income.
Results:
Data implied several determinant factors, including patient knowledge, attitudes, actions, perceptions, family support, healthcare worker involvement, and collective behaviour, significantly influencing the success of monitored self-isolation. The Reni-Model demonstrated significant effectiveness in preventing the transmission of COVID-19 within families.
Conclusion:
This study emphasises the importance of prioritising and taking concrete actions to implement monitored self-isolation, drawing valuable lessons from the COVID-19 pandemic.
1. INTRODUCTION
At the end of 2021, WHO reported the prevalence of COVID-19 in the Province of North Sumatra, Indonesia, has 632,568 confirmed positive, 22,653 deaths, and a 3.58% fatality rate, which means it was above the average national fatality rate of 2.17% [1, 2]. To prevent the spread of COVID-19, the Indonesian government has instructed prevention and mitigation through various policies. Indonesian Law No.6 of 2018 mentioned that quarantine is an effort to prevent and ward off the entry or exit of diseases and public health risk factors that can potentially cause public health emergencies. The term isolation refers to separating sick people from healthy people in healthcare facilities to get treatment and care [3]. In this regard, self-isolation is the separation of COVID-19 patients from healthy people within a specific limit of 10 days from the day of collecting specimens for asymptomatic patients and an additional three days for symptom-free patients [4].
Meanwhile, patients with moderate and severe symptoms of COVID-19 will be advised to undergo hospitalisation [5]. In the confirmed cases that self-isolated at home, health officers carried out the monitoring process in coordination with the local health office [3]. Monitoring can be done by telephone or periodic or daily visits and recorded on the daily monitoring form. Monitoring was carried out through body temperature checks and daily symptom screenings. If isolation and monitoring are completed, a statement letter can be given using the attached form [4]. Self-isolation is one of the government policies considered effective in controlling the transmission of COVID-19, whereas the capacity of healthcare centres and centralised isolation facilities are minimal. Furthermore, the advantages of the self-isolation strategy are more accessible and more negligible psychological impact [6].
Instead of financial support from the government, self-isolation challenges several factors such as the unavailability of sufficient food in the family [7], weak monitoring by the Public Health Centre [8], the inadequacy of the house as a place of self-isolation [9], lack of knowledge on the rules of self-isolation [10], delays for seeking the hospital and those who arrived at the hospital were already in severe and critical condition [11], the rise of new clusters within families and the patients were depressed in solitude [12]. Moreover, the risk of transmission to family members requires more significant financial support [13].
To deal with the weaknesses of the self-isolation system, the role of family members was crucial for monitoring the patient's condition and ensuring that the patient just stayed at home or not going anywhere for two weeks. However, the implementation of self-isolation was also supported by health workers in terms of monitoring by ensuring that family members stick to the health protocols concerning Guidelines for Examination, Tracing, Quarantine, and Isolation [4, 14]. Systematic effort and sustainable systems are highly suggested to avoid new family clusters that impact the COVID-19 mitigation process in a community [15]. It is challenging to monitor and evaluate self-isolation to prevent COVID-19 transmission [16].
In this study, we have developed a monitored model of self-solation named the “Reni-Model”. This model aimed to evaluate determinant factors correlated with the triumph of self-isolation, how to construct and develop a new model, and how to apply the monitored model in a natural environment to prevent transmission [17, 18]. This model was presented in a module system involving the isolation activities of COVID-19 patients at home for 14 days. Previous research evaluating COVID-19 isolation was conducted in Singapore [19]. However, there is no report on the effectiveness of monitored self-isolation in Indonesia, so this study can become a scientific basis for determining the sustainability of self-isolation protocol as one of the strategic modalities in preventing the transmission of COVID-19 at the family level.
2. METHODS
The research design used is a mixed method with an embedded design approach. The research comprises five stages: analysis, design, development, implementation, and evaluation (ADDIE). The data collection through ADDIE stages referred to a mixed-method research guideline [20]. This research was conducted from March to September 2022 in Deli Serdang Regency, Province of North Sumatra, Indonesia.
2.1. Analysis Stage
The analysis stage was an explorative-qualitative method via in-depth interviews with direct observation or face-to-face. Informants are asymptomatic COVID-19 patients who conducted self-isolation (10 persons) and the health workers in the Public Health Centre handling COVID-19 cases (5 persons). Informants were selected by purposive sampling based on the appropriateness and adequacy of knowledge of the topic. We found that none of the participants refused to participate, and no one else presented except the participants and researchers. Triangulation of data sources was carried out to validate the qualitative results. At this stage, determinant factors correlated with the triumph of self-isolation have been identified.
2.2. Design Stage
The design stage was conducted as an expert interview to construct the design of a new model based on the previous analysis stage. Informants are experts in public health, task forces of COVID-19, module experts, and communication experts. The design stage started with preparing a draft module, which was then submitted to the informant as material for discussion and in-depth interviews. In this stage, module documents have been drafted.
2.3. Development Stage
In the development stage, three experts have been involved in the feasibility test by reviewing the module with the questionnaires on a Likert scale. An acceptability test by asymptomatic COVID-19 sufferers, family members, and health workers was conducted using Likert scale questionnaires. All stakeholders also gathered in one day of focus group discussion to evaluate the intervention model. In this stage, some advice has been attained from the feedback of all participants to develop a final module concept.
2.4. Implementation Stage
At this stage, a quantitative research method was applied. Analysis used a quasi-experimental pre-test and post-test in asymptomatic COVID-19 sufferers with self-isolation. Sample selection was carried out based on symptoms, not on PCR. The sample size was obtained using a total sampling technique of 30 people for the intervention group and 30 for the control group. Inclusion criteria were 18-45 years old, having no comorbidities, being willing to be disciplined during self-isolation, having good communication, and being ready to be a respondent. Informed consent was obtained from all participants in this study according to the Ethical Approval No. 700/UN.16.2/KEP-FK/2022. Exclusion criteria were rejected to sign informed consent, loss to follow, and worsening clinical symptoms.
Face validity was conducted early to ensure the as-prepared questionnaires could be easily understood. The validity and reliability tests of the questionnaire were carried out simultaneously. The questionnaire is valid if the Pearson correlation method's validity test calculation shows a significance value <0.05. Meanwhile, the questionnaire is reliable if Cronbach's Alpha value is > 0.6 [6]. Questions not meeting the validity and reliability tests will be eliminated and not included in further data analysis. Intervention or no intervention will occur on the subjects for ten days. After that, the issues will be given a post-test questionnaire on a Likert scale. Data were then classified into nine coded themes of questions and then presented in a matrix form.
2.5. Evaluation Stage
The matrix form was divided into four themes: ease of use of the module, clarity of module content, attractiveness of the module, and the relevance of the module content. The matrix form has fully covered the data obtained from the focus group discussion and the interview results. Data analysis according to the theme by sticking to the goal.
Statistical data analysis of pre-and post-intervention using a paired t-test to determine whether there is an increase concerning intervention. A selection of questions was based on the total item of the correlation validity test using Smart PLS to obtain an accurate score for each variable. After receiving the appropriate question items, latent variable analysis can be carried out with the Confirmatory Factor Analysis (CFA) technique to assess the suitability of the question construct to the model. Evaluation of goodness of fit for reliability testing using Smart PLS. Independent variables (age, education, economic status, occupation, ethnicity, gender, knowledge, attitudes, actions, perceptions, family members, and health workers) will be displayed in proportion (percentage). Comparison of pre-test and post-test scores was statistically analysed using a paired t-test. The p-value < 0.05 was considered a statistically significant difference.
3. RESULTS
3.1. Qualitative Data
Some patients complain about their experience at the hospital, thus influencing reasons for choosing self-isolation instead of inpatient hospitalisation. Another reason is that the recovery would be much easier while at home. Eating, sunbathing, resting, sports activities, and cooking are the main activities during self-isolation. The duration of self-isolation ranged from 1 to 4 weeks, depending on the different endurance levels. A more robust immune system means the time of the self-isolation until recovered will be faster.
Protocols were applied during self-isolation, including disinfectant, towel, interaction, bathroom, wasted mask, washing hands, social distancing, PCR test, room sharing, using mask, and spraying. Informants have shown the highest obedience to using masks to avoid transmission to others. Supporting factors were the use of drugs and vitamins. The availability of drugs and types of medicines or vitamins can affect the speed of the healing process. The health workers also play a role in monitoring patients during self-isolation. So that patients can receive correct information directly from the health workers. Family members also play an active role by ensuring that those who are in self-isolation can be more enthusiastic or provide psychological support to speed up the healing period. Based on the observations and interviews, two main factors hinder the implementation of self-isolation, namely stress and negative stigma from society. The patients fear the public will discover that COVID-19 virus has infected them. The burden of accumulation of thoughts will lead to stress and weaken the immune system.
The results of in-depth interviews showed that the patient's level of knowledge about the importance of self-isolation was still inadequate. The patient's attitude was still negative, but they kept trying to comply with the health protocol set by the Public Health Centre. Due to mobility restrictions, the COVID-19 sufferer's response was not maximal enough to fulfil domestic needs. There were differences in the perceptions of informants as COVID-19 sufferers towards the clinical conditions while undergoing self-isolation at home. The lack of optimal role of the family members and health workers for sufferers was also identified. Collective behaviour in providing psychological support for sufferers and efforts to prevent new clusters were still not optimal.
3.2. Design of Module
We used qualitative data to develop an in-depth interview with three experts about determinant factors that result in constructing a monitored self-isolation model acceptable to COVID-19 sufferers, family members, health workers, and the wider community. The module's design was constructed based on expert comments with eight determinants as described below:
1. “Knowledge is one of the determinant factors expected to be able to design a better self-isolation module design.”
2. “Building a positive attitude is an aspect that determines the success of self-isolation through increasing patient discipline and adherence to health protocols while undergoing self-isolation.”
3. “Positive actions to meet domestic needs will determine the success of the self-isolation module, which is good and acceptable to everyone.”
4. “Building positive perceptions in clinical conditions is necessary to succeed in the monitored self-isolation modules.”
5. “The role of the family is essential in supporting the success of self-isolation in the form of recovering the patient's health as soon as possible so that the self-isolation module can be built and trusted by the wider community.”
6. “Health workers play an essential role in creating self-isolation modules that are good and acceptable to all parties, especially the wider community.”
7. “The collective behaviour of COVID-19 sufferers is an essential supporting element for each sufferer that will increase the success of self-isolation.”
8. “Avoiding the formation of new family clusters is an essential step so that the success of this new self-isolation model is genuinely acceptable to all parties, including the wider community.”
3.3. Development of Module
The addition of intervention or moderating variables aims to increase further the success of monitored self-isolation in preventing family-based transmission of COVID-19. The intervention variable used for module development is the empowerment or counselling of COVID-19 sufferers, which includes three indicators: (i) patient education by researchers, (ii) interactive discussion, and (iii) health workers training.
Consensus Decision Making Group (CDMG) consisted of three experts who stipulate that the implementation of the monitored self-isolation model in this study is in the form of a “Structured Module” focused on the COVID-19 sufferers undergoing affordable self-isolation, family members, and health workers as executors of empowering COVID-19 sufferers while undergoing monitored self-isolation and applied to a broader community. The feasibility test was referred to the module format with four assessment criteria, as presented in Table 1.
The development of a monitored self-isolation module in a diagram model is shown in Fig. (1).
3.4. Implementation of Reni-model
Implementation was conducted through empowerment with explanations about Reni's Monitored Self-Isolation Model. The number of intervention participants was limited to 30 COVID-19 sufferers, so the training process was sufficiently focused, and interactions with participants became more active. After the empowerment intervention was completed, participants were again given a questionnaire to evaluate whether there was an increase in knowledge, attitudes, actions, perceptions, family roles, the role of health workers, collective behaviour, and the possibility of new clusters in the family.
3.5. Evaluation of Reni-model
The respondents' characteristics of interventions and control groups are presented in Table 2.
| No | Assessment Criteria | Rating Results | ||
|---|---|---|---|---|
| Module Expert | Substantive Expert | Language Expert | ||
| 1 | Introduction | 80 | 82 | 81 |
| 2 | Presentation | 76 | 77 | 74 |
| 3 | Closing | 79 | 82 | 82 |
| 4 | Glossary | 82 | 81 | 78 |
| Mean | 79.25 | 80.50 | 78.75 | |
| Quotation | “The module is considered feasible to be followed up.” | “The module is feasible but needs intervention empowerment.” | “The language of the module is feasible.” | |
| No. | Characteristics | Frequency (f) | Percentage (%) |
|---|---|---|---|
| 1 | Age | - | - |
| - | Pre-Adult (< 21 years old) | 11 | 36.67 |
| - | Adult (≥ 21 years old) | 19 | 63.33 |
| 2 | Gender | - | - |
| - | Male | 13 | 43.33 |
| - | Female | 17 | 56.67 |
| 3 | Ethnicity | - | - |
| - | Non-Malay | 9 | 30.00 |
| - | Malay | 21 | 70.00 |
| 4 | Education | - | - |
| - | Basic | 14 | 46.67 |
| - | High | 16 | 53.33 |
| 5 | Occupation | - | - |
| - | Working | 12 | 40.00 |
| - | No job | 18 | 60.00 |
| 6 | Income | - | - |
| - | Low | 7 | 23.33 |
| - | Adequate | 23 | 76.67 |
| 7 | Family Members | - | - |
| - | < 3 persons | 9 | 30.00 |
| - | > 3 persons | 21 | 70.00 |
| 8 | Isolated Family Members | - | - |
| - | > 2 persons | 17 | 56.67 |
| - | < 2 persons | 13 | 43.33 |
| 9 | Success Indicator | - | - |
| - | Infected | 9 | 30.00 |
| - | Non-infected | 21 | 70.00 |
| - | Total | 30 | 100.0 |
| No | Determinant Factors | Pre- | Post- | ||
|---|---|---|---|---|---|
| f | % | f | % | ||
| 1 | Knowledge | - | - | - | - |
| - | Not good | 16 | 53.33 | 8 | 26.67 |
| - | Good | 14 | 46.67 | 22 | 73.33 |
| 2 | Attitude | - | - | - | - |
| - | Not good | 13 | 43.33 | 9 | 30.00 |
| - | Good | 17 | 56.67 | 21 | 70.00 |
| 3 | Response | - | - | - | - |
| - | Negative | 14 | 46.67 | 7 | 23.33 |
| - | Positive | 16 | 53.33 | 23 | 76.67 |
| 4 | Perception | - | - | - | - |
| - | Not good | 11 | 36.67 | 8 | 26.67 |
| - | Good | 19 | 63.33 | 22 | 73.33 |
| 5 | Family support | - | - | - | - |
| - | Not good | 12 | 40.00 | 7 | 23.33 |
| - | Good | 18 | 60.00 | 23 | 76.67 |
| 6 | Health Workers support | - | - | - | - |
| - | Not good | 14 | 46.67 | 8 | 26.67 |
| - | Good | 16 | 53.33 | 22 | 73.33 |
| 7 | Collective Behavior | - | - | - | - |
| - | Not good | 13 | 43.33 | 9 | 30.00 |
| - | Good | 17 | 56.67 | 21 | 70.00 |
| 8 | Family Cluster | - | - | - | - |
| - | Not Good | 12 | 40.00 | 4 | 13.33 |
| - | Good | 18 | 60.00 | 26 | 86.67 |
| 9 | Success Indicator | - | - | - | - |
| - | Not Good | 9 | 30.00 | 5 | 16.67 |
| - | Good | 21 | 70.00 | 25 | 83.33 |
| - | Total | 30 | 100.00 | - | - |
The socio-demographic data mentioned above is the data of trial respondents before developing the Reni-Model for the success of monitored self-isolation, which was applied in the Deli Serdang Regency. Univariate analysis of determinant factors before and after the intervention used category values (Good and Not Good) as presented in Table 3.
After conducting interventions in the form of education, participatory discussions, and training for COVID-19 sufferers conducted by researchers, there was a change or increase in the value of the determinant factors. The analysis of difference t-tests before and after the model through empowerment is presented in Table 4.
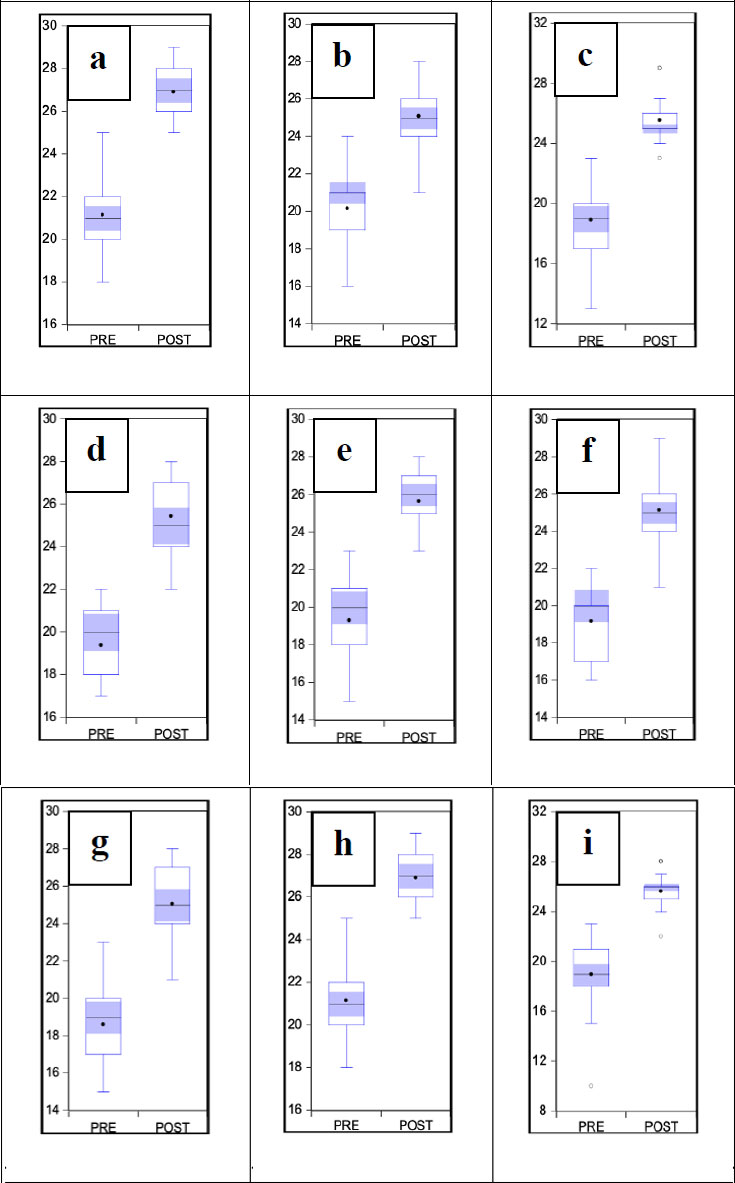
Table 4 clearly shows that the mean values of all variables increased significantly. These results exhibited that after developing the model to empower COVID-19 sufferers, there were improvements in all determinants, which is seen in the box-plotted data in Fig. (2).
| No. | Determinant Factors | Mean | Sig-p | ||
|---|---|---|---|---|---|
| Pre | Post | - | |||
| 1 | Knowledge | 21.13 ± 2.11 | 26.90 ± 1.21 | 0.000 | |
| 2 | Attitude | 20.13 ± 1.83 | 25.06 ± 1.83 | 0.000 | |
| 3 | Response | 18.90 ± 2.12 | 25.53 ± 1.40 | 0.000 | |
| 4 | Perception | 19.36 ± 1.62 | 25.43 ± 1.50 | 0.000 | |
| 5 | Family Supports | 19.30 ± 1.87 | 25.63 ± 1.40 | 0.000 | |
| 6 | Health Workers Supports | 19.16 ± 1.72 | 28.46 ± 1.50 | 0.000 | |
| 7 | Collective Behavior | 18.60 ± 2.11 | 25.03 ± 1.90 | 0.000 | |
| 8 | Family Cluster | 19.23 ± 2.06 | 23.63 ± 1.29 | 0.000 | |
| 9 | Success Indicator | 18.73 ± 2.50 | 25.60 ± 1.32 | 0.000 | |
4. DISCUSSION
This study showed that age characteristic was significantly correlated with the success of self-isolation (p < 0.05, OR = 3.393), whereas the more mature a person is, the smaller the chance of being infected by asymptomatic COVID-19. A study among South African adults reported that people without intimate relationships are more stressed than people with close relationships [21]. These results might correlate with the obedience to health protocol being higher in mature than younger persons, and the older are more cooperative in self-isolation at home [22]. Gender was also significantly correlated to the success of self-isolation (p = 0.05, OR = 4.083), that the majority of asymptomatic COVID-19 sufferers are female and the symptomatic COVID-19 sufferers are male. The literature has shown differences in gender in terms of social isolation, loneliness, social relationships, and quality of life [23]. Ethnicity was significantly correlated with the success of self-isolation (p < 0.05, OR = 4.481), whereas the non-Javanese had a higher percentage of infection than the Javanese. Certain ethnicities may face social and economic inequalities that may affect their ability to carry out self-isolation effectively [22]. Education was also significantly relevant to the success of self-isolation (p < 0.05, OR = 4.055), whereas the lower-educated person has more risk than the higher-educated person. This might be due to their obedience to the health protocol [24]. Occupation was also significantly related to the success of self-isolation (p < 0.05, OR = 5.153), indicating that the percentage of infected patients who do not work is higher than those who have jobs.
On the other hand, jobs that require physical interaction and contact with other people, such as jobs in the health sector, food service, and public transportation, can increase the risk of exposure to the virus and interfere with the effectiveness of self-isolation [25]. Our data showed that income level was correlated to the success of self-isolation (p < 0.05, OR = 3.578). In contrast, the percentage of infection experienced by those with inadequate income was higher than those with adequate income [26]. Higher income means more affordability to provide protection systems, sanitation, food and vitamin supplements, and supporting facilities at home [27]. Our study showed that the values of OR = 0.501 indicated that the number of family members did not significantly correlate with the success of self-isolation. However, the number of family members that undergo self-isolation correlates to the successful self-isolation program indicator (OR = 1.779) [28]. Furthermore, multivariate analysis of respondent characteristics revealed that the most significant factors of respondent characteristics are gender, education, occupation, and income, respectively.
To study more about determinant factors, bivariate analysis has been employed. Data showed that knowledge has a significant relationship with the success of monitored self-isolation in preventing transmission of asymptomatic COVID-19 (OR = 4.177). It is shown that the higher the knowledge, the higher the level of prevention or preparedness behaviour and the creation of successful self-isolation [18]. To increase the knowledge about self-isolation in the future, it is necessary to design a communication strategy that can reach groups with insufficient knowledge. This can be done by ensuring the proper way of communication and social media [29], and the most important is interpersonal communication among family members [30]. The bivariate analysis also proved that attitude has a significant relationship with the success of monitored self-isolation in preventing asymptomatic transmission of COVID-19 (OR = 4.375). A positive attitude will demonstrate adherence to health protocols, namely self-isolation, and increase the success of self-isolation itself [31]. This study also showed that action or response has a significant relationship with the success of monitored self-isolation in preventing transmission of asymptomatic COVID-19 (OR = 5.991). Adoption of positive behaviour might encourage respondents to adopt safe and effective practices to protect themselves from the disease [32]. Perception was also significantly correlated with the success of monitored self-isolation (OR = 4.890).
Suppose someone perceives the pandemic as a severe threat and understands that self-isolation protocols are essential to prevent the spread of the virus. In that case, they are more likely to adhere to self-isolation rules and take the necessary precautions [22]. The role of the family was significantly related to the success of self-isolation in preventing the transmission of asymptomatic COVID-19 (OR = 5.333). The households ensure that self-isolation protocols are correctly followed, such as ensuring that COVID-19 sufferers do not leave the house during the self-isolation period and do not interact with other people who do not live in the same house [33]. Adopting appropriate measures to maintain social and family relationships, maintain healthy activities, and manage emotions and psychiatric symptoms can help alleviate the dire consequences of loneliness and isolation [34]. Health workers' support was the significant factor related to the success of self-isolation (OR = 3.911). More than providing health information and medical support, health workers can monitor individual health conditions through online or telephone consultations. If the individual experiences worsening symptoms, the health workers can provide emergency supervision on what action must be taken. Health workers can also provide mental and emotional support, such as counselling and therapy [35]. Effective response to COVID-19 requires strong multi-sector coordination guided by strong leadership at all health system levels [28]. Community-based efforts must be integrated with existing health system infrastructure and aligned with plans and protocols supported by the Ministry of Health and local governments [32]. Collective behaviour was related to the success of self-isolation being monitored in preventing transmission of COVID-19 (OR = 5.116). This result might be because individual compliance with self-isolation rules was not only dependent on individual awareness and decisions alone, but the behaviour of other people around them also influenced it. Interactions between individual, social, and cultural contexts can influence engagement in some behavioural changes [36].
Moreover, the family cluster was significantly related to the success of monitored self-isolation (OR = 5.344). Transmission within family clusters is widespread. Most respondents who were not infected with asymptomatic COVID-19 were families who did not experience family cluster transmission [36-38].
CONCLUSION
Implementing monitored self-isolation at the family level was a systematic response to the rapid spread of COVID-19. Despite challenges such as stress and societal stigma, this study has exhibited the most significant characteristics of gender, education, occupation, and income, respectively. Moreover, it is proved that the identified determinant factors, including patient knowledge, attitudes, actions, perceptions, family support, healthcare worker involvement, and collective behaviour, significantly influenced the success of monitored self-isolation. The critical finding of this study is a developed “Reni-Model” in a module system incorporating education, participatory discussions, and training. Reni-Model has been proven an effective intervention accepted by COVID-19 patients, their families, healthcare workers, and the broader community. By addressing the barriers and providing empowering interventions, the Reni-Model enhanced the implementation of monitored self-isolation and preventing family-based transmission. These findings highlight the importance of comprehensive strategies considering the sociocultural context and actively involving various stakeholders in successfully executing self-isolation measures during the COVID-19 pandemic. It is greatly possible that our model to be developed in to a digitalized module, a more accessible and reliable for future implementation.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus disease 2019 |
| WHO | = The World Health Organization |
| COREQ | = Consolidated criteria for reporting qualitative research |
| PCR | = Polymerase Chain Reaction |
| PLS | = Partial Least Squares |
| OR | = Odds Ratio |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of the Faculty of Medicine, Universitas Andalas. Approval No. 700/UN.16.2/KEP-FK/2022.
HUMAN AND ANIMAL RIGHTS
No animal were used that are the basis of this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants of this study.
STANDARDS OF REPORTING
COREQ guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
This research was funded by Kemendikbudristek No. 086/E5/PG.02.00.PT/2022.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


