All published articles of this journal are available on ScienceDirect.
E. Coli-caused Foodborne Outbreak in Bantul Regency, Indonesia, 2023: A Retrospective Cohort Study
Abstract
Background
On October 18, 2023, Bantul District Health Office received notification from the Pleret Public Health Center (PHC) that several employees were sick with diarrhea and abdominal pain.
Objective
An epidemiological investigation was carried out to confirm the outbreak, detect additional cases, identify risk factors and causes, and recommend preventive measures.
Methods
This study employed active case finding followed by a retrospective cohort study. Individuals who reported diarrhea, stomachache, or malaise after consuming chicken distributed on Monday, October 16, 2023, were considered. Data were obtained through an e-questionnaire and direct interviews with all employees, their families, and food handlers. Food samples were sent to the health laboratory for analysis. Chi-square and multiple binomial regression were used to analyze the data.
Results
There were 68 sick individuals among the 140 people interviewed. Most cases occurred in women (52.9%), the 41-50-year age group (26.5%), and PHC employees (64.7%). Diarrhea (95.6%), abdominal pain (70.6%), and malaise (19.1%) were the most prevalent symptoms. The outbreak was identified as a common source, with incubation periods ranging from 1 hour to 20 hours, with an average of 5 hours and 6 minutes. Fried chicken was linked to a higher chance of becoming afflicted in this outbreak (aRR=5.09; 95% CI=1.33-19.47). E. Coli and mold were detected in the laboratory results.
Conclusion
This study concludes that there was a foodborne outbreak among PHC employees due to E. coli. Therefore, improving the foodborne disease surveillance system and monitoring household food production is needed to prevent outbreaks.
1. INTRODUCTION
Foodborne diseases remain a major public health concern worldwide [1]. In both developed and developing nations, foodborne diseases contribute to the primary cause of morbidity and mortality [2]. The two contributing factors include the general population's greater susceptibility (e.g., the elderly or the immunocompromised), which leads to more serious illness outcomes, and the spread of antibiotic resistance [3]. Another essential aspect is the globalization of food supply chains, which results in large-scale food distribution and the potential for disease transmission. Foodborne infections are also significantly impacted by changes in the virulence of recognized pathogens, new consumption habits, and population movements [4]. Foodborne pathogenic bacteria contamination in food systems is a severe concern that can result in the development of various diseases and even mortality. The World Health Organization estimates that every year, at least 33 million years of healthy life are lost globally as a result of eating unsafe foods [5].
A foodborne disease outbreak happens when two or more people become sick after consuming food that has been epidemiologically confirmed as a source of infection [6]. Food toxicity is caused by the presence of bacterial toxins, which are produced when bacteria proliferate in food. In contrast, food infection occurs when bacteria enter the body via contaminated food, triggering the body's immune response. Both factors can lead to gastrointestinal disease. E. coli and Salmonella are among the most common bacteria responsible for foodborne illnesses [7].
Escherichia coli (E. coli) is a common bacterium found in the human intestines that does not typically cause harm to health [8]. Few strains of E. coli acquire virulence genes through horizontal transfer and cause gastroenteritis. Diarrheagenic Escherichia coli (DEC) is the primary cause of acute gastroenteritis in children. However, until now, DEC-related epidemiology information is limited [9].
In Indonesia, according to the SPIMKER (Sistem Pelaporan Informasi Masyarakat Keracunan) application, the Indonesian Food and Drug Authority (BPOM) reported 122 foodborne outbreaks in 2023. Of the 8,937 individuals who were reported, 4,729 experienced illness, resulting in an attack rate of 52.91%. The case fatality rate was 0.38%, with 18 deaths. From 2019 to 2021, the attack rate increased and then declined in 2022 (45.29% in 2019, 46.62% in 2020, 69.40% in 2021, and 50.64% in 2022). However, the attack rate increased in 2023 compared to 2022 [10].
Based on the food distribution, foodborne outbreaks in 2023 occurred in 29 provinces, with West Java reporting the highest (16.11%), followed by Central Java with 14 cases (11.48%). Microbiological contamination was the most frequent cause of 68 cases, of which 42 (34.43%) were suspected and 26 (21.31%) were confirmed. The outbreaks were caused by pathogens, such as Salmonella, Escherichia coli, Clostridium perfringens, Bacillus cereus, Staphylococcus aureus, and Bacillus cereus. In addition, there were 19 food poisoning outbreaks caused by chemicals, with 13 (10.66%) suspected and 6 (4.92%) confirmed, involving histamine, cyanide, arsenic, and lead (Pb). The remaining 35 cases (28.69%) had unknown causes. Foodborne outbreaks were linked to food produced by households, catering services, snacks, MD food, ML food, and Home Industry Food (PIRT). Over the past five years, home-cooked food has been the leading source of foodborne outbreaks, accounting for 53.28% in 2023, 34.72% in 2022, 52% in 2021, 49% in 2020, and 40.30% in 2019 [10].
On October 18, 2023, the Pleret Public Health Center (PHC) notified the Bantul District Health Office about several employees experiencing diarrhea and stomach aches. The initial assumption was that this incident occurred after they consumed fried chicken served by one of the workers on October 16, 2023. Based on this information, the investigative team conducted an epidemiological investigation and collected food samples, specifically fried chicken, which was suspected to be the source of the food poisoning. An e-questionnaire was distributed to all PHC employees to continue tracking disease cases.
In this view, this investigation aims to establish a working case definition and verify the existence of an outbreak. This assessment must be initiated and completed immediately to avoid further illness. The process should include verifying the validity of the information, collecting data from relevant laboratory examinations conducted, identifying cases and collecting details about them, and ensuring the collection of proper clinical specimens and food samples [6].
2. METHODOLOGY
2.1. Study Design
This study employed active case finding followed by a retrospective cohort design. The inclusion criteria consisted of individuals who consumed fried chicken served on Monday, October 16, 2023, and were considered part of the at-risk population. Exposed cases were defined as those who reported one or more symptoms—such as diarrhea, stomach pain, or malaise—after consuming the fried chicken on that day, while unexposed cases were those who did not consume the fried chicken. Individuals who refused to be interviewed, were too ill, or were unavailable during the epidemiological investigation period were excluded.
2.2. Ethical Approval
This study was conducted following the principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Research Ethics Committee of the Faculty of Medicine, Public Health, and Nursing at Universitas Gadjah Mada (KE/FK/0107/EC/2025).
2.3. Epidemiological Investigation
Epidemiological investigations were conducted by verifying the presence of an outbreak by visiting the PHC and interviewing staff members. Interviews were done with all PHC employees and their families using e-questionnaires to collect data, such as age, gender, food consumption, time of consumption, symptoms experienced, and time of symptom onset. We collected food samples from a staff member who kept leftover fried chicken in the health center's refrigerator. On October 18, 2023, the samples were collected and sent to the regional laboratory for analysis.
Biological samples were not collected in this study. On October 19, 2023, an environmental study was conducted by interviewing food sellers and conducting observations by visiting food production locations to observe food preparation activities, such as cooking, storing, and serving.
2.4. Sample Size
This study used total sampling. All employees and their families who received or consumed chicken were interviewed.
2.5. Statistical Analysis
The data were analyzed with STATA 17 software [11]. The study used descriptive analysis, which involved describing the data based on the person (age, gender, signs and symptoms, time of onset, and food consumed) and time variables. The epidemic curve was used to analyze time variables.
To determine food-specific risk, a bivariate analysis was performed using a risk ratio (RR) with a 95% confidence interval. The chi-square test was also utilized to assess the hypothesis for each food item. Food items with a p-value less than 0.25 were subjected to multivariable analysis, which estimated the RR adjusted by multiple binomial regression.
3. RESULTS
3.1. Attack Rate and Clinical Symptoms
Based on the information gathered, 140 people were interviewed, of whom 68 were found to be ill. The majority of cases occurred among women (52.9%), in the 41-50 age group (26.5%), and among PHC employees (64.7%) (Table 1). No warning signs or symptoms were identified during the outbreak study. The most common symptoms included diarrhea (95.6%), stomachache (70.6%), and malaise (19.1%). Further details on the symptoms can be found in (Fig. 1).
3.2. Incubation Period
Based on the epidemic curve (Fig. 2), this outbreak followed a common source transmission pattern, with cases increasing rapidly. The first case occurred on October 16, 2023, at 7 p.m., peaking at 3 a.m. on October 17, 2023, before gradually decreasing. The incubation period ranged from 1 to 20 hours, with an average of 5 hours and 6 minutes.
The food menu for this outbreak included fried chicken, chili sauce, and a side salad, all stored in a lunch box lined with banana leaves. A bivariate analysis showed that both fried chicken and chili sauce were statistically significant foods. Fried chicken had the highest and most significant relative risk (RR), with an RR of 5.82 and a 95% CI of 1.54 to 21.97 (Table 2).
Multivariable analysis using multiple binomial regression is shown in Table 3. Only fried chicken was found to be statistically significant in this study. According to multivariable analysis, fried chicken had the largest and most significant relative risk, with an RR of 5.09 and a 95% confidence interval of 1.33-19.47. This means that after controlling for other variables, people who ate fried chicken had a five-fold higher risk of sickness than people who did not eat fried chicken.
| Characteristic | Population at Risk | Number of Case | Attack Rate (%) |
|---|---|---|---|
| Sex | |||
| Male | 59 | 32 | 47.1 |
| Female | 81 | 36 | 52.9 |
| Age (years) | |||
| 1-10 | 10 | 5 | 7.4 |
| 11-20 | 12 | 6 | 8.8 |
| 21-30 | 26 | 15 | 22.1 |
| 31-40 | 27 | 13 | 19.1 |
| 41-50 | 29 | 18 | 26.5 |
| 51-60 | 26 | 8 | 11.8 |
| 61-70 | 5 | 3 | 4.4 |
| 71-80 | 3 | 0 | - |
| 81-90 | 1 | 0 | - |
| 91-100 | 0 | 0 | - |
| 101-110 | 1 | 0 | - |
| Occupation | |||
| PHC employees | 83 | 44 | 35.3 |
| Not PHC employees | 57 | 24 | 64.7 |
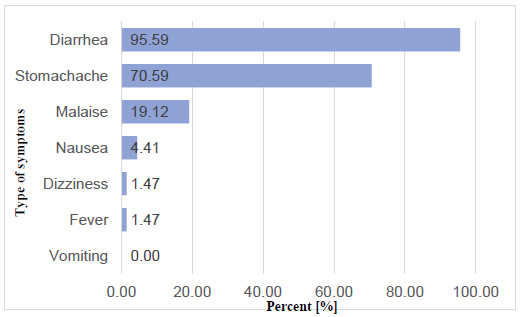
Clinical symptoms of the foodborne outbreak in Public Health Center, Bantul, Yogyakarta.
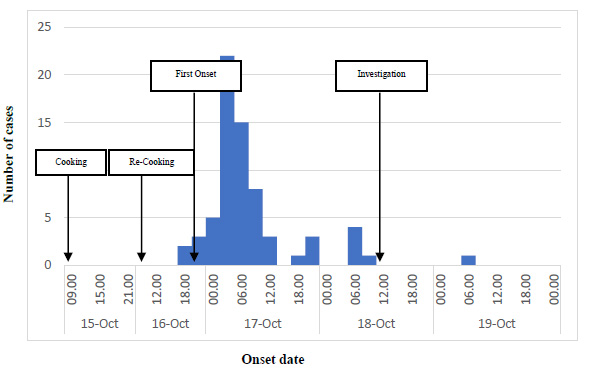
Epidemic curve of the foodborne outbreak in Public Health Center, Bantul, Yogyakarta.
| Food Items | Ill | Not Ill | RR | 95% CI |
|---|---|---|---|---|
| Fried Chicken | ||||
| Exposed | 66 | 53 | 5.82 | 1.54- 21.97 |
| Unexposed | 2 | 19 | ||
| Chili Sauce | ||||
| Exposed | 34 | 19 | 1.64 | 1.17-2.28 |
| Unexposed | 34 | 53 | ||
| Side Salad | ||||
| Exposed | 16 | 14 | 1.12 | 0.76-1.66- |
| Unexposed | 52 | 58 |
| Food Items | Ill | Not Ill | aRR | 95% CI |
|---|---|---|---|---|
| Fried Chicken | ||||
| Exposed | 66 | 53 | 5.09 | 1.33-19.47 |
| Unexposed | 2 | 19 | ||
| Chili Sauce | ||||
| Exposed | 34 | 19 | 1.32 | 0.96-1.82 |
| Unexposed | 34 | 53 |
| Characteristic | Bacillus cereus | Staphylococcus aureus | Escherichia coli | Outbreak |
|---|---|---|---|---|
| Symptoms | ||||
| Diarrhea | ± | ± | ± | + |
| Stomache | + | + | + | + |
| Malaise | - | - | - | + |
| Nausea | + | + | - | ± |
| Dizziness | - | - | + | ± |
| Fever | - | - | ± | ± |
| Vomiting | + | + | - | - |
| Incubation Period | 2-4 hours | 30 minutes-8 hours | 12-48 hours | 1-20 hours |
| Risk Factors | Storing cooked food at room temperature, storing cooked food in a big container in the refrigerator, and preparing meals several hours before serving | Storing cooked food at room temperature, storing cooked food in a big container in the refrigerator, touching cooked food at room temperature, and preparing meals several hours before serving | Infected people handling food, insufficient cold storage, inadequate cooking, cleaning, and hygiene, ingesting raw or undercooked meat | Fried chicken is cooked repeatedly with insufficient cold storage. |
| Food Characteristic | Cooked rice | Ham, meat and poultry products, high protein foods | Half-cooked meat, cheese, water | Fried chicken |
| Type of Sample | Results | |
|---|---|---|
| Food Samples | Fried Chicken | Mold/yeast, E. coli pathogen, Proteus mirabilis, Escherichia coli non-pathogen |
3.3. Laboratory Investigation
Based on the symptoms, incubation period, type of food, and risk factors, E. coli was identified as the cause of the food poisoning (Table 4). This conclusion was further supported by laboratory results, which confirmed the presence of the E. coli pathogen in the food sample (Table 5).
3.4. Environmental Investigation
Following up on interviews with food handlers, it was discovered that no food handlers had become sick while handling food that day or in the prior few days. Chicken orders for Monday, October 16, 2023, began to be processed the day before, on Sunday, October 15, 2023. A total of 100 boxes were ordered. The ordered menu consisted of fried chicken, chili sauce, and a side salad. A lunchbox lined with banana leaves was used to pack orders.
The orders were sent in two parts on Sunday, October 15, 2023. The chicken was washed, seasoned, and pan-simmered for 40 minutes. After being removed from the pan, the chicken was left to air out in a container. It was then stored in the cupboards to be fried the following day.
On Monday, October 16, 2023, at 4:30 a.m., the chicken was reheated by boiling in a hot pan and seasoned for 10 minutes. The chicken was fully cooked and ready for packing by 6:30 a.m. At 8:00 a.m., the food items—fried chicken, chili sauce, and side salad—were wrapped in plastic and packed in lunchboxes lined with banana leaves. The delivery process was completed by 9:30 a.m. at the PHC. Food handlers wore Personal Protective Equipment (PPE) (aprons, work clothing/chef attire, hair covers) and followed proper cooking practices, including soap cleaning. Nonetheless, insufficient cooking and improper cold storage were identified as risk factors for this outbreak.
4. DISCUSSION
The epidemiological investigation identified fried chicken as the source of the foodborne illness. Laboratory samples of the fried chicken tested positive for mold/yeast, pathogenic E. coli, Proteus mirabilis, and non-pathogenic E. coli. This supports the differential diagnosis linking the outbreak to E. coli bacteria. The type of food consumed, the symptoms, and the incubation period—ranging up to 20 hours—were key factors in determining the cause of the illness.
Escherichia coli are usually harmless bacteria that live in the intestines of humans and animals and contribute to intestinal health. However, consuming food or water contaminated with specific strains of E. coli can result in gastrointestinal problems ranging from mild to severe. Leafy greens, sprouts, raw milk and cheese, raw beef, and raw poultry have all been linked to previous E. coli outbreaks in the United States [12].
In Indonesia, pathogenic bacteria were shown to be the most common cause of food poisoning, contributing to 74.85% of cases (8,615 cases) and a CFR of 0.1%, with E. coli, Bacillus cereus, and Staphylococcus sp being the most prevalent. The presence of E. coli bacteria indicates poor sanitation and hygiene procedures. Several E. coli strains, particularly enterotoxigenic strains, may cause sickness in humans through various pathways. These bacteria cause toxins to be produced in the gastrointestinal tract [13].
Enterotoxigenic Escherichia coli (ETEC) is the primary intestinal bacteria responsible for tens of millions of cases of gastrointestinal illness annually [14]. ETEC infection is spread by contaminated food and water, particularly in underdeveloped nations with inadequate infrastructure for clean drinking water and waste disposal. Previous studies have shown that ETEC can remain in excrement for over six months and that they typically appear in water as biofilms, which increases their chance of survival [15].
In this study, the primary symptoms of E. coli infection included abdominal pain, diarrhea, vomiting, and fever [16]. These symptoms align with those observed in this outbreak, particularly diarrhea and stomach pain. Another study noted that E. coli infections typically begin with non-bloody diarrhea, which resolves without complications. Additionally, compared to other types of bacterial gastroenteritis, patients with E. coli infections often experience more intense abdominal pain. Diarrhea usually develops within two to twelve days after consuming contaminated food [2].
Previous studies have identified E. coli in poultry and duck hatcheries, as well as in environmental samples and from humans in Egypt. In one study, E. coli was detected in 62 of 171 samples, representing 36.3% of the total [17]. Additionally, E. coli O157:H7 was isolated from various meat and poultry specimens, including ground beef, pork chop, pork loin, pork hock, ground pork, chicken leg, turkey drumstick, lamb riblet, lamb loin chop, lamb shoulder blade chop, and lamb leg [18]. This is consistent with the findings in this outbreak, where fried chicken was identified as the primary source. It is possible that the infection was present from the outset, even before the food preparation process began.
E.coli bacteria can normally live at temperatures ranging from 8 to 46 degrees Celsius. These bacteria bacteria can be found in the kitchen, where raw materials are produced and processed before entering the cooked meal via hands, tool surfaces, cooking areas, and equipment [19]. According to our study, the chicken was placed in a container to allow it to air out after being removed from the pan. The chicken was then placed in the cupboards to be fried the following day. This indicates that the chicken was placed in an unsealed container. This is consistent with another study, which found that an unsealed food container has twice the risk of E. coli contamination [20].
We also discovered that the chicken was reheated many times, which could result in contamination. In a previous study, the analysis revealed that two re-heated food samples tested positive for E. coli. However, further research revealed no significant changes between re-heating and direct-cooking food [21]. Therefore, all types of foods are equally susceptible to contamination [22].
These findings raise concerns regarding food safety. One crucial preventive measure is the promotion of proper personal hygiene practices. Additionally, providing essential facilities, such as access to clean water, handwashing stations with soap, changing rooms, and proper work attire (including uniforms, aprons, head coverings, masks, and gloves), is extremely beneficial [20].
CONCLUSION
There was an outbreak of food poisoning at the Pleret Public Health Center. Those at risk in this food poisoning outbreak included women between the ages of 41 and 50 and employees of public health centers. The most common symptoms experienced were diarrhea, stomach pain, and malaise. The incubation period lasted from 1 hour to 20 hours, with an average of 5 hours and 6 minutes. Furthermore, fried chicken was the source of food poisoning in this outbreak, with E. coli bacteria serving as the causative agent. Inadequate cooking and inappropriate cold storage were additional risk factors. Thus, raising concerns about food safety with employees and food handlers is essential.
STUDY LIMITATIONS
Our epidemiological investigation has some limitations. The results showed mold/yeast contamination since the samples of fried chicken were collected on October 18, 2023, rather than February 16, 2023, the initial day of the suspected outbreak. Additionally, no biological samples were collected for this study. This study employed total sampling at the health facility, but severely ill people who refused to be interviewed were excluded; thus, they may not be representative of the population.
AUTHORS’ CONTRIBUTIONS
S.I.I., D.A.H., and B.S.W. were responsible for the study conception and design. S.I.I. and D.A.H. handled the data collection. S.I.I., B.S.W., and S.A. performed the analysis and interpretation of the results. S.I.I., B.S.W., and S.A. also contributed to drafting the manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DEC | = Diarrheagenic Escherichia coli |
| PHC | = Public Health Center |
| RR | = Risk ratio |
| PPE | = Personal Protective Equipment |
| ETEC | = Enterotoxigenic Escherichia coli |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Research Ethics Committee of the Faculty of Medicine, Public Health, and Nursing at Gadjah Mada University, Indonesia (KE/FK/0107/EC/2025).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [B.W] upon request.
ACKNOWLEDGEMENTS
The authors would like to appreciate the assistance provided by the Pleret Public Health Center and the Bantul District Health Office during the outbreak investigation.


