RESEARCH ARTICLE
Stigma in the Prolonged Pandemic: Insights from Nurses in Two Indonesian Provinces
Yosi Marin Marpaung1, *
Article Information
Identifiers and Pagination:
Year: 2024Volume: 17
E-location ID: e18749445292650
Publisher ID: e18749445292650
DOI: 10.2174/0118749445292650240312041029
Article History:
Received Date: 13/11/2023Revision Received Date: 25/02/2024
Acceptance Date: 28/02/2024
Electronic publication date: 24/04/2024
Collection year: 2024

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background
Nurses in Indonesia have faced extraordinary challenges amid the prolonged coronavirus disease pandemic, including stigmatization. However, much is understood about this experience only from the initial period of the pandemic.
Objective
This study aimed to shed light on the enduring intensity of stigma experienced by nurses in protracted health crises.
Materials and Methods
This study is a part of a research project titled “Exploration of Stigma Towards Nurses in Indonesia During the COVID-19 Pandemic,” conducted 1.5 years after the pandemic onset. A qualitative descriptive approach was used. Thirty-three nurses from both urban and rural settings who encountered stigma in two Indonesian provinces participated in individual interviews using a semi-structured guide. Thematic analysis through the Framework Method was employed for data analysis.
Results & Discussion
Three themes emerged: 1) the dynamic of stigma intensity during a prolonged COVID-19 pandemic; 2) nurses’ points of reference when elucidating this intensity; and 3) the perceived contributing factors to the stigma intensity in the protracted pandemic. Participants reported experiencing stronger stigma in the early period of the pandemic. In the later period, some manifestations of stigma persisted, although not as strongly as before. When describing the intensity, nurses often referenced the frequency and strength of emotions stemming from stigmatizing behaviors—such as avoidance, rejection, suspicion, negative rumors, and disparaging remarks about the nursing profession. Eight contributing factors to stigma intensity were identified.
Conclusion
Stigma intensity during the prolonged pandemic appeared to have similarities and distinctions with the phenomena observed in previous health crises. Continuous evaluation and mitigation efforts are imperative to alleviate the stigma experienced by nurses in protracted health crises. Understanding the contributing factors to the dynamic nature of stigma intensity is crucial for developing targeted interventions.
1. INTRODUCTION
Stigma is a complex social phenomenon [1] that is highly detrimental to both individuals and society across various dimensions of life [2-7]. Hatzenbuehler, Phelan, and Link, influential figures in the development of stigma knowledge, have asserted that stigma satisfies all factors that can persistently affect people's health for an extended period of time despite the dramatic changes in disease control [8].
In the context of health, attention to stigma affecting health workers needs to be strengthened. During disease outbreaks, healthcare providers are at significant risk of being stigmatized and suffering challenges that could impact their resilience and functioning [9]. Stereotyping and discriminatory behavior have persisted within this group during outbreaks of emerging diseases in the last decade, such as H1N1, Ebola, Zika, severe respiratory syndrome (SARS), and Middle East respiratory syndrome coronavirus (MERS-CoV), resulting in negative impacts on the well-being of healthcare workers [5-7, 10-12].
COVID-19, an emerging infectious disease, cannot be separated from the phenomenon of stigma. Since its emergence at the end of 2019, the stigma triggered by COVID-19 has affected health workers providing care throughout the pandemic [13-18]. The growing stigma associated with COVID-19 has led to physical violence, bullying, expulsion of health workers, refusal to access public facilities, and destruction of health services in various parts of the world [13, 14, 16, 18, 19], including Indonesia [15, 20, 21].
In Indonesia, nurses are one group of health workers affected by the stigma associated with COVID-19. A survey of 2050 nurses throughout Indonesia taken in April 2020 revealed a variety of stigma manifestations experienced by nurses. These included feelings of humiliation due to handling COVID-19 patients, threats of expulsion (even to nurses not directly involved in the treatment of COVID-19), local residents avoiding seeing nurses pass in front of their homes, avoiding nurses' families, and even refusing to allow a nurse's body to be buried in a nearby cemetery [22].
These troubling, discriminatory behaviors against nurses in Indonesia raise questions, given the prolonged course of the COVID-19 pandemic. To the best of our knowledge, investigations of stigma in the long-running pandemic period remain rare. In Indonesia, research on stigma toward nurses has focused mostly on the initial period of the pandemic [20, 21, 23-28]. Thus, it is necessary to add more knowledge about these experiences in a protracted crisis. Such research will increase the understanding of the burden created by stigma and will help policymakers and practitioners develop compre- hensive measures critical for reducing stigma. This study was intended to provide an understanding of how nurses in Indonesia describe the intensity of stigma in the prolonged COVID-19 pandemic.
2. MATERIALS AND METHODS
2.1. Design and Participants
This study is part of a research project titled “Exploration of Stigma Towards Nurses in Indonesia During the COVID-19 Pandemic,” conducted 1.5 years after the pandemic onset. The study used a qualitative descriptive approach to understand how people interpret, construct, and derive meaning from their world and experiences [29]. A semi-structured interview method was employed to gain insight into how nurses describe the intensity of stigma in the context of the prolonged COVID-19 pandemic in Indonesia.
To better picture the condition of Indonesia, the urban area of Jakarta province and the rural side of West Borneo province was chosen to gain richer data [30]. The purposive sampling method was used to recruit registered nurses actively working at healthcare facilities in the selected provinces who had experienced stigmatizing behavior during the pandemic. Invitations to participate were sent through various channels with the help of social media. To support the sampling process, a brief questionnaire was used to collect data related to socio-demographic information, work-related profiles, and stigma-related experiences. The sampling ended after theoretical saturation was reached [31].
Thirty-three (33) informants participated in this study. The average age of the participants was 32 years, with the youngest being 24 years old and the oldest 45 years old. Most participants were female (n=25; 76%), married (n=18; 55%) and worked at the secondary and tertiary healthcare levels (n=24; 73%). The number of participants working in urban areas (n = 16; 48%) and rural areas (n = 17; 52%) was nearly equal (Table 1).
| Participants | Age (Year) | Gender | Marital Status | Education Qualification in Nursing | Type of Healthcare Facility | Service Coverage | Experience as Nurse (year) |
|---|---|---|---|---|---|---|---|
| P1 | 24 | Female | Single | Diploma III | Secondary/Tertiary | Urban | 3 |
| P2 | 26 | Female | Single | Bachelor | Secondary/Tertiary | Urban | 3 |
| P3 | 25 | Male | Single | Bachelor | Secondary/Tertiary | Urban | 3 |
| P4 | 27 | Male | Single | Bachelor | Secondary/Tertiary | Urban | 3 |
| P5 | 42 | Female | Married | Bachelor | Primary | Rural | 20 |
| P6 | 27 | Female | Single | Bachelor | Primary | Urban | 4 |
| P7 | 41 | Female | Married | Bachelor | Secondary/Tertiary | Urban | 20 |
| P8 | 45 | Female | Married | Bachelor | Secondary/Tertiary | Urban | 21 |
| P9 | 27 | Female | Single | Magister | Secondary/Tertiary | Rural | 2 |
| P10 | 31 | Female | Married | Bachelor | Secondary/Tertiary | Urban | 7 |
| P11 | 33 | Female | Single | Bachelor | Secondary/Tertiary | Urban | 11 |
| P12 | 28 | Female | Married | Diploma III | Secondary/Tertiary | Rural | 7 |
| P13 | 36 | Female | Single | Bachelor | Secondary/Tertiary | Urban | 13 |
| P14 | 34 | Female | Married | Diploma III | Secondary/Tertiary | Rural | 9 |
| P15 | 24 | Female | Single | Bachelor | Secondary/Tertiary | Urban | 1 |
| P16 | 31 | Female | Single | Bachelor | Primary | Rural | 7 |
| P17 | 36 | Female | Married | Diploma III | Secondary/Tertiary | Rural | 13 |
| P18 | 45 | Female | Married | Diploma III | Secondary/Tertiary | Urban | 21 |
| P19 | 30 | Female | Married | Bachelor | Primary | Urban | 8 |
| P20 | 40 | Male | Married | Diploma III | Secondary/Tertiary | Rural | 21 |
| P21 | 29 | Female | Married | Diploma III | Primary | Rural | 2 |
| P22 | 29 | Female | Single | Bachelor | Secondary/Tertiary | Urban | 4 |
| P23 | 28 | Female | Single | Diploma III | Primary | Urban | 8 |
| P24 | 39 | Male | Single | Diploma III | Primary | Rural | 18 |
| P25 | 25 | Male | Married | Bachelor | Secondary/Tertiary | Rural | <1 year |
| P26 | 25 | Male | Single | Bachelor | Secondary/Tertiary | Rural | 2 |
| P27 | 36 | Female | Married | Diploma III | Secondary/Tertiary | Rural | 13 |
| P28 | 30 | Female | Married | Diploma III | Secondary/Tertiary | Rural | 6 |
| P29 | 34 | Male | Married | Diploma III | Secondary/Tertiary | Rural | 11 |
| P30 | 35 | Male | Married | Diploma III | Secondary/Tertiary | Rural | 13 |
| P31 | 37 | Female | Single | Diploma III | Secondary/Tertiary | Rural | 4 |
| P32 | 36 | Female | Married | Diploma III | Primary | Rural | 15 |
| P33 | 30 | Female | Married | Diploma III | Primary | Urban | 9 |
2.2. Data Collection
Semi-structured interviews in the Indonesian language were conducted from September 2021 to the initial week of January 2022. Before conducting the interviews, the questions were tested by two nurses who have backgrounds in West Borneo and Jakarta. At the beginning of the interview, the study objective and interview mechanism were re-introduced to the participants, followed by a casual conversation to enhance trust and rapport between the researcher and the participant. Furthermore, questions associated with the study objective were presented. Samples of the main open-ended questions were provided: “What are the stigmatizing attitudes and treatment you have experienced during this pandemic?”; “Are there any differences in these attitudes of treatment from the beginning of the pandemic until now, and if so, why?”. Researchers conducted the interviews in an exploratory manner. Probing on the answers given by the participants was addressed during the interview.
All interviews were conducted synchronously online [32] using the Zoom platform. The justification for using Zoom was due to the COVID-19 pandemic situation, which had limited face-to-face data collection. Using technology was helpful in capturing visual data. Nurses in both urban and rural areas also had familiarity with the necessary devices and internet connections, as well as familiarity with the Zoom platform [33]. Researchers conducted the interviews individually with each participant to ensure confidentiality and comfort. The average time of the interview was 60 minutes. After the interviews, participants were compensated for their internet usage.
All in-depth interview recordings with informants were transcribed. The transcribing process was carried out immediately after each interview. Three trained students helped with the process. Further steps of analysis only began after approvals of transcripts had been obtained through a member-checking process for participants. All the transcripts were in the Indonesian language.
2.3. Data Analysis
Researchers used a Framework Method approach to generate themes [34]. This method consists of seven steps of analysis. The analysis process began with a thorough reading of transcripts written in the original language to familiarize researchers with the data. Six transcripts that have the depth of phenomena being explored were selected for this step. The decision to determine which transcripts to read was made through discussion among researchers. The researchers then took notes and conducted coding procedures on these transcripts. All researchers contributed as the coders. The next steps were categorizing and developing an analytical framework. All the codes generated in the previous step were categorized and organized to an analytical framework, which was then applied to all datasets. After all datasets were coded, researchers created framework matrices, charted data into matrices, and developed themes. Finally, an interpretation memo was developed to conclude the findings. The researchers employed the traditional way of handling the data. The analysis process used paper, pen, and Microsoft Excel.
The trustworthiness of the study was maintained based on Korstjens and Moser [35], which includes credibility, transferability, dependability, confirmability, and reflexi- vity. Credibility was ensured by using multiple data sources from both urban and rural settings, as well as from nurses in different settings (i.e., primary and secondary/tertiary health settings). Member-checking was also conducted, where participants were asked to review the interview transcriptions. Transferability was addressed by providing clear context in the method, including who the participants were, when and where the data was collected, and how it was collected, allowing others to apply the results to their own setting. Purposive sampling was also used to support transferability. Dependability and confirmability were ensured with regular meetings among the researchers to discuss the data, the coding and theme compilation that were collaboratively conducted, and the member-checking process, which helped to increase objectivity and reduce subjective biases. Finally, all researchers were aware that their background in public health, nursing, and healthcare management might influence their positionality or the reflexivity process of the analysis. Therefore, to improve the validity and integrity of the data, the bracketing was carried out in the data collection phase.
2.4. Ethical Aspects
This study obtained ethical clearance from the local institutional review board (Reference number: 1090/SLKE-IM/UKKW/FKIK/KE/VII/2021). Prior to data collection, informed consent was obtained from all participants. Researchers also maintained confidentiality throughout the research process and reporting.
3. RESULTS
After analysis, three themes were generated. Descriptions and quotes from study participants were elaborated. The quotes were translated from the Indone- sian language to English.
3.1. Theme 1: The Dynamic of Stigma Intensity During a Prolonged COVID-19 Pandemic
Almost all participants agreed that the stigma towards nurses was strongly felt and experienced by nurses at the start of the COVID-19 pandemic. It then continued to decline gradually as the pandemic progressed. “During the early days of Covid, I was avoided by friends, family, and co-workers, but now I am not.”–P1, 24 years old.
A participant shared her fears at the beginning of the pandemic as she faced the reaction of neighbors, noting that the feeling subsided after a period. “Maybe at first it was scary when I was first asked to work in the COVID unit, it was a bit scary. When I came back home, I was like, oh my God, I'm afraid of neighbors. But the more the time passed by, it seems that people are getting used to it too”–P2, 26 years old.
Another participant also mentioned that avoidance from co-workers was reduced after the pandemic had lasted for some time. “(In the beginning) they were more afraid. When we walked down to the area of management (hospital), it must be like ‘Ugh, stay away, don't come near you guys to this room’. Why did they do so? I'm in the ICU, not in the COVID room. They seemed to generalize. I think now it's okay, it's normal”–P16, 31 years old.
The stigma manifestations associated with this pattern were primarily behaviors linked to the threat of COVID-19. Many participants felt shunned, avoided, rejected, fearful and worried in this period as compared to later periods.
Although participants generally reported a decline in stigma intensity over the course of the pandemic, stigma had not completely disappeared by the end of 2021, when the study was conducted. Stigma was still experienced on some occasions, although not as strongly as before.
When the incidence increased, demeaning words from patients and their families were often experienced due to unmet expectations regarding the quality of services provided by nurses. “In the second wave, (…) the hospital was full, and we couldn’t accept patients. I was treated badly at that time, with several patients with stigma they brought to us. That was a month ago that I experienced. We were crammed with patients, and the oxygen supply was low. So, we said, ‘Madam, we were out of oxygen, and the facility and staff were both completely occupied. Please visit a different hospital.’ Immediately they said, ‘Eh, you're a nurse, huh! You were sworn in to do this and serve. Then you?!’ She said to me, ‘You know, I could pay your wages for an entire year!’ It was very disparaging to me. She said, ‘I could pay your salary and bonuses directly for a year. If that is how you serve, you won't enter heaven’–P15, 24 years old.
As the incidence of COVID-19 decreased, some participants felt more vulnerable to stigma. In this context, they felt that society viewed them as a major source of COVID-19 transmission compared to the general population. One participant revealed that the decreasing number of new COVID-19 cases caused people around her to accuse her of transmitting COVID-19 to family members, even though transmission may have had an unrelated source.“Around November, my family and I got COVID-19. We had seven people in our house, and all of us got it. (…) Since I am a health worker, I took an isolation period in the hospital. At that time, the case was going down when we were hit. The response from the neighbors was not nice. When I arrived home, the rumors were like I brought it to my family.”–P2, 26 years old.
Another form of stigma revolved around the issue of health workers making profits during the COVID-19 period. Some believed that health workers were faking COVID-19 test results in order to gain benefits from the COVID-19-related funding. When new cases had already declined, nurses’ requests to carry out COVID-19 screening procedures at health facilities were suspected of fraud. “In August or September, while the number of cases was declining, we continued to operate a polyclinic for acute respiratory illnesses. There, a PCR swab must be performed on a patient who has had symptoms for a week. However, there was a patient refusing to be PCR-tested (for Coronavirus). “I don’t want to undertake it because currently, there are fewer COVID cases. Why must I perform PCR? There’s no such thing as Covid. I don’t want it to be positive when it is tested by PCR. All of you, health workers, you are all to make the result positive for COVID.”–P22, 29 years old.
3.2. Theme 2: Nurses’ Points of Reference when Elucidating the Intensity of Stigma
Participants often explained the intensity of stigma they experienced during the prolonged pandemic by taking into account both the frequency of stigmatizing behaviors and the intensity of emotions they felt about it. The most frequently mentioned behaviors used to describe this intensity were avoidance behaviors from family members, friends, and colleagues in healthcare facilities. Other points of reference they used included the frequency and emotions associated with nurses’ expulsion from their residences, rumors and accusations of nurses being the main source of COVID-19 transmission or falsifying COVID-19 test results for financial gain, and how often they observed patients or individuals still hiding when being visited. Participants also discussed the intensity of stigma when non-COVID clients questioned them during service about whether they were nurses who also handle COVID-19 and when clients used negative labeling towards them.
In addition to the behaviors mentioned above, the intensity of stigma throughout the pandemic was also associated with the extent to which participants felt negative about their level of acceptance in their residential community. It was often found that participants felt the stigma had subsided when they were no longer afraid to go home, be expelled, or be asked to move. In other words, the intensity of the stigma decreases when they feel safe living close to the community.
Following these expressions, researchers attempted to structure the point of references nurses repeatedly used to evaluate the intensity of stigma in a protracted pandemic;
(a) The frequency of avoidance behavior.
(b) The frequency of expulsion from their home/ residence.
(c) The frequency of witnessing people being suspi-cious or accusing them of faking COVID-19 test results.
(d) The frequency of hearing negative rumors about themselves/their profession.
(e) The frequency of meeting clients who are suspicious or worried if they are nurses who handle COVID-19.
(f) The frequency of verbal conflicts that demean nurses occurs in health services.
(g) The intensity of fear or anxiety regarding each of the above situations.
3.3. Theme 3: The Perceived Contributing Factors to the Stigma Intensity in the Protracted Pandemic
Several factors influenced the intensity of stigma against nurses during the pandemic (Fig. 1). These included aspects related to communication, the image of nurses, burden distribution, fatigue and familiarity with the pandemic, inability to meet community needs, and incentive policies.
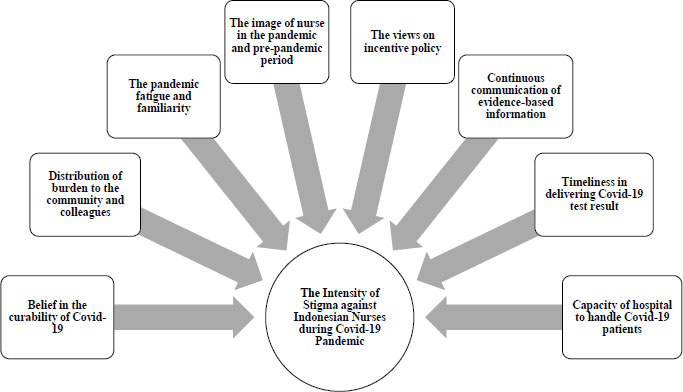 |
Fig. (1). Factors influencing stigma intensity towards nurses during the prolonged COVID-19 pandemic. |
3.3.1. Continuous Communication of Evidence-based Information
As the COVID-19 pandemic continued, participants mentioned that people were exposed to more information, leading to increased knowledge and less stigma to health workers. However, false information circulating during the pandemic and the inability to assess accurate information still encouraged stigma towards nurses. Continuous communication of evidence-based information plays an important role in reducing the intensity of stigma, including within the scope of health workers. One participant noted that fear of coming into contact with equipment provided by the nurse on duty in the COVID-19 zone had decreased after health staff knew the scientific findings that transmission through fomites was proven to be very low. “Initially, it was because we did not know what the course of the disease was like, nor what the risk of transmission was. As a result, we nurses kept our distance from each other, even for small things like patient reports. We could no longer use paper. They always reminded us that if we wanted to admit a patient, we did not need to bring the paper but simply take a photo of it. This included lab and ECG results. However, now everything has changed as we know the risk of transmission is only a fraction of a percent for these things.”–P13, 36 years old.
3.3.2. Belief that COVID-19 can be Cured
The belief in the curability of COVID-19 was seen as a factor contributing to the reduction of stigma. The fact that COVID-19 could be cured brought hope and a higher sense of community dependence on health workers. Consequently, participants were increasingly sought after and not avoided as much as before. “What we have now is not as bad as last year. Although there are still some who do not want to be visited, people are relatively more welcoming now because they also know that COVID-19 can now be cured. […] They know that health workers can help by prescribing medicine.”–P5, 42 years old. A participant added that successful handling of cases leading to recovery also had a positive effect on stigma intensity towards them. This was said to have increased people's trust in the approach and information given by health workers.
3.3.3. Distribution of Burden to the Community and Colleagues
Participants in the study noted that the declining stigma towards nurses may have been due to the shared burden felt by both nurses and the community. At the beginning of the pandemic, there was a perception that healthcare workers were most at risk. However, as more cases emerged, the community began to feel the burden and risks were shared. The shared burden also changed the negative perception of people in the workplace, especially those handling COVID-19 cases. As COVID-19 cases began to appear in non-COVID-19 units, the burden started to be distributed to other units in the health facility. This likely increased empathy and reduced the stigmatizing behaviors of colleagues toward nurses who worked with COVID-19 patients. “It was like that in the beginning. Now that there have been many cases, many patients don't admit that they have COVID-19. After a long time, my friend admitted that, in the end, they were also caught in the green zone. So, in the end, they felt for themselves that caring for those with COVID-19 is actually not that bad. And, their friends in the red zone are also still healthy. So, yes, now it's not anymore.”–P2, 26 years old.
3.3.4. The Pandemic Fatigue and Familiarity
Fatigue and familiarity with the pandemic were seen to reduce the stigma against them during a prolonged pandemic. Participants saw pandemic fatigue as a rejection of the reality of the pandemic. As cases continued to increase during the long pandemic period, they saw some people became bored and tired of the rules and their application, leading to an indifferent attitude towards the pandemic. In contrast, pandemic familiarity was seen by participants as an acceptance of the reality of the pandemic. Participants saw that the addition of cases over time had encouraged acceptance of the pandemic, and the rules were seen as a new culture that provided a sense of security. Familiarity was also encouraged as more and more people were affected. This helped more people understand the burden of stigma. Therefore, people no longer viewed COVID-19 as something extraordinary. For some participants, familiarity with the pandemic led to a feeling of indifference or neglect towards unpleasant treatment from others. “These past 2 years have been really hard for nurses and other health workers who care for and treat COVID-19 patients. However, as time passes and we enter the middle of 2021, people are becoming more accustomed to it, so it's not as difficult as it used to be. The first time was tough because it was the first time. I am one of those who experienced exclusion.”–P27, 36 years old.
3.3.5. The Image of Nurse in the Pandemic and Pre-pandemic Period
During the pandemic, the public's increased level of empathy towards nurses who worked as part of humanitarian efforts was likely playing a role in decreasing the stigma against them. Increased support in the form of moral and material aid was seen as a sign of the fading of stigma. On the other hand, the long-standing negative image of nurses in the pre-pandemic period seemed to encourage stigma towards nurses during the pandemic. Participants shared that prior to the pandemic, nurses were often seen as only doctors' assistants in the public eye. This encouraged more different treatment towards nurses from patients and their families during the pandemic. “People trust doctors more than nurses. (...) thus, families were more aggressive when they were with nurses, while with doctors, they were more receptive. So, with doctors, they spoke more politely because they saw that doctors have higher education, are smarter, so more appreciated”– P2, 26 years old. In summary, the public's perception of nurses has changed during the pandemic. While there has been an increase in public empathy towards nurses, the pre-existing negative image of nurses has contributed to stigma during the pandemic.
3.3.6. The Views on Incentive Policy
Financial incentives for healthcare workers during the pandemic had both positive and negative impacts on stigma. Some participants believed that the incentives decreased stigma among nurses by increasing their involvement in COVID-19 handling, leading to greater understanding among colleagues. However, interest in incentives also caused jealousy among those not involved, resulting in unpleasant and stigmatizing remarks among health workers. “Yes, until now, sometimes they would say, “Wow, it is good working in the isolation room. More money. More successful.”–P31, 37 years old. Additionally, in the community, the incentives led to suspicions that nurses would falsify test results for financial gain.
3.3.7. Timeliness in Delivering COVID-19 Test Results
During the pandemic, participants reported that delays in delivering COVID-19 test results were frequent, particularly during the initial period. Some even mentioned that test results were submitted after the patient had passed away. This delay had increased the intensity of stigma towards health workers, including nurses. The delay created a sense of distrust and suspicion of the integrity of health workers, with some believing that the motive behind the delay was financial gain. “In the past, it took time for the results of COVID-19 tests to come out, sometimes up to 24 hours or 6 hours. There was a patient who died before getting the test result, but their symptoms already indicated that they had COVID-19. Although the swab results were negative, the patient passed away and we had to bury them as a COVID-19 patient based on their signs and symptoms. The family had objected to this change from a negative result and felt that the result was made positive by us. Nowadays, the situation is safer.”–P11, 33 years old.
3.3.8. Capacity of Hospital to Handle COVID-19 Patients
Every time the number of new cases escalated, limited bed capacity and the number of hospitals caused some participants to reject patients seeking help. This rejection during the crisis had become a gateway for the emergence of stigmatized behavior experienced by nurses in healthcare. “At that time, there was a shortage of oxygen. Family members urged the hospital to meet their oxygen needs. Meanwhile, there was an overall oxygen crisis in Indonesia. This was the time when we, as nurses, were verbally abused, talked about, and gossiped about with negative comments.” –P25, 25 years old.
4. DISCUSSION
During the initial period of the COVID-19 pandemic in Indonesia, nurses strongly felt the experience of stigma. Many of these primarily manifested in forms of avoidance and eviction. Brewis, Wutich, and Mahdavi noted that COVID-19 could create a strong stigma, like other infectious diseases, due to these three characteristics: infectiousness, potential fatality, and lack of treatment associated with the disease [36]. These characteristics made COVID-19, in its early days, a serious threat. Referring to the six dimensions of stigma articulated by Jones et al. [37], this would mean that COVID-19, early in its appearance, had a high peril dimension, which intensified the people’s fear and reactions toward affected people and those handling COVID-19.
However, unlike some other infectious diseases which over time could trigger fear reactions, this study demonstrated that the dimension of peril in COVID-19 did not persist throughout the pandemic. Nurses perceived that extreme stigmatization—in the form of expulsion and blatant avoidance, for example—continued to decline towards the end of 2021 (when the data collection was conducted). This gradual decrease in stigma towards nurses is somewhat different from the stigma associated with other respiratory-related infectious diseases such as MERS. After the emergence of MERS cases, stigma is still shown to be a burden for years [6, 7]. This could be explained following the dimension of peril in MERS. Since 2012, the nature of MERS has been known as a life-threatening infectious disease without specific vaccines and treatments [38]. Meanwhile, with COVID-19, pre- ventive measures such as the use of personal protective equipment have been easy to implement and have felt effective, especially heading into 2021. The number of people who healed or had mild cases grew and a therapeutic regimen was proven effective in increasing the recovery rate, which made the threat of COVID-19 no longer as strong as it had appeared at the beginning. Moreover, 35 percent of MERS cases are reported to end in death [38], far exceeding COVID-19’s average global fatality rate of around 5 percent [39]. With MERS, the risk of experiencing stigma also seems to impact more health workers. Human-to-human transmission of MERS predominantly occurs in the healthcare setting [38]. In contrast, there is no data showing that COVID-19 was mostly transmitted in a healthcare setting or by healthcare workers.
A comparison with tuberculosis (TB), another respiratory infectious disease, may also shed light on the progressive decline of the COVID-19 stigma against nurses. TB is a common respiratory disease, first emerging in the 1700’s. TB cure methods have existed for a long time. The first successful remedy for TB was described in 1854, and after decades following Koch’s success to isolate the tubercle bacillus around 1880, many advances in anti-tuberculous drugs were developed. Nonetheless, it was noted that TB-related stigma continued to impact affected individuals until now [40]. Characteristics of the populations most impacted by TB were explained to influence this prolonged stigma phenomenon. Stigma is known to be strengthened when a disease is associated with a marginalized, historically powerless, or socially undervalued group [36]. Unlike COVID-19, which affected almost all social segments of the population, TB is often associated with poverty or lower social classes [41].
Although nurses generally experienced a gradual decrease in stigma behaviors, some forms of stigma continued to be felt throughout the COVID-19 trajectory. At times of increasing new cases, some nurses experienced more stigma related to their professionalism, for example, when their job as nurses was insulted because they could not immediately meet the client’s needs. High numbers of new cases could lead to extreme anxiety among the wider community, resulting in heightened expectations of nurses. When nurses were unable to meet these expectations, stigma towards them increased. This research shows that clients’ disappointment will lead to expressions of disbelief in nurses’ abilities and negative labels against them. Other studies also confirmed that COVID-19 has indeed become a vehicle for more stigmatizing attitudes against nurses [42, 43].
On the other hand, during the decline in new cases, nurses experienced vulnerability to being blamed first if someone around them contracted COVID-19. Nurses also felt more vulnerable to accusations of falsifying COVID-19 test results because, in periods of low cases, people were more likely to distrust positive COVID-19 test results. As revealed by previous epidemics, a decrease in cases does not always mean the disappearance of stigma [44]. Stigma can remain and be even more focused on groups considered more at risk. Categorization may create the impression of a separation between the “general public” and “vulnerable groups,” contributing to the existence of an “in-group” and “out-group,” which also leads to the formation of stigma [45].
According to the participants, there is a likelihood that familiarity and fatigue with the pandemic would influence social acceptance and affect people's perceptions of the phenomenon. Both those who accept the pandemic as a new reality and those who are unconcerned may result in fewer nurses experiencing forms of stigma. A future quantitative study is needed to determine whether public pandemic familiarity and fatigue really have a significant effect in reducing stigma toward healthcare workers during a pandemic. As far as the researcher’s efforts in literature review, there has been no research that specifically discusses this.
At the community level, communication of scientific evidence both to the public and healthcare workers has been valuable in preventing stigma. Therefore, ensuring continuous and accessible scientific information for both groups would be helpful in addressing stigma during a prolonged pandemic. Proper health education about scientific evidence will prevent the stigmatization of healthcare workers [16]. In addition to scientific evidence, providing sufficient information about the policy regarding financial incentives for healthcare workers would also be beneficial in the context of Indonesia to prevent the development of suspicion. The benefits of reducing false information in the community would not only be experienced by healthcare workers but also by programs targeting the community at large to control pandemics that are carried out by them [46].
Furthermore, another important thing is to increase trust in the healthcare workers. Shaping a positive image of Indonesian nurses must be supported in the long run, beyond the pandemic period. This is because nurses in Indonesia have long experienced inferiority and confused their professionalism compared to their closest members in the care team, namely doctors. The labels “doctor's maid” or “doctor’s assistant” have been used to refer to nurses due to historical reasons and media portrayal [47, 48]. Universities as institutions that create nurses, healthcare organizations, and media could be empowered for this purpose.
According to the findings, seeking ways to establish a fast and accurate COVID-19 diagnosis, as well as ensuring adequate capacity in health facilities at the onset of cases and when the cases are increasing, are also crucial. Timeliness in delivering results and having sufficient capacity would increase the possibility that everyone receives accurate information and prompt services. This would lower suspicion and enhance community satisfaction towards nurses as frontliners.
In this study, participating nurses repeatedly used the experiences of stigma as avoidance, rejection, suspicion, negative rumors, and disparaging remarks about the nursing profession to evaluate the stigma intensity, leading to the need to underline these in stigma prevention. Efforts to build a sense of security and trust with nurses during the pandemic are desperately required [16]. This is critical due to the escalated mental health consequences that they could experience in this period, as also observed in other epidemics and pandemics in the past [49]. It is also important to prevent conflicts between nurses and patients or patients' families during the pandemic. Studies have shown that healthcare professionals are more susceptible to stigmatization by the community and to face workplace conflicts [50]. Conflicts can open the door to stigmatizing behaviors, where demeaning words or labels occur [16].
When assessing the magnitude of stigma in protracted crises, nurses often relied on their emotional responses to stigma experiences. This implies that alongside examining the frequency of stigma manifestations, evaluating the intensity of emotions must also be taken into account in stigma assessments as it can impact nurses' self-assessment. Based on the findings of this study, researchers have compiled a set of potential questions (Table 2) that could be utilized to assess subsequent stigma intensity associated with the pandemic or similar extraordinary events in the future.
4.1. Implications and Limitations
To the best of the researcher’s knowledge, the nature of this study, which discusses stigma in the long term fills a gap of many previous stigma studies. This study suggests that future programs and policies aimed at preventing stigma towards Indonesian nurses in extraordinary events like the pandemic must consider the prolonged nature of stigma. Such efforts to anticipate and reduce stigma towards nurses should be made at the onset of the outbreak and continue along the trajectory of an epidemic. Attention should be given to avoid more complexity in disease control efforts during the challenging situation, because nurses play a critical role as frontliners. Factors contributing to stigma intensity listed in this study can be used in the development of strategies for anti-stigma intervention in the future.
| List of Questions: |
|---|
| 1. How often do nurses feel they are being avoided (both verbally and non-verbally)? 2. How often do nurses experience expulsion from their home/residence? 3. How often do nurses experience suspicion or accusations of faking [name of disease] test results? 4. How often do nurses hear negative rumors about themselves/their profession? 5. How often do nurses meet clients who are suspicious or worry about whether they are handling [name of disease]? 6. How often do verbal conflicts that demean nurses occur in health services? 7. To what extent do feelings of fear or anxiety about the above situations exist among nurses? |
The possible weakness of this research is that data collection (i.e., interview) was performed online, which might have reduced the openness and comfort of participants to some degree even though researchers had performed ways to establish confidentiality, trust, and comfort throughout the study. In addition, the transferability of the findings to other settings may be limited to places that have similarities with the sociodemographic and cultural profile of Indonesia. Indonesia itself has a multiethnic and multireligious society and is considered to be in the low-socioeconomic country group at the time this study was conducted.
CONCLUSION
Stigma against nurses during the COVID-19 pandemic was stronger at the beginning of the pandemic, which is similar to the stigma observed during previous emerging infectious disease outbreaks. However, over the course of the pandemic, the degree of stigma gradually decreased. This is likely due to the perceived reduction in risk and fatality, as well as increasing awareness that anyone can transmit COVID-19 regardless of their social status. Nonetheless, some forms of stigma continued to occur regardless of the number of cases during the pandemic, albeit less intensely than before, in the workplace and in community settings. The intensity of stigma towards nurses during the prolonged pandemic was driven by several factors, including pandemic fatigue and familiarity, evidence-based communication, the curability of COVID-19, different views on nurses' image and incentive policy, burden distribution, and the adequacy of facilities. These contributing factors could be taken into account in the development of programs and policies to tackle pandemic-related stigma. Further research could examine the association or causation between these factors and stigma through quantitative studies. The proposed questions could also be used to investigate stigma in the current situation or in future health crises.
LIST OF ABBREVIATIONS
| MERS-CoV | = Middle East Respiratory Syndrome Coronavirus |
| TB | = Tuberculosis |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study obtained ethical clearance from the Faculty of Medicine and Health Sciences ethical committee at Krida Wacana Christian University, West Jakarta, Indonesia (Reference number: 1090/SLKE-IM/UKKW/ FKIK/KE/VII/2021).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
COREQ guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions.
FUNDING
The study was funded by Krida Wacana Christian University, Awards/Grant number: 07/UKKW/LPPM-FKIK/LIT/VI/2021.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank all the participants in this research, who, amidst their busy schedules during the COVID-19 pandemic, still gave themselves to participate. We also thank Agatha Tunjung Dwivania, Faustina Kewa Wara, and Masaaro Laia for their support.
REFERENCES
| [1] | Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol 2001; 27(1): 363-85. |
| [2] | Van Brakel WH. Measuring health-related stigma—A literature review. Psychol Health Med 2006; 11(3): 307-34. |
| [3] | Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: Adding moral experience to stigma theory. Soc Sci Med 2007; 64(7): 1524-35. |
| [4] | Heijnders M, Van Der Meij S. The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychol Health Med 2006; 11(3): 353-63. |
| [5] | Park JS, Lee EH, Park NR, Choi YH. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Arch Psychiatr Nurs 2018; 32(1): 2-6. |
| [6] | Ahn SH, Kim JL, Lee SH, Park HY, Lee JJ, Lee H. Associations of health-related quality of life with depression and stigma in MERS-CoV survivors during the recovery period. Med 2022; 101(25): 29440. |
| [7] | Farag E, nour M, Marufu O, et al. The hidden epidemic: MERS-CoV-related stigma observations from the field, Qatar 2012-2015. Int J Infect Dis 2016; 45: 332. |
| [8] | Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013; 103(5): 813-21. |
| [9] | Saeed F, Mihan R, Mousavi SZ, et al. A narrative review of stigma related to infectious disease outbreaks: what can be learned in the face of the COVID-19 pandemic? Front Psychiatry 2020; 11(December): 565919. |
| [10] | Fischer LS, Mansergh G, Lynch J, Santibanez S. Addressing disease-related stigma during infectious disease outbreaks. Disaster Med Public Health Prep 2019; 13(5-6): 989-94. |
| [11] | Yuan K, Huang XL, Yan W, et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: A call to action. Mol Psychiatry 2022; 27(1): 19-33. |
| [12] | Santibañez S, Polgreen PM, Beekmann SE, Rupp ME, Del Rio C. Infectious disease physicians’ perceptions about ebola preparedness early in the us response: A qualitative analysis and lessons for the future. Health Secur 2016; 14(5): 345-50. |
| [13] | WHO. Attacks on health care in the context of COVID-19. 2020. Available from : https://www.who.int/news-room/feature-stories/detail/attacks-on-health-care-in-the-context-of-COVID-19 |
| [14] | Dye TD, Alcantara L, Siddiqi S, et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: An analytical cross-sectional global study. BMJ Open 2020; 10(12): e046620. |
| [15] | Faris M, Arifianto MR. Social Stigma toward health workers associated with Coronavirus Disease 2019. Open Access Maced J Med Sci 2020; 8(T1): 112-4. |
| [16] | Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis 2020; 20(7): 782. |
| [17] | Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability 2020; 12(9): 3834. |
| [18] | Mostafa A, Sabry W, Mostafa NS. COVID-19-related stigmatization among a sample of Egyptian healthcare workers. PLoS One 2020; 15(12): e0244172. |
| [19] | Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front public Heal 2021; 8: 1-11. |
| [20] | Manik MJ, Natalia S. Social stigma towards nurses taking care of patients with COVID-19 in Indonesia: A mixed-methods study. Belitung Nurs J 2021; 7(2): 98-106. |
| [21] | Yufika A, Pratama R, Anwar S, et al. Stigma against COVID-19 among health care workers in Indonesia. Disaster Med Public Health Prep 2022; 16(5): 1942-6. |
| [22] | FIK UI. Penolakan pemakaman perawat garda depan COVID-19 potret stigma sosial memilukan. 2021. Available from : https://nursing.ui.ac.id/penolakan-pemakaman-perawat-garda-depan-COVID-19-potret-stigma-sosial-memilukan/ |
| [23] | Janitra FE, Melastuti E, Yusuf A, Fadhilah H, Wibawa YA, Padjadjaran JK. Perceived stigma, psychological response, and nurse coping in the COVID-19 pandemic in indonesia. J Keperawatan Padjadjaran 2021; 9(1): 10-7. |
| [24] | Istianti DW, Wirata RB. Pengalaman perawat tentang stigma COVID-19 pada profesi perawat. J Kesehatan 2022; 9(2): 102-18. |
| [25] | Winugroho T, Budiarto A, Hidayat A. Pengaruh stigmatisasi sosial terhadap koping stress perawat dalam penanganan COVID-19 di rumah sakit dr. soedjono magelang. NERS J Keperawatan 2021; 17(2): 81. |
| [26] | Aprianti A, Laksana P, Anggraini FDP. Stigma masyarakat indonesia pada pasien dan tenaga kesehatan COVID-19 berdasarkan teori health belief model. J Kesehat Masy Andalas 2021; 15(2): 15-21. |
| [27] | Gafur A, Zainuddin Z, Musdalifah M, Darmansyah S. COVID-19 & Stigma of patient families and health workers in makassar city, Indonesia. Al-Sihah: The PubHea Sci J 2021; 13(1): 88. |
| [28] | Peratiwi I, Friska H, Subratha A. Studi kualitatif stigma negatif terhadap tenaga kesehatan yang terkena COVID-19. J Ilmu Kesehat 2021; 5(1): 38-42. |
| [29] | Doyle L, McCabe C, Keogh B, Brady A, McCann M. An overview of the qualitative descriptive design within nursing research. J Res Nurs 2020; 25(5): 443-55. |
| [30] | Head of central bureau of statistics regulation no. 120 of 2020 concerning classification of villages, urban and rural areas in Indonesia. 2020; 1-430. |
| [31] | Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018; 18(1): 148. |
| [32] | Salmons J. Designing and conducting research with online interviews. Cases in Online Interview Research 2011; 1-30. |
| [33] | Datareportal. Digital 2021. Available from : https://datareportal.com/reports/digital-2021-indonesia |
| [34] | Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13(1): 117. |
| [35] | Korstjens I, Moser A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract 2018; 24(1): 120-4. |
| [36] | Brewis A, Wutich A, Mahdavi P. Stigma, pandemics, and human biology: Looking back, looking forward. Am J Hum Biol 2020; 32(5): e23480. |
| [37] | Jones EE, Farina A, Hastorf A. Social stigma: The psychology of marked relationships 1984. |
| [38] | WHO. Middle East respiratory syndrome coronavirus 2022. Available from : https://www.who.int/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov) |
| [39] | WHO. Coronavirus disease (COVID-19) pandemic 2022. Available from : https://www.who.int/emergencies/diseases/novel-coronavirus-2019 |
| [40] | Meghji J, Gregorius S, Madan J, et al. The long term effect of pulmonary tuberculosis on income and employment in a low income, urban setting. Thorax 2021; 76(4): 387-95. |
| [41] | Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Rep 2010; 125(4): 34-42. |
| [42] | Bhatti OA, Rauf H, Aziz N, Martins RS, Khan JA. Violence against healthcare workers during the COVID-19 pandemic: A review of incidents from a lower-middle-income country. Annals of Global Health 2021; 1-11. |
| [43] | Byon HD, Sagherian K, Kim Y, Lipscomb J, Crandall M, Steege L. Nurses’ experience with type II workplace violence and underreporting during the COVID-19 pandemic. Workplace Health Saf 2021; 70(9): 21650799211031233. |
| [44] | Peprah P, Gyasi RM. Stigma and COVID‐19 crisis: A wake‐up call. Int J Health Plann Manage 2021; 36(1): 215-8. |
| [45] | Mawar N, Saha S, Pandit A, Mahajan U. The third phase of HIV pandemic: Social consequences of HIV/AIDS stigma & discrimination & future needs. Indian J Med Res 2005; 122(6): 471-84. |
| [46] | Peshkovskaya A, Galkin S. Health behavior in Russia during the COVID-19 pandemic. Front Public Health 2023; 11(October): 1276291. |
| [47] | Romana A, Kedang S, Rindu Y, Roku R. Textbook of basic nursing concepts 2023; 1-404. |
| [48] | Fahriati AP. Description of public perception of the nursing profession in the Banangan sub-district area 2015. |
| [49] | Wasim A, Truong J, Bakshi S, Majid U. A systematic review of fear, stigma, and mental health outcomes of pandemics. J Ment Health 2023; 32(5): 920-34. |
| [50] | Saragih ID, Tarihoran DETAU, Rasool A, Saragih IS, Tzeng HM, Lin CJ. Global prevalence of stigmatization and violence against healthcare workers during the COVID ‐19 pandemic: A systematic review and meta‐analysis. J Nurs Scholarsh 2022; 54(6): 762-71. |









