All published articles of this journal are available on ScienceDirect.
Factors Affecting Student Nurses’ Adherence to Standard Precautions for Preventing Tuberculosis and HIV at Eswatini University
Abstract
Background
The prevention of Healthcare-associated Infections (HAIs) has become an increasing challenge throughout the world. Tuberculosis (TB) and Human Immunodeficiency Virus (HIV) are among the infections that student nurses are at risk of acquiring during their clinical practice in the healthcare setting. One of the most essential measures used to control HAIs is the application of standard precautions. However, student nurses have been found to not adhere to the standard precautions for the prevention of TB and HIV when allocated for clinical practice in the Eswatini healthcare setting.
Methods
A non-experimental quantitative approach was used to conduct a survey on senior student nurses of Eswatini University using the questionnaires. The total population of third-, fourth-, and fifth-year students was selected through the census sampling method. Statistical Package for Social Science version 26 software was used to analyze the data.
Results
Factors influencing compliance with standard precautions for the prevention of TB and HIV have been categorized into the availability of resources, measures taken by student nurses, hospital support role, and university support role.
Conclusion
The researchers recommend that TB and HIV prevention skills be demonstrated to student nurses in the skills laboratory and that clinical facilitators should accompany students in the clinical area. In the hospitals, ordering and monitoring of supplies should be done well to eliminate the shortage of resources, and preceptors should be exempted from other duties so that they can be able to supervise student nurses.
1. INTRODUCTION
Hospital-acquired Infections (HAI) are opportunistic infections that are typically not present at the time of admission, but are usually acquired after hospitalization and manifest 48 hours after admission to the hospital [1]. HAIs are a leading risk factor for patients, healthcare workers, and students with respect to morbidity and mortality in healthcare environments [2]. It is estimated that HAIs affect 5% to 10% of hospitalized patients [3]. Among these infections, Tuberculosis (TB) and Human Immunodeficiency Virus (HIV) can also be accidentally transmitted from one person to another in the clinical setting. Globally, 38.4 million people were living with HIV in 2021, and in 2020, an estimated 10 million people had TB worldwide [4, 5]. One of the most essential measures used to control these infections is the application of standard precautions. Standard precautions are strategies used to prevent the spread of micro-organisms in healthcare settings regardless of the patient’s diagnosis or presumed infection status [6].
Healthcare workers, including student nurses, should adhere to standard precautions to protect themselves and their patients from infections. As previous studies have alluded, the objectives of standard precautions are designed to protect healthcare workers from acquiring occupational infections and reduce and prevent transmission of infections [7]. There is a possibility of microorganisms being transferred from one patient to another through the healthcare workers as well as healthcare workers infecting themselves. Student nurses are among the healthcare workers who do not comply with standard precautions as they should for the prevention of TB and HIV [8].
Educational institutions always organize clinical place- ment for student nurses as an essential part of nursing education [9]. It is in this encounter that student nurses get a chance to put the theory they have learned in class into practice. However, different studies globally reveal that a considerable percentage of students lack knowledge and skills regarding the prevention of exposure to infections and diseases while in training [10, 11]. Student nurses in Eswatini, just like the rest of the world, are also exposed to TB and HIV daily during practice in the Clinical Learning Environment (CLE). In addition, Eswatini has the highest prevalence of TB (1382 cases per 100,000 population) and HIV, accounting for 31% among adults aged 18-49 years in the world [12]. This puts the lives of the students and the patients they are caring for at risk of cross-infection in the hospital setting. Previous studies show that healthcare workers adopt standard precautions depending on their perception of the risk of contracting the infectious disease in each clinical situation [13]. It is for this reason that compliance with standard precautions of student nurses can be low as they may not always correctly judge the situations that call for the application of protective measures. Therefore, a study to assess the factors affecting student nurses’ adherence to standard precautions for preventing tuberculosis and HIV at Eswatini University was warranted.
2. MATERIALS AND METHODS
2.1. Study Design and Setting
A non-experimental quantitative approach was used to assess factors affecting student nurses’ adherence to standard precautions for preventing tuberculosis and HIV. The study took place at the University of Eswatini, Faculty of Health Sciences, found in the nation’s capital Mbabane in the Hhohho region of Eswatini.
2.2. Participants
Study participants were student nurses who were in years 3, 4, and 5 because they had experience working in the clinical attachments. A census sampling method was applied and this sampling method was ideal because the population of interest was small. The total number of student nurses in years three, four, and five during the period when this study was done was 144. All of these student nurses comprised the sample size for our study; however, 105 students provided their consent to participate and filled out questionnaires completely. The inclusion criteria were both male and female student nurses in years three, four, and five, and all students who consented to be a part of the study. Student nurses who did not provide consent to be a part of the study and those who were absent from university during the period of data collection were excluded.
2.3. Data Collection
This study was approved by the Eswatini Health and Human Research Review Board and the University of Pretoria’s ethics committee. The research instrument used in this study was self-administered questionnaires. The researchers chose questionnaires because they are less costly, they offer the possibility of complete anonymity, and the absence of an interviewer ensures no interviewer bias. The researchers after acquiring permission from the authorities of the university hand-delivered the question- naires to students. Each questionnaire had a consent form attached to it for students to read and sign before completing the questionnaire. Students were asked to return the completed questionnaires to their class representatives in the absence of the researchers to ascertain anonymity. The researchers collected the questionnaires after a week from the day they were distributed.
2.4. Data Analysis
Collected data were entered into Microsoft Excel and the Statistical Package for Social Sciences (SPSS) software version 26 was used to analyze the data. Graphs, tables, and percentage distribution were used to analyze and present the demographics, as well as the different questions in the questionnaire. Respondents’ self-report questionnaires were used to identify factors influencing adherence to standard precautions. A statistician was also involved during the data analysis process.
3. RESULTS
3.1. Demographics of the Participants
As tabulated in Table 1, 62.9% (n=66) of the participants were female students while 37.1% (n=39) were male students. The majority (n=40) of the participants were between ages 20-24 years. The lowest number of students, accounting for 2.9% (n=3) per group, were between the ages 40- 44 years and 44- 49 years. The median age was 28 years and the standard deviation was 6.761. Regarding marital status, most of the participants 70.5% (n=74) were single, while 29.5% (n=31) were married. Out of 105 students who responded, 27.6% (n=29) of the students were in the 3rd year, 54.3% (n=57) were in the 4th year, and 18.1% (n=19) were in the 5th year.
| Variables | Respondents (N) | Percentage (%) |
|---|---|---|
| Gender | - | - |
| Male | 39 | 37.1 |
| Female | 66 | 62.9 |
| Age group | - | - |
| 20 – 24 years | 40 | 38.1 |
| 25 – 29 years | 17 | 16.2 |
| 30 – 34 years | 21 | 20 |
| 35 – 39 years | 20 | 19 |
| 40 – 44 years | 3 | 2.9 |
| 45 and above | 3 | 2.9 |
| Not stated | 1 | 1 |
| Marital status | - | - |
| Married | 31 | 29.5 |
| Single | 74 | 70.5 |
| Level of study | - | - |
| 3rd year | 29 | 27.6 |
| 4th year | 57 | 54.3 |
| 5th year | 19 | 18.1 |
| Total | 105 | 100 |
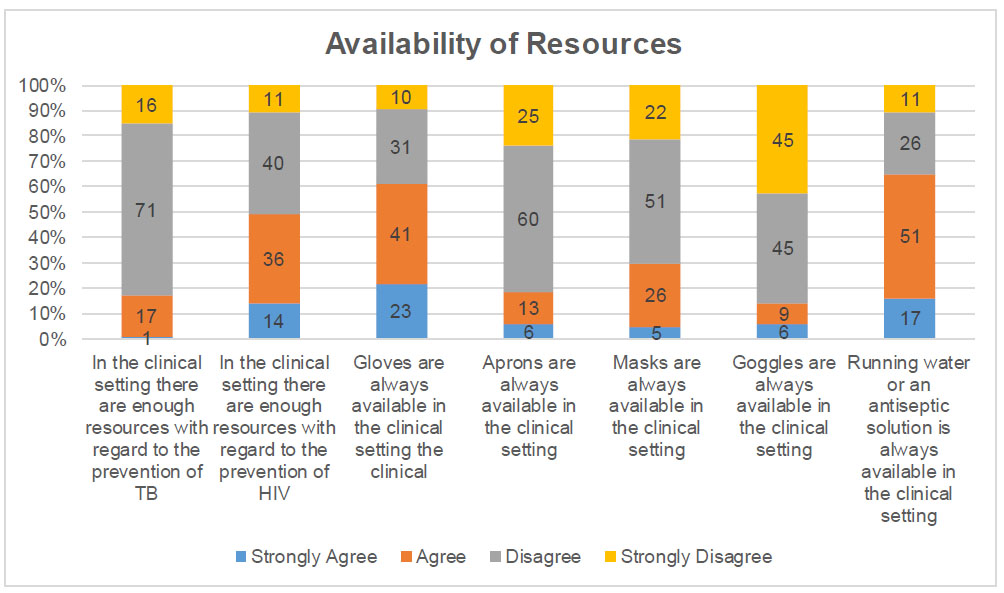
Availability of resources.
3.2. Factors Affecting Student Nurses’ Adherence to Standard Precautions
In this study, factors influencing compliance with standard precautions for the prevention of TB and HIV have been discussed under four sub-topics, namely the availability of resources, measures taken by student nurses, hospital support role, and university support role. A four-point Likert scale was utilized using the following frequency responses: strongly agree, agree, disagree, and strongly disagree. The frequency responses ‘strongly agree’ and ‘agree’ were combined and presented as an agree option, while ‘strongly disagree’ and ‘disagree’ were combined and expressed as disagree.
3.2.1. Availability of Resources
As illustrated in Fig. (1), only 17.1% (n=18) of the participants agreed that in the clinical setting, there were enough resources with regard to the prevention of TB, while the majority of the participants, i.e., 82.9% (n=87), disagreed with this statement. Regarding HIV, 4 participants did not answer this question so the total number of participants who responded to this question was 101. Responses to this question were varied. Almost half of the participants, i.e., 47.6% (n=50), agreed that there were enough resources with regard to the prevention of HIV in the clinical area, while 48.6% (n=51) of the participants disagreed with this statement. Students were then asked about the availability of gloves, aprons, masks, goggles, and running water, and their answers still varied, as presented below.
• A large group of participants, i.e., 61% (n=64), agreed that gloves were always available in the clinical setting, while unfortunately, 38.1% (n=41) of the students disagreed.
• Only 18.3% (n=19) of the participants agreed that aprons were always available in the clinical setting, and the majority of the students, i.e., 81.7% (n=85), disagreed that aprons were available, while 1% (n-1) did not answer.
• One participant did not answer the question regarding masks, making the total respondents of participants for this question to be 104. A small portion of participants, i.e., 29.5% (n=31), agreed to the availability of masks in the clinical setting, while the majority of participants thought otherwise, accounting for 69.5% (n=73) of the participants.
• The least number of participants, i.e., 14.3% (n=15), agreed with the availability of goggles, while the majority of the students, i.e, 85.7% (n=90), disagreed with this statement.
• Most students, i.e., 64.8% (n=68), agreed to the availability of running water or an antiseptic solution in the clinical setting, while on the other hand, 35.2% (n=37) disagreed with this statement.
In general, gloves and hand washing equipment were the only resources having higher scores in terms of availability according to these students. Lack of this basic PPE does not work in any department in the hospital as some infections are airborne and some are spread through contact, but it becomes worse in departments, like maternity and theater, where there are splashes of blood and body fluids.
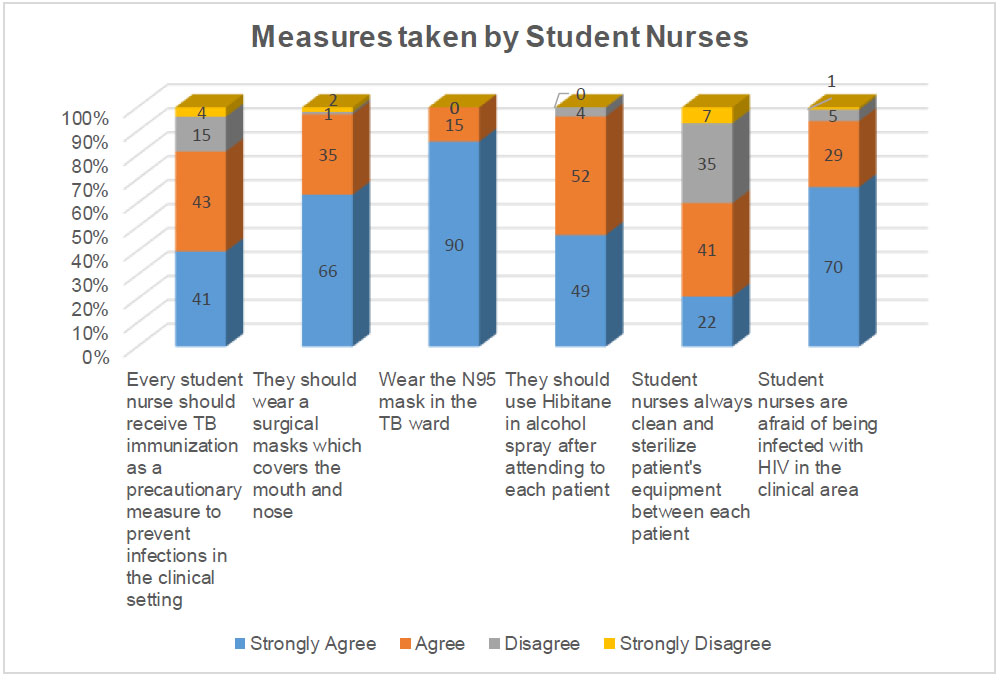
Measures taken by student nurses.
3.2.2. Measures taken by Students
This variable is summarized in Fig. (2). The question on TB immunization was answered by 103 students, of whom, 80% (n=84) agreed that all student nurses should receive TB immunization as a precautionary measure to prevent infections in the clinical setting, but on the contrary, 18.1% (n=19) disagreed with this statement. Many student nurses, i.e., 96.2% (n=101), agreed that they should wear a surgical mask that covers the mouth and nose, while a very small fraction, i.e., 3% (n=3) disagreed with this statement; however, 1% (n=1) of the nurses did not answer. All of the participants, i.e., 100% (n=105), agreed that students should wear the N95 mask in the TB ward. Most students showed agreement with the notion that a Hibitane alcohol spray should be used after attending to each patient, accounting for 96.2% (n=101). Only 3.8% of the respondents (n=4) disagreed with this statement. The students’ responses were divided with respect to cleaning and sterilizing equipment, as some of them, i.e., 60% (n=63), agreed that they always clean and sterilize patient equipment between caring for each patient; however, 40% (n=42) of the respondents disagreed with this statement.
From the answers, student nurses have been found to be more motivated to practice precautionary measures to protect themselves and their patients. This explains why 94.3% (n=99) of them admitted to be afraid of being infected with HIV in the clinical area. The least number of students, i.e., 5.7% (n=6), disagreed with this statement.
3.2.3. Hospital Support Role
Most of the participants, i.e., 83.8% (n=88), agreed that most HIV prevention methods learned in class were practiced in the clinical area, while only 16.2% (n=17) disagreed with the fact. As far as HIV prevention is concerned, students reported that they could smoothly integrate theory into practice as what they have learned in class is also found in practice in the clinical area. However, with respect to TB, the numbers were slightly reduced as 69.5% (n=73) agreed that most of the TB prevention methods learned in class are practiced in the clinical area, while some of the students, i.e., 30.5% (n=32), disagreed.
Most participants (77.1%; n=81) agreed the experienced nurses in the clinical area to be supportive in facilitating knowledge of standard precautions, while 22.9% (n=24) of the participants disagreed. With regards to role modeling, the students were also divided, but more than half of them thought that the nurses in the clinical area were not good role models in the use of protective measures. 45.8% (n=48) of the participants agreed that the nurses in the clinical area were good role models for the use of protective measures, while 55.2% (n=57) disagreed. Furthermore, 78.1% (n=82) agreed that the hospital provides training on infection prevention, while a small group of the students, i.e., 21.9% (n=23), disagreed.
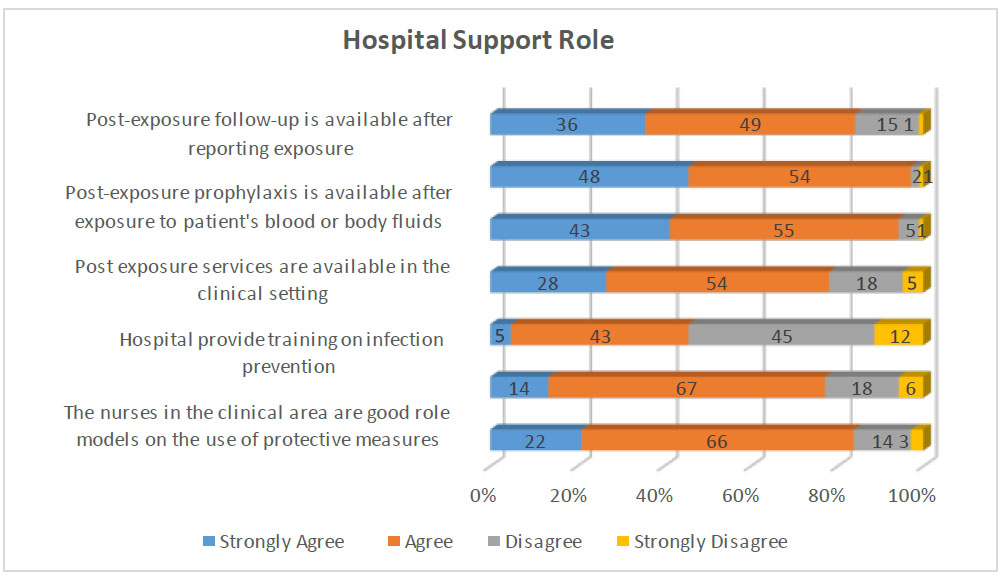
Hospital support role.
One participant did not answer the question on Post-exposure Prophylaxis (PEP), but most of the students, i.e., 93.3% (n=98), agreed that post-exposure services are available in the clinical setting. Unfortunately, 5.7% of the respondents (n=6) disagreed with this statement. A lot of the student nurses, i.e., 97.1% (n=102), agreed post-exposure prophylaxis to be available after exposure to a patient's blood or body fluids, and only 2.9% (n=3) disagreed with this statement. On the follow-up, however, the numbers in terms of agreement have slightly reduced; 81% (n=85) of the participants agreed post-exposure follow-up to be available after reporting exposure. However, a small number of the students 15.2% (n=16) disagreed with this statement and 3.8% (n=4) did not answer (Fig. 3).
In summary, it can be concluded that if not 100%, the hospital, to a large extent, teaches students about infection control, emphasizes what has been learned in class, and mentors students during their practice in the clinical area and in case of accidental exposure, assisting them by providing the appropriate measures.
3.2.4. University Support Role
As illustrated in Fig. (4), a good percentage of the students, i.e., 90.5% (n=95), agreed that the university continuously teaches them on how to prevent contracting infections in the clinical setting. However, not all students agreed with this statement, as 9.5% (n=10) disagreed. The majority of student nurses, i.e., 91.4% (n=96), also agreed the information on standard precautions learned in class to be clear and adequate. A few of them, i.e, 8.6% (n=9), however, disagreed. But generally, the university has been reported to be doing a good job with respect to supporting students as far as standard precautions are concerned.
4. DISCUSSION
One of the important factors in adherence to standard precautions is the availability of resources, like Personal Protective Equipment (PPE), without which there are no means for health workers to comply. In the current study, only 17.1% of the students agreed that there are enough resources for TB prevention, and 47.6% agreed with respect to HIV prevention. A literature review previously done on standard precautions found the inadequate provision of equipment and protective equipment to be one of the reasons and consequences for low adherence to standard precautions by the nursing team [14]. One study performed in Nigeria showed that more than two-third (80.6%) of the participants reported that only gloves and face masks are provided for surgical and delivery procedures [15]. In this study, the availability of resources was reported as worse, since only gloves (61%) and running water (64.8%) were informed by the students to be available. It comes as no surprise that another study done in Eswatini showed only 51.4% of student nurses to indicate that they always use PPE [8]. However, in this study, with respect to other PPE, like aprons, masks, and goggles, only 18.3%, 29.5%, and 14.3% of the students reported their availability. With such a lack of PPE, it has been reported to be difficult to adhere to standard precautions. In agreement with this statement, 48.6% of the student nurses, in a study performed in Nigeria, alluded that they cannot practice standard precautions because of the inadequate supply of barrier equipment [16]. According to the findings of this research study, the lack of resources is one of the factors that negatively influences adherence to standard precautions for TB and HIV prevention. Another study has shown healthcare workers having access to PPE to be 2.87 times more likely to be compliant than those not having PPE [2].
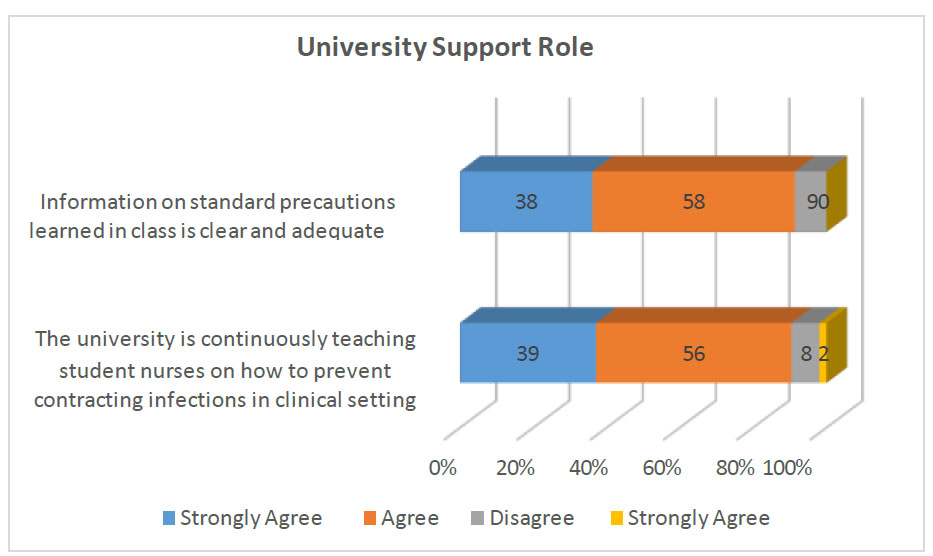
University support role.
As a lot can be done by the government, the hospitals, and the university to ensure adherence to student nurses regarding standard precaution, it all starts at a personal level. The students’ opinions and willingness count, whether or not they are going to comply. Many student nurses (96.2%) agreed that they should wear a surgical mask that covers the mouth and nose, and all of the students (100%) agreed that they should wear the N95 mask in TB wards. Similarly, a previous study showed that 89.5% of the students believed in wearing masks and other protective devices as part of precautionary measures [15]. Most students (96.2%) agreed that a Hibitane alcohol spray should be used after attending to each patient. Another study showed slightly different results where only 63.8% of the students believed they should perform hand hygiene in between patient contact [17]. The students’ responses were divided in terms of cleaning and sterilizing equipment; some (60%) agreed that they always clean and sterilize patient equipment between each patient. Similarly, a study done in Australia showed that 52% of the students believed they should always clean medical equipment after use [18]. TB immunization is a precautionary measure that students can adopt to prevent themselves from contracting TB during practice in the clinical area. In this study, 80% of the student nurses agreed that they should receive TB immunization. However, the effectiveness of the TB vaccine (BCG) has been said to be poor in adults and, therefore, it is not used in Eswatini [19, 20]. The students reported that they can use these measures to protect themselves in the CLE, but still, 94.3% of them admitted that they are afraid of being infected with HIV in the clinical area. These results are different from those of a study performed involving the Thai population, where only 41% of the participants reported that they were “scared” by the thought of contracting HIV/AIDS at work [21].
For student nurses to grasp the concept of standard precaution, it should be first taught to them. We have also come to know from this study that the hospital teaches students about infection prevention as 78.1% of the participants agreed to the availability of such training. These findings are similar to those of a study done in South Africa where most of the students reported that they had demonstrations, orientation sessions, and clinical teaching regarding infection control in the clinical area [22]. After teaching the students, it is important that these standard precautions be clearly put into practice in the CLE. In this study, when students were asked if most of the HIV and TB prevention methods learned in class are practiced in the clinical area, 83.8% and 69.5%, respectively, agreed to it. On the contrary, another study on the experiences of nursing and midwifery students in clinical placements stated that students have reported some practices done by qualified nurses to be against to what they have learned in the class [23].
Another important aspect that can facilitate knowledge and adherence to standard precautions could be having supportive nurses in the clinical area. In this study, 77.1% of the students stated the experienced nurses to be supportive; however, only 45.8% agreed to be good role models. Negative role modelling was also found in a study conducted in South Korea where student nurses discussed various occasions related to non-compliance, including poor hand hygiene, the non-use of PPE, and poor needle recapping by nurses [24]. The students further stated that they have difficulty in adhering to standard precautions when they are working with nurses who do not comply. The hospital has also been reported to have the responsibility of providing Post-exposure Prophylaxis (PEP) services in case one of the health workers, including student nurses, is exposed to blood and body fluids during their practice. In this study, 93.3% of the participants agreed to the availability of post-exposure services in the clinical setting, and 81% agreed that post-exposure follow-up is done. This is good because the safety of the students is secured in this matter. It is important that student nurses should be aware that PEP services are available in case of exposure. In another study, not all the student nurses were aware of the availability of PEP in the units they were working in, though the majority reported being aware of it; thus, 60.9% of the first-year, 75% of the second-year, 76.9% of the third-year, and 84.1% of the fourth-year students knew about the availability of PEP in the Primary Healthcare (PHC) facilities [22].
The university is the primary institute responsible for teaching the student nurses about standard precautions. In this study, 90.5% of the students agreed that the university continuously teaches them on how to prevent contracting infections in the clinical setting and 91.4% also agreed information on standard precautions learned in class to be clear and adequate. In a study done in Cyprus on factors influencing compliance to standard precautions, the participants reported that continuous reminders about the need for implementing standard precautions improve compliance [25].
CONCLUSION
A lot has been done to ensure adherence among student nurses, which includes training in the hospital, PEP services, supportive nursing personnel, and the continuous support role of the university. However, as student nurses face the reality of emergency situations, lack of equipment, and working with nurses who do not adhere to standard precautions in the CLE, they find themselves not complying like they should. With this poor adherence to standard precautions, student nurses are at a risk of infecting themselves and their patients during their practice in the clinical area. Through this research study, the researchers appeal to the universities and the hospitals to cling to the factors facilitating adherence to standard precautions and eliminate the barriers to adherence to standard precautions among student nurses.
LIMITATIONS
The researchers have used self-reporting and this may cause a problem because some participants can give incorrect information. Also, this study was conducted in one university, yet performing the study in multiple universities could offer a larger sample size and diversity, enhancing the generalizability. The study could benefit from a deeper exploration of the contextual factors that might influence adherence, such as institutional policies and cultural attitudes, towards TB and HIV prevention.
FUTURE RESEARCH
Further research should be conducted on strategies and interventions to enhance adherence to standard precautions among student nurses. Furthermore, a longitudinal observation study needs to be conducted on the same subject to support the findings of this study.
AUTHORS’ CONTRIBUTION
Ncobile Sidzandza Victoria Gina, Melitah Molatelo Rasweswe, and Miriam Mmamphamo Moagi contributed to conceptualization,data curation, formal analysis, investigation, project administration, methodology design, validation, writing of the original draft, and writing, review, and editing. Melitah Molatelo Rasweswe and Miriam Mmamphamo Moagi supervised the study. Ncobile Sidzandza Victoria Gina and Miriam Mmamphamo Moagi contributed to the visualization.
LIST OF ABBREVIATIONS
| CLE | = Clinical Learning Environment |
| HAI | = Hospital-acquired Infection |
| HIV | = Human Immune Virus |
| TB | = Tuberculosis |
ETHICAL STATEMENT
This study was approved by the Eswatini Health and Human Research Review Board and the University of Pretoria’s ethics committee.
AVAILABILITY OF DATA AND MATERIAL
All the data and supporting information are provided within the article.


