All published articles of this journal are available on ScienceDirect.
Enhancing the Role of Primary Care Private Practitioners in Addressing Gaps in TB Care: An Analysis of National TB Data from Medan
Abstract
Introduction
Tuberculosis is a global problem, and the prevalence of TB in Indonesia is the second highest in the world. In 2022, tuberculosis (TB) affected an estimated 10.6 million individuals worldwide. Most patients in Indonesia, especially those with cough complaints, first seek treatment from private health services. However, these health service providers have limitations for TB diagnosis and treatment, leading to poor and inadequate treatment and the risk of developing drug resistance.
Aim
The purpose of this study was to increase the role of private practitioners, especially doctors in primary care, who provide continuous, comprehensive, first-contact, and coordinated services to fill TB treatment gaps, ranging from suspected TB to complete and cured treatment.
Methods
This is a retrospective observational study using the TB registry in Medan, Indonesia, during the year 2021, which includes data on newly diagnosed and relapsed cases of tuberculosis patients who were treated completely, cured, unsuccessfully, lost to follow-up, and died. The TB registry was recorded in the SITB (TB Information System) and can be accessed nationally. The instrument uses the form TB 08 SITB, which was filled out in the city. Data were analyzed univariately using SPSS presented in the form of frequencies and percentages and bivariate using contingency coefficient test in the form of value and approximate significance.
Results
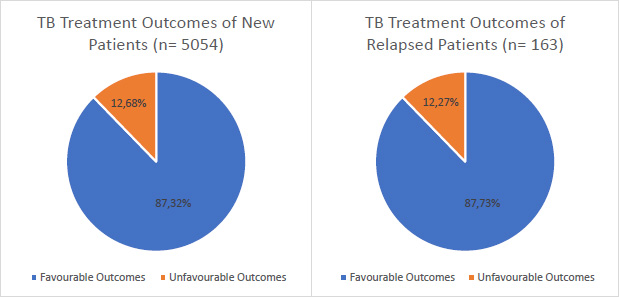
The treatment success rate among all subjects in new TB cases was approximately 87.3%. Therefore, there was a gap in TB treatment adherence of 12.7%. The treatment success rate for relapsed TB cases was 87.7%, so there is a 12.3% gap in treatment adherence. Data analysis revealed a significant association between TB classification and treatment outcomes.
Conclusion
There are gaps in TB services ranging from screening and early detection of suspected TB to diagnosis, treatment, notification, and evaluation of TB treatment outcomes. Increasing the role of private practitioners, especially doctors in primary care as first contact, continuity care, and comprehensive and coordinated care in TB control will be useful in filling TB service gaps.
1. INTRODUCTION
Variations in prevalence and management approaches throughout nations make tuberculosis (TB) a persistent global health concern. Recognizing the tuberculosis care cascades is crucial for evaluating the efficacy of tuberculosis programs and identifying gaps in care delivery [1]. There are differences in TB mortality and prevalence rates across high- and low-burden nations, which emphasizes the necessity for specialized TB management strategies depending on the regional epidemiological context [2]. In 2022, an estimated 10.6 million people fell ill with tuberculosis (TB) worldwide, including 5.8 million men, 3.5 million women and 1.3 million children [3]. Finding gaps in TB care and directing the creation of focused interventions to enhance outcomes can be accomplished by analyzing the efficacy of TB screening initiatives [4].
Government rules and regulations for collaborative management of TB-DM have not been consistently applied in government and private health services. These policies and programs aimed to enhance the private sector's involvement in tuberculosis (TB) treatment by implementing Public-Private Mix (PPM) strategies. The importance of PPM lies in the abundance of evidence demonstrating the weaknesses of private service providers in accurately diagnosing and effectively managing patients with tuberculosis. Currently, the health service infrastructure in Indonesia is heavily reliant on a substantial private sector. Most tuberculosis (TB) patients in Indonesia seek treatment at private healthcare. However, these healthcare providers have limitations regarding TB diagnosis and treatment equipment and insufficient capacity and compliance among health workers. Furthermore, private healthcare services tend to provide delayed notifications of cases and poor quality of TB care, leading to poor and insufficient treatment and a risk for the development of drug resistance.
Key gaps encompass the following: individuals with active tuberculosis in the population who are unable to access health facilities and undergo a TB diagnostic test (Gap 1), those who access locations where diagnostic tests are available but are not successfully diagnosed (Gap 2), those who are successfully diagnosed but are not registered in treatment (Gap 3), those who initiate therapy but fail to achieve treatment success (Gap 4), and those who complete therapy but experience death or TB recurrence within a year (Gap 5) [5]. Globally, the gap between estimated TB incidence and the number of TB patients officially registered approached 75% in 2021, in which Indonesia contributed about 13% of the gap, ranked second just after India with a percentage of 24%. On the other hand, among new or relapse TB patients, the global gap between treatment initiation and treatment success was about 14%, which means the global treatment success rate reached a percentage of 86% [6].
Even in Indonesia, years after that, 175,664 fewer TB cases were detected in 2020 compared to 2019. The COVID-19 pandemic began in 2020, which caused a decline in the number of TB cases discovered. This number is not ideal for TB case detection to occur more quickly [7]. This research aims to investigate the gaps in the tuberculosis care cascade in Medan 2021 and to evaluate the relationship between TB classification and treatment outcomes.
2. METHODS
This retrospective observational study employs the cross-sectional approach to TB registry data in Medan, Indonesia, from January to December 2021. The registry data were accessed from SITB (Sistem Informasi TB/TB Information System), the national TB registry established by the Ministry of Health of Indonesia, which is nationally accessible. The population of the study was the data of TB patients treated and registered in the SITB registry in Medan from January to December 2021. Sampling is conducted to represent the population through the total sampling method. The data consisted of TB patients’ classification based on anatomical site, history of previous TB treatment, and HIV status. The data also included the treatment outcomes of the patients, namely favorable outcomes (treatment completed or cured), unfavorable outcomes (failed, died, or lost to follow-up), not evaluated. Univariate analysis was conducted to determine the characteristics of participants in the form of frequencies and percentages. Bivariate analysis was used to analyze the relationship between TB classification (new and relapsed patients) and treatment outcomes using a contingency coefficient test (p<0.05). Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS Inc.) version 29.0.
3. RESULTS
In 2021, the total number of new tuberculosis (TB) cases reported in Medan was 5,057, while the number of relapse cases was approximately 163. It is important to note that the number of relapse cases does not represent a direct proportion of the new cases reported in the same year. Analysis of demographic characteristics by gender revealed a higher prevalence among males in both categories (Table 1). Among the 5,057 new TB cases, males accounted for approximately 62.05% (3,138/5,057), while females comprised 37.95% (1,919/5,057). In relapse cases, males represented 73.62% (120/163) and females 26.38% (43/163).
3.1. Treatment Outcomes of New TB Cases
Three subjects (0.06%) were not evaluated or transferred to another TB status register in the new TB case category. This indicates that almost all new TB case subjects underwent treatment evaluation (99.94%). The number of subjects based on the classification of new TB cases treatment outcomes were as follows: treatment completed 69.79%, cured 17.53%, treatment failed 0.06%, died 3.05%, and loss to follow-up 9.58% (Table 2).
| Characteristic |
New Patients n (%) |
Relapse Patients n (%) |
|---|---|---|
| Gender (n, %) | ||
| Male | 3,138 (62.05) | 120 (73.62) |
| Female | 1,919 (37.95) | 43 (26.38) |
| Total | 5,057 (100,00) | 163 (100,00) |
| Classification |
New Patients n (%) |
Relapse Patients n (%) |
|---|---|---|
| Patients on TB Treatment | ||
| Evaluated | 5,054 (99.94) | 163 (100) |
| Bacteriologically confirmed | 2,184 (43.21) | 97 (59.51) |
| Clinically confirmed | 2,499 (49.45) | 66 (40.49) |
| Extrapulmonary | 371 (7.34) | 0 (0) |
| Not evaluated/ moved | 3 (0.06) | 0 (0) |
| Bacteriologically confirmed | 2 (66.67) | 0 (0) |
| Clinically confirmed | 1 (33.33) | 0 (0) |
| Extrapulmonary | 0 (0) | 0 (0) |
| Outcomes | ||
| Treatment completed | 3,527 (69.79) | 95 (58.28) |
| Bacteriologically confirmed | 1,078 (30,56) | 41 (43.16) |
| Clinically confirmed | 2,117 (60.02) | 54 (56.84) |
| Extrapulmonary | 332 (9.41) | 0 |
| Cured | 886 (17.53) | 48 (29.45) |
| Bacteriologically confirmed | 857 (96.73) | 44 (91.67) |
| Clinically confirmed | 29 (3.27) | 4 (8.33) |
| Extrapulmonary | 0 (0) | 0 (0) |
| Treatment failed | 3 (0.06) | 0 (0) |
| Bacteriologically confirmed | 2 (66.67) | 0 (0) |
| Clinically confirmed | 1 (33.33) | 0 (0) |
| Extrapulmonary | 0 (0) | 0 (0) |
| Died | 154 (3.05) | 6 (3.68) |
| Bacteriologically confirmed | 67 (43.51) | 3 (50.00) |
| Clinically confirmed | 82 (53.25) | 3 (50.00) |
| Extrapulmonary | 5 (3.25) | 0 |
| Loss to follow-up | 484 (9.58) | 14 (8.59) |
| Bacteriologically confirmed | 67 (37.19) | 9 (64.29) |
| Clinically confirmed | 82 (55.99) | 5 (35.71) |
| Extrapulmonary | 5 (6.82) | 0 (0) |
|
Treatment Outcomes |
New Patients n (%) |
Relapse Patients n (%) |
Value |
Approximate Significance |
|---|---|---|---|---|
| Treatment completed | 3,527 (69.79) | 95 (58.28) | 0.055 | 0.003 |
| Cured | 886 (17.53) | 48 (29.45) | ||
| Treatment failed | 3 (0.06) | 0 (0) | ||
| Died | 154 (3.05) | 6 (3.68) | ||
| Loss to follow-up | 484 (9.58) | 14 (8.59) |
Gap of TB treatment adherence.
3.2. Treatment Outcomes of Relapsed TB Cases
In the relapsed TB category, no cases were evaluated or transferred to another TB status register (n:163, 100%). The treatment outcomes for relapsed TB showed that treatment completed was the most prevalent outcome, accounting for 58.28% of cases. The number of cases cured, loss to follow-up, and death were 29.45%, 8.59%, and 3.68%, respectively. No treatment-failed outcomes were found among the relapsed TB cases that were treated and evaluated (Table 2).
3.3. The Relationship between TB Classification and Treatment Outcomes
The results presented summarize the relationship between TB classification and treatment outcomes. The contingency coefficient test yielded a value of 0.055 with an approximate significance of 0.003, suggesting a statistically significant association between treatment outcomes and patient group classification (p<0.05) (Table 3).
3.4. Gaps: Adherence to Treatment among New TB Cases and Relapsed TB Cases
Fig. (1) illustrates the gap in TB treatment adherence by comparing treatment outcomes between new TB patients and relapsed TB patients. The pie charts show that the proportion of patients with favorable treatment outcomes is slightly higher among relapsed TB patients (87.73%) than new TB patients (87.32%). Conversely, the percentage of patients with unfavorable outcomes is marginally higher among new patients (12.68%) than relapsed patients (12.27%). This small difference suggests that treatment adherence among new TB cases is relatively poor. However, even a slight variation in unfavorable outcomes may indicate potential challenges in adherence that could impact long-term disease control efforts.
4. DISCUSSION
In Indonesia, there were 175,664 fewer TB case notifications in 2020 compared to 2019. The number of TB cases detected until October 2022 was 503,712, showing a 60,477 rise over 2021. According to the data, treatment coverage decreased in 2020 and 2021 but began to rise in 2022. Treatment coverage in 2022 is 52% of the aimed for 90% as of Nov 1, 2022. The Treatment Success Rate (TSR) increased in 2021, but as of October 2022, the TSR 2022 was still 82% of the aimed for 90% [7].
Results of this study showed that among TB patients registered and treated in the registry data in Medan during the year 2021, about 87% have achieved treatment success. In Brazil, another country with a similar burden of tuberculosis cases, a study explored Brazil's Notifiable Disease Information System using a mathematical model, and it revealed that the treatment success percentage of those who started treatment was 81.4% in 2018 [8]. A similar study in Zambia estimated that 86.2% of new/relapse pulmonary TB patients completed their treatment in 2015, and this completion rate increased to 90.3% in 2018 [9].
The length course of TB therapy brought up the problem of non-adherence, nevertheless. One of the key factors influencing treatment outcomes is adherence [10]. Tuberculosis treatment failure can be attributed to various reasons, including forgetfulness, being busy with other work, being out of town or away from the usual place of medication intake, the long duration of treatment, the burden of taking many pills, feeling that medication is unnecessary as symptoms improve, the perception that the condition is not improving. The medication is ineffective, increased appetite after taking the medication, or the TB clinic is far from home [11]. These thoughts are influenced by multiple factors, such as the support provided by treatment supervisors in delivering information about the disease and treatment, the patient's understanding linked to their level of education and knowledge, the duration of the illness and its side effects, the availability of healthcare facilities, and others.
Therefore, it is crucial to emphasize the importance of trained Directly Observed Treatment (DOT) supervisors to monitor each TB patient’s treatment to prevent it from being futile. This is supported by a study by Widani and Sianturi (2020), which showed a significant relationship between DOT support and TB patient adherence to treatment. DOT supervisors are not limited to trained health workers; family members can also play a role as close individuals around the patient [12]. The role of DOT supervisors includes ensuring patients take their medication daily or according to the prescribed dosage, counseling, assisting in the treatment process, offering emotional support, and participating in weight gain programs. Thus, inadequate involvement of DOT supervisors in the treatment process makes patients more susceptible to discontinuing their medication [12, 13].
The relationship between the attitude of healthcare workers and TB treatment outcomes is crucial in determining treatment success. The attitude of healthcare workers, including their behavior, empathy, and professional competence, can influence patient motivation and adherence to the treatment regimen. This is supported by a study at the Waena Health Center, which found significant results regarding the relationship between healthcare workers' attitudes and patient adherence to medication [14]. Poor relationships between patients and healthcare providers can lead to communication breakdowns, causing patients to be unaware of risky behaviors and mistakenly believe that their actions have no consequences [11, 15].
Other institution's experience appears to support this, as the increase in cure rates was brought about not only by the implementation of DOT in Lausanne in the 1990s but also by a management shift that included bettering the education of specialized nurses, hiring translators to improve communication, rearranging appointment schedules, and, most importantly, paying more attention to the social issues that vulnerable populations and migrants faced [16]. The End TB Strategy included three pillars comprising a complete package of interventions. The first pillar focused on integrated, patient-centered care and prevention, which calls for expanding and improving the main TB program activities, such as using contemporary technologies to enhance patient care. Digital technology may, therefore, be a crucial instrument to improve DOT implementation. The Health Belief Model (HBM) can be integrated into digital technologies to enhance further its capacity to modify behavior and promote better adherence to medicine [17].
Furthermore, nutrition plays a crucial role in determining the outcome of treatment for individuals with tuberculosis [18]. Weight gain has been identified as a significant indicator of treatment success and recovery in individuals with tuberculosis [19]. Being underweight or experiencing malnutrition is also linked to an increased risk of tuberculosis (TB) and greater mortality rates during TB treatment [20, 21]. An incremental rise in body weight was noted in a retrospective analysis conducted on tuberculosis patients who had been successfully treated in Chennai, India [22].
According to a study conducted in Vietnam, individuals who experienced weight loss during their therapy were more prone to having an unfavorable outcome compared to patients who did not [23]. Compared to patients who did not gain weight, patients under 40 kg at the start of treatment and who gained more than 5% of their body weight were found to have a lower probability of an unsuccessful treatment outcome. Additionally, they discovered that those who are neither gaining nor losing weight, especially in the first two months of treatment, need to be given special attention since they seem to be more likely to experience a poor course of treatment [24]. A study conducted by the Tuberculosis trial consortium in the USA and Canada revealed that patients who were underweight at the time of diagnosis had a higher risk of experiencing a recurrence. A Randomized control study conducted in Mexico found that adding zinc and vitamin A micronutrient supplements enhanced the therapeutic impact of Tuberculosis treatment. The BMI changed significantly along with the rise in weight, and the nutritional status also changed. For 95% of the patients in the intervention group, all of these were shown to be reliable indicators of treatment success [25]
This study also found that the TB classification (new patients and relapsed patients) was associated with treatment outcomes (p<0.05). This aligns with a study by Faye et al. ( p<0.001). The odds ratio for drug history (previous drug history) suggests that an 84% increase in the likelihood of successful TB treatment is associated with every unit increase in the previous drug history [ 26 ]. However, in other studies, relapse TB had been identified as a protective factor for treatment outcomes (Odds Ratio = 1.26), although this relationship was not statistically significant (p = 0.356) [ 27 ]. However, challenges persist in scaling up these initiatives nationwide. Key barriers include financial constraints, the need for comprehensive training programs for private practitioners, and regulatory hurdles that may hinder seamless integration. Policymakers must address these challenges by developing sustainable funding mechanisms, standardized training curricula, and regulatory frameworks incentivizing private-sector participation. Strengthening public-private partnerships and leveraging digital health technologies could facilitate improved coordination, ensuring private practitioners adhere to national TB guidelines. Expanding such collaborative models could significantly contribute to achieving national TB control goals, reducing disease burden, and improving patient outcomes.
CONCLUSION
This study highlights the significant association between TB classification and treatment outcomes. The findings indicate that while the overall treatment success rate is high for both new and relapsed TB cases, there remains a gap in treatment adherence that requires attention. This study provides important insights into the factors influencing TB treatment adherence in Indonesia, highlighting structural barriers and policy improvement opportunities. Our findings emphasize the need for enhanced collaboration between the public and private healthcare sectors to strengthen patient support systems and improve adherence rates. This research contributes to developing evidence-based policies to optimize treatment success by identifying key gaps in current TB care practices. Future research should explore intervention-based approaches, such as leveraging private-sector engagement, mobile health technologies, and community-based adherence support programs, to enhance TB treatment outcomes. Strengthening these strategies will be crucial in achieving Indonesia’s TB elimination goals and reducing the disease burden.
STUDY LIMITATIONS
This study has several limitations. First, the reliance on self-reported data from patients and healthcare providers may introduce recall and social desirability bias, potentially affecting the accuracy of adherence assessments. Second, the study was conducted within a specific region of Indonesia, which may limit the generalizability of findings to other areas with different healthcare infrastructures and patient demographics. Third, while the study identifies key barriers to TB treatment adherence, it does not directly evaluate the effectiveness of specific interventions, such as private-sector engagement or digital adherence tools, which could offer potential solutions. Future research should address these limitations by incorporating objective adherence measures, expanding the study scope, and testing intervention-based strategies.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: I.I.F. and Y.M: Contributed to study conception and design; R.A: Contributed to the analysis and interpretation of the results; IHE drafted the manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| TB | = Tuberculosis |
| PPM | = Public-Private Mix |
| SITB | = Sistem Informasi TB |
| TSR | = Treatment Success Rate |
| DOT | = Directly Observed Treatment |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The experimentation involving human subjects in this study was reviewed and approved by the Komite Etik Penelitian, affiliated with Universitas Sumatera Utara, Indonesia, under approval number 880/KEP/USU/2021.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The authors certify they have obtained all appropriate patient consent forms.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article. Underlying data: Figshare, https://doi.org/10.6084/m9.figshare.28873895 [28].
ACKNOWLEDGEMENTS
The authors would like to acknowledge the patients who participated in this study and thank Pocut Fatimah Fitri and Junida Sinulingga for helping implement this research.


