All published articles of this journal are available on ScienceDirect.
Perception of Primary Health Care Staff towards the New Model of Care System
Abstract
Introduction
The new Model of Care system is an approach to health services that defines best practices. It aims to ensure that the right people receive the right care, at the right time, from the right team, in the right place. This study assessed the new Model of Care perception among healthcare providers in the primary health care centers in the Eastern Health Cluster.
Methods
This cross‐sectional, observational, and analytic study was conducted between October and December 2023. This study targeted health care providers in the primary health care centers in the Eastern Health Cluster. Various existing questionnaires were adopted to develop a new version of the questionnaire. A total of 142 participants completed the questionnaire.
Results
A (46.5%) understood the concepts of the new Model. The percentage of knowledge of the implementation of the new Model and the continuous training necessary reached (87.32%). A (76.76%) acknowledged that the workplace arranged for conferences, speeches, or meetings related to the new Model, P (<0.006). A (47.18%) were willing to implement the new Model, P (<0.05).
Discussion
The knowledge, awareness, and familiarity with the system and its pathways were investigated, and the results were consistent with those of a previous study.
Conclusion
This study found that health care providers had knowledge, awareness, and were familiar with the new Model and its pathways. These findings highlight the importance of continuous engagement strategies and training to enhance healthcare providers' adoption in order to facilitate the implication of the new Model of Care.
1. INTRODUCTION
National Transformation Program, 2021 reported that Saudi Vision 2030 was launched in 2016 as a roadmap for economic and development efforts, defining goals and outlining commitments and responsibilities [1]. (Aldawsari et al., 2024) reported that Saudi Vision 2030 is based on three main pillars: a vibrant society, a thriving economy, and an ambitious nation. As part of Saudi Vision 2030, the Health Sector Transformation Program (HSTP) was established to contribute to achieving a vibrant society, one of the main pillars of Saudi Vision 2030 [2]. Suleiman & Ming (2025) documented part of Vision 2030, Saudi Arabia is developing a health care framework and model aimed at increasing efficiency, equity, and quality [3]. (Al-Nozha, 2024) summarized that health care transformation in Saudi Arabia aims to restructure the sector into a comprehensive, efficient, and integrated system that prioritizes the health of individuals, including citizens, residents, visitors, and society as a whole [4].
It was reported that the current Saudi health care system is facing many challenges (Health Sector Transformation Program, 2021). The challenges, according to the HSTP in Saudi Arabia, include poor integration between service levels of care, pathway management, infrastructure, coordinated care, communication between providers and patients, a shortage of medications, a lack of standardized clinical guidelines, and variations in the quality and delivery of care. The current health care model tends towards treatment rather than prevention [5].
The Ministry of Health (2023) suggested developing a new Model of Care (MoC) system in 2018 to overcome the challenges mentioned previously. This aligns with the principles set out in the Constitution of the World Health Organization: “Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” [6]. Izzuldeen et al. (2023) illustrated that the new MoC system is designed to ensure that a comprehensive system of care is available to support people with their health and wellness needs: physical, mental, and social well-being [7]. Althuwaybi et al. (2025) reported that the new MoC system represents an innovative framework aimed at improving health care services in a more efficient and effective manner [8].
Althumairi et al. (2023) recommended studies exploring the knowledge and perceptions of primary health care staff towards the new MoC system since the new MoC was developed. Primary Health Care Centers (PHCCs) are important because they serve as the first point of contact between community members and health care providers [9]. The main goal of this research was to assess and evaluate the perceptions of primary health care staff towards the new MoC system in the Eastern Health Cluster. Primary health care staff were assessed because they are the first health care providers seen by patients, which highlights the importance of understanding their readiness and preparedness, knowledge, perceptions, and practices related to the new MoC system. This study provides a baseline for continuing work towards improving the new MoC system and fills the gap in the literature.
1.1. Objectives
This study assessed the new Model of Care perception among healthcare providers in the primary health care centers in the Eastern Health Cluster. This study assesses primary health care staff knowledge about the pathways of different systems of care within the new MoC system. It measures the awareness of the importance of implementing the new MoC system and describes the potential of the new model. In order to connect areas within the health care sector and streamline workflow pathways from the perspective of primary health care staff. Additionally, this study aims to measure the role of the new MoC system in facilitating health care transformation according to the perceptions of primary health care staff.
1.2. Literature Review
Alhazmi (2021) suggested that the Ministry of Health (MOH) is responsible for regulating the health care system and providing health care services throughout the country [10]. Wan Puteh et al. (2020) reported that MOH provides 60% of the total health services through 13 health directorates in Saudi Arabia and is the main government provider. Other government health care providers offer comprehensive health services to the target population, usually employees and their families, and account for 20% of health services. Their budgets are allocated directly from the Ministry of Finance through their ministries and agencies [11]. Gurajala (2023) illustrated that PHCCs were providing basic health care services, including preventive care, health education, and screening services. Secondary health care services were provided by specialized hospitals and centers, which provide more advanced health care services, including diagnostic services, surgical procedures, and emergency care [12].
Alasiri & Mohammed (2022) summarized that there are challenges in the current health care system in terms of the quality of patient services due to the lack of standardization of protocols and treatment pathways and differences in their provision [13]. Chowdhury et al. (2021) reported that the new MoC system provides several benefits that constitute the core of health care transformation integrated services; improving the patient experience by offering clear system of care pathways that deliver high-quality, timely and accessible services; organizing and directing numerous initiatives; enabling value-based health care financing by linking payment mechanisms to the care pathways and outcomes of the new MoC system; and facilitating sharing of national knowledge and care. In order to improve the design of the new MoC system, it was necessary to collect data and assess the current state of the health care system. Furthermore, to determine the indicators of the current health care situation, a survey was distributed within the Kingdom of Saudi Arabia to more than 60,000 citizens. Additionally, more than 2,500 health care professionals from around the world participated in the discussions, and more than 1,000 were surveyed to understand the perspectives of these target groups. The main objective was to identify possible solutions to the six key questions, which inspired the primary design of the new MoC system. The answers to these questions will eventually become the systems of care [14].
Memish et al. (2022) emphasized that the new MoC system is the backbone of the HSTP, which aims to deliver 42 interventions across 6 systems of care while developing clinical guidelines, promoting the use of evidence-based practices, reducing the disparities in care, and promoting accountable care [15].
Trad et al. (2024) illustrated that the new MoC system was designed around six systems of care over multiple layers: keep well, planned care, maternity care, urgent care, chronic care, and end-of-life care [16]. Al Khashan et al. (2021) reported that the new MoC system implements 42 initiatives, 27 of which are divided into six systems of care and 15 overlapping initiatives with different care systems, of which 36 are directly related to PHCCs [17]. Within each system, specific interventions are designed to address concerns and cross-cutting interventions that apply to one or more systems (Table 1) [6].
| System of Care | Definition | Intervention |
|---|---|---|
| Keep Well | The system will support people to stay healthy, get well again, provide them with knowledge, empower them and support them with healthy communities. | 1. Health coach programs 2. Community-based wellness programs 3. Workplace wellness programs 4. School wellness programs 5. Healthy food promotion 6. Health edutainment programs; and 7. Promoting the Saudi Centre for Disease Control. |
| Planned Care | The system will support patients in obtaining an outstanding and consistent outcome of planned procedures, by providing a necessary, efficient and high-quality care. | 8. One-stop clinics 9. Pathway optimization 10.Length of stay reduction initiatives; and 11.Step-down and post-discharge service. |
| Safe Birth | The system will support women in safe delivery and healthy infants. It will provide ongoing support from pre-marriage and pre-conception to postpartum and during the development of the early years. | 12.Premarital screening 13.Preconception care services 14.Maternity care services 15.National birth registry 16.Postnatal care services 17.Well baby clinics 18.Neonatal care services. |
| Urgent Care | The system will support people when they face an urgent problem by providing the necessary treatment in the right place at the right time and supporting the return of patients to their homes and to community services. | 19. A resource control center 20. Urgent care clinics 21. Population-based critical care centers. |
| Chronic Condition | The system will support people in managing their chronic conditions by providing integrated care, facilitating patient flow between care settings and by promoting care at the appropriate setting. | 22. Chronic disease screening 23. Case coordination 24. Continuing care services. |
| Last Phase | The system will support patients and their families during the last stage of their lives. It will provide them with compassionate care and enable them to spend their last days in a place of their choice. | 25. Patient and family support 26. Hospice care services 27. Multidisciplinary team development. |
| Cross-cutting Interventions |
These are interventions integrated into two or more of the Systems of Care to support implementation. | 28. Health in all policies 29. Virtual self-care tools 30. Virtual education and navigation tools 31. Health hotline services 32. Healthy living campaigns 33. School education programs 34. Enhanced primary care services 35. Enhanced home care services 36. Resource optimization 37. Integrated personal health records 38. National referral networks 39. National guidelines 40. Outcomes monitoring 41. Systematic data collection 42. Health research programs. |
1.3. Health Clusters and Implementation of the New MoC System
Al Mubarak et al. (2021) investigated that health clusters in Saudi Arabia are an integrated and interconnected network of health care providers within the framework of a single administrative structure aimed to facilitate beneficiaries’ access to health services; allowing their transfer among several types of care; and granting clear and precise decision rights and benefits, including resource allocation, salaries, and employee evaluations [18].
Haji (2023) indicated that it is important to understand the factors affecting the integration of the new MoC system in the early stage of implementation to ensure appropriate integration routine work of PHCCs to ensure further implementation of the new MoC system and enhanced primary care initiatives [19].
According to (Al-Zahrani et al., 2023), the article aimed to assess the implementation of Team-Based Care (TBC) in primary health care services in Saudi Arabia. Each team consists of at least one family physician, a nurse, a health coach, and a case coordinator. The study recorded good inclusion scores for the health staff included in the TBC model. More than eighty percent of the people surveyed agreed/strongly agreed that participation in the TBC model is a legitimate part of their role and that they are open to working with colleagues in the new approach of the model and continuing to support it. They strongly agree that the feedback on the TBC model may be useful for its future improvement [20]. Sarooji et al. (2024) reported that the TBC is a vital service in primary health care for patients [21].
Alomari et al. (2021) assessed knowledge of the new MoC system among Riyadh First Health Cluster staff at the Ministry of Health, Saudi Arabia. This study aimed to assess knowledge through four dimensions: awareness, understanding, acceptance, and action. They revealed that employees have good knowledge of the new MoC system in Saudi Arabia and a high level of acceptance towards it [22].
2. MATERIALS AND METHODS
2.1. Study Design
A cross-sectional, observational, and analytic study was conducted between October 2023 and December 2023 to assess perceptions of the new MoC system among health care providers in the PHCCs in the Eastern Health Cluster. Various versions of questionnaires were adopted to develop the new version, which was not completely self-developed, as other questionnaires were incorporated.
2.2. Settings
This study targeted health care providers in the PHCCs in the Eastern Health Cluster. The study used an online self-developed questionnaire that was distributed to the target population via official emails and WhatsApp platforms.
2.3. Sample Size and Technique
According to the Human Resources Administration of the Dammam Health Network at Eastern Health Cluster, 1200 health care staff members worked in the Dammam Primary Health Care Centre as of the summer of 2023. With a 95% confidence level, a margin of error of 5%, and the use of the sample size calculator available online at calculator.net, the calculated sample size was 292 health care staff members in Primary Health Care Centers.
2.4. Inclusion Criteria
Health care providers in the PHCCs in the Eastern Health Cluster, both men and women, aged 20 years and above, with at least a 2-year diploma.
2.5. Exclusion Criteria
Health care staff are not working in the PHCCs in the Eastern Health Cluster.
2.6. Data Collection Tools
A questionnaire was developed by the researchers. Different versions of prior questionnaires were adopted to develop the new version, which was therefore not completely self-developed; the other questionnaires used were based on a scientific review of previously published articles. The final online questionnaire that was used in the study had 31 closed-ended questions. The first part of the questionnaire consisted of 5 questions that collected demographic information, such as sex, age, current duties, education level, and years of experience. The second part of the questionnaire consisted of 13 questions that assessed the knowledge and awareness of health care providers in the PHCCs towards the new MoC system in the Eastern Health Cluster. The third part of the questionnaire consisted of 13 questions on health care providers' perceptions of the new MoC system in the Eastern Health Cluster [20, 22].
2.7. Pilot Study
Pilot testing was performed to examine the validity of each question and to identify any ambiguities before the full questionnaire was implemented among 25 individuals, who represented approximately 10% of the target sample. The final version of the questionnaire was reviewed and approved by the research supervisor. The questionnaire was distributed to a sample of health care providers in the PHCCs in the Eastern Health Cluster. The data were collected using an online survey via Google Forms between September and October 2023.
2.8. Validity and Reliability
To validate the questionnaire, the final draft of the questionnaire was reviewed and approved in terms of structure and context by the project supervisor from the Saudi Electronic University. The questionnaire was self-developed from previous literature. Additionally, the questionnaire was pilot tested among 10% of the target sample.
2.9. Data Analysis
Descriptive statistics were calculated, including the frequency, percentage, mean, median, mode, and standard deviation of the data. Statistical analysis was performed by measuring the associations between different variables of interest using the chi-square test. Statistical significance was set at a P value ≤ 0.05. Statistical procedures were performed using Excel and the online statistical calculator mathisfun.com. Additionally, tables and figures were used to present the data.
2.10. Ethical Considerations
This study was approved by the Dammam Medical Complex Institutional Review Board (IRB Protocol No: MNG-02, Date: 12/09/2023, and IRB log No: 44). The invitation page of the questionnaire contains the purpose of the study, contact information of the researcher, and the right to refuse participation or withdraw without any consequences. Therefore, informed consent was obtained from the participants to participate in this study at the beginning of the questionnaires. The confidentiality and privacy of participant data were ensured by keeping participation in the study completely anonymous and written only on the cover page of the questionnaire. Participation in the questionnaire was voluntary, and the participants had the right to refuse participation or withdraw at any time. There was no risk or cost associated with participation in this study. The data were collected anonymously without individual personal information such as names or identification numbers. The data were collected for research purposes only.
3. RESULTS
A total of 157 responses were received; however, 15 were excluded because they did not meet the inclusion criteria, leading to a study population of 142 primary health care staff. The 142 primary health care staff members responded to the questionnaire to assess their perceptions of the new MoC system. The response rate was (48.59%) among males, while the majority were female (51.40%). The response rate for the age group 20–29-year-olds was (33.10%). The majority were from the age group 30–39 years old (47.88%). The response rate for the age group 40–49-year-olds was (16.90%). The minority rate response was for the age group 50–59-year-olds (0.70%). The response rate for the age group 60 years or above was (1.40%). Their current roles included management (30.28%), medical physician (21.83%), nursing (35.91%), allied health (4.92%), and others (7%). The education levels included two-year diploma (30.28%), bachelor's degree (40.14%), master’s degree (21.83%), and PhD degree (7.74%). Participants who had less than 5 years of experience were (22.53%), 5-9 years of experience were (26.76%), 10-14 years of experience (28.87%), 15-19 years of experience (13.38%), and 20 years of experience and above (8.45%). (Table 2).
The first objective of this study was to investigate health care staff's knowledge of the new MoC system, and the results revealed that approximately 46.5% understood all the general concepts of the new MoC system. They knew that the new MoC system introduces 42 initiatives and includes 6 care systems (keep well, safe births, planned care, urgent care, chronic care and last phase), supporting health services from preventive to curative care and ensuring the availability of a comprehensive care system that meets the health needs of the entire population (physical, mental and social well-being) (Fig. 1).
| Demographic Characteristics | Frequencies | % | |
|---|---|---|---|
| Gender | Male | 69 | 48.59% |
| Female | 73 | 51.40% | |
| 20–29-year-old | 47 | 33.10% | |
| 30–39-year-old | 68 | 47.88% | |
| Age | 40–49-year-old | 24 | 16.90% |
| 50–59-year-old | 1 | 0.70% | |
| 60-year-old or above | 2 | 1.40% | |
| Management | 43 | 30.28% | |
| Medical Physician | 31 | 21.83% | |
| Current Job Title | Nursing | 51 | 35.91% |
| Allied Health | 7 | 4.92% | |
| Others | 10 | 7% | |
| Two-years Diploma | 43 | 30.28% | |
| Education Level | Bachelor's Degree | 57 | 40.14% |
| Master's Degree | 31 | 21.83% | |
| PhD Degree | 11 | 7.74% | |
| Less than 5 Years | 32 | 22.53% | |
| 5 - 9 Years | 38 | 26.76% | |
| Years of Experience | 10 - 14 Years | 41 | 28.87% |
| 15 - 19 Years | 19 | 13.38% | |
| 20 Years and above | 12 | 8.45% | |
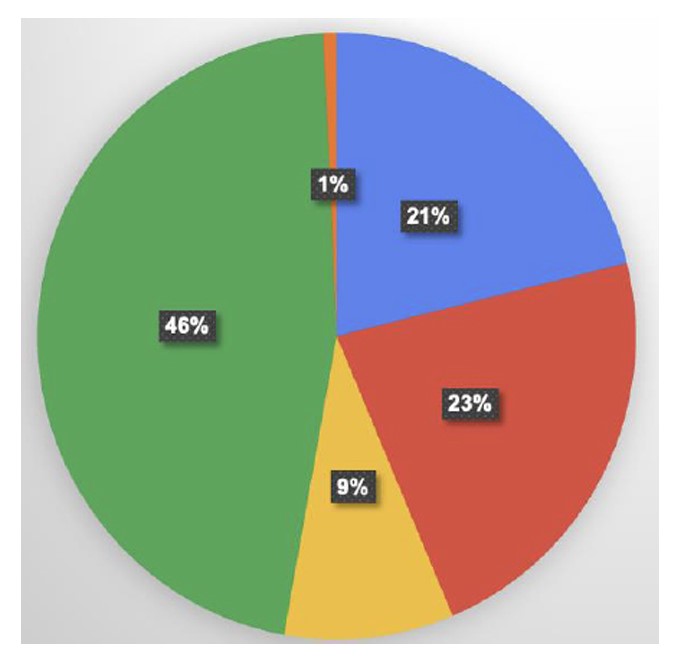
Note: 21% Ensure the availability of a comprehensive care system that meets the health needs of the entire population (physical, mental, and social well-being). 23% Supporting the provision of all health services from preventive to curative care. 9% The New Models of Care system will deliver 42 initiatives that will integrate with six systems of care (Keep Well, Safe Birth, Planned Care, Urgent Care, Chronic care and the last phase). 46% are all. 1% None of the above
The second objective of this study assessed health care staff in terms of awareness and implementation of the new MoC system. The percentage of knowledge of the implementation of the new MoC system in the PHCCs and the continuous training necessary for health care workers reached (87.32%). A (76.76%) of participants acknowledged that the workplace arranged for conferences, speeches, or meetings related to the new MoC system, with a significant P value (<0.006) (Table 3).
| General knowledge and awareness of the New Model of Care System | Yes | No | Maybe |
|---|---|---|---|
| Application of the New Model of Care system in Primary Health Care Centers | 124 (87.32%) | 4 (2.81%) | 14 (9.85 %) |
| Familiarity of New Model of Care system | 132 (92.95%) | 5 (3.52%) | 5 (3.52%) |
| Familiarity of New Model of Care guidelines | 115 (80.98%) | 12 (8.45%) | 15 (10.56%) |
| Workplace arrangements for conferences, speeches, or meetings related to New Mode of Care System updates | 109 (76.76%) | 17 (11.97%) | 16 (11.26%) |
| Familiarity of New Model of Care System pathways | 115 (80.98%) | 16 (11.26%) | 11 (7.74%) |
| Continuous training in the New Model of Care system necessary for health care staff | 124 (87.32%) | 9 (6.33%) | 9 (6.33%) |
| Overall Fit Value | Chi- square = 24.6181; DF = 10; P-value = 0.006118 | ||
| Familiarity of specific New Model of Care pathways | Yes | No | Maybe | P-value |
|---|---|---|---|---|
| Keep Well pathway | 120 (84.50%) | 12 (8.45%) | 10 (7.04%) | 0.9628 |
| Planned Care pathway | 120 (84.50%) | 13 (9.15%) | 9 (6.33%) | 0.759 |
| Safe Birth pathway | 123 (86.61%) | 9 (6.33%) | 10 (7.04%) | 0.7099 |
| Urgent Care pathway | 127 (89.43%) | 7 (4.92%) | 8 (5.63%) | 0.2051 |
| Chronic Care pathway | 123 (86.61%) | 10 (7.04%) | 9 (6.33%) | 0.7689 |
| Last Phase pathway | 108 (76.05%) | 17 (11.97%) | 17 (11.97%) | 0.007802 |
| Items | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| The New Model of Care System will increase access to healthcare services. | 65 (45.77 %) | 55 (38.73%) | 17 (11.97%) | 4 (2.81%) | 1 (0.70%) |
| The New Model of Care System will improve the quality of care. | 49 (34.50%) | 68 (47.88) | 18 (12.67%) | 6 (4.22%) | 1 (0.70%) |
| The New Model of Care System will reduce patients’ waiting time. | 47 (33.09 %) | 51 (35.91%) | 33 (23.23%) | 9 (6.33%) | 2 (1.40%) |
| The New Model of Care System will reduce the cost of health services. | 54 (38.02 %) | 54 (38.08%) | 24 (16.90%) | 8 (5.63%) | 2 (1.40%) |
| The New Model of Care System will help individuals to be proactive and aware of their own health. | 45(31.69 %) | 66 (46.47%) | 24 (16.90%) | 5 (3.52%) | 2 (1.40%) |
| The New Model of Care System will help in early detection of diseases. | 61 (42.95 %) | 52 (36.61 %) | 22 (15.49 %) | 3 (2.11 %) | 4 (2.81%) |
| The New Model of Care System will improve patient health. | 54 (38.02 %) | 57 (40.14 %) | 26 (18.30 %) | 4 (2.81%) | 1 (0.70%) |
| The New Model of Care System will connect the Primary Health Care Centers ,Specialized Clinics, and the Hospitals together. | 53 (37.32 %) | 59 (41.54 %) | 21 (14.78%) | 5 (3.52%) | 4 (2.81%) |
| The New Model of Care System has a clear guideline that allows the healthcare provider to track the patient’s condition through the care coordinator. | 41 (28.87 %) | 61 (42.95 %) | 29 (20.42%) | 9 (6.33%) | 1 (0.70%) |
| The New Model of Care System provides staff with information they need to provide appropriate patients care. | 43 (30.28%) | 63 (44.36%) | 29 (20.42%) | 6 (4.22%) | 1 (0.70%) |
| The implementation of the New Model of Care System is appropriate to the current conditions in Primary Health Care Centers. | 49 (34.50 %) | 57 (40.14 %) | 20 (14.08 %) | 15 (10.56%) | 1 (0.70%) |
| I think that I am willing to implement the New Model of Care System. | 44 (30.98 %) | 67 (47.18 %) | 24 (16.90%) | 5 (3.52%) | 2 (1.40%) |
| The New Model of Care systems can be integrated into existing systems. | 39 (27.46 %) | 65 (45.77 %) | 24 (16.90%) | 7 (4.92%) | 7 (4.92%) |
| Overall Fit Value | Chi-square = 60.4783 ; DF =44 ; P-value = 0.05 | ||||
Moreover, this study assessed familiarity with the new MoC system pathway, as presented in Table 4, and revealed that each of the six systems of care (keep well, planned care, safe births, urgent care, chronic care, and last phase) was not significant, except for the last phase pathway. The majority of health care staff responded to the following question: “Are you familiar with the new MoC pathway?”, with the most “yes” responses for the urgent care pathway (89.43%), safe birth pathway (86.61%), and chronic care pathway (86.61%).
The results of the questions assessed primary health care staff perceptions of the new MoC system indicated that (45.77%) would increase access to healthcare services, followed by helping in early detection of diseases (42.95%) and improving patient health (38.02%).
Many were willing to implement the new MoC system (47.18%), with a significant P value (<0.05) (Table 5).
4. DISCUSSION
This study assessed perceptions of the new MoC system among health care providers in PHCCs in the Eastern Health Cluster. The majority of participants had a high level of knowledge of most aspects of the concept of the new MoC system, while some only knew about one part. These findings indicate that health care staff need to be more aware of and intensify their knowledge of all goals and what they aim to provide. The results of this study revealed that 46.5% of the participants understood the general concept. The percentage of respondents who understood only one goal support for health services from preventive to curative care was 22,53%.; 21,12% of the participants knew the goal of ensuring the availability of a comprehensive care system that met the health needs of the entire population (physical, mental and social well-being); and 9,15% of the participants knew that it introduces 42 initiatives and includes 6 care systems (keep well, safe births, planned care, urgent care, chronic care, and last phase). One percent of the participants did not know of the initiative. These results are consistent with those of (Alomari et al., 2021), who demonstrated that when the participants’ knowledge was assessed, the majority understood the general concept of the new MoC system, while some understood only one part of the system, and (1,7%) of the participants had no knowledge [22].
This study assessed health care staff in terms of general knowledge and awareness of the new MoC system, and the results revealed that the majority of respondents answered “yes”. The percentage of implementation in the PHCCs and continuous training necessary for health care workers reached 87.32%, familiarity with the new MoC system was 92.95%, familiarity with the guidelines was 80.98%, familiarity with the pathways was 80.98%, and the 76.76% of respondents answered yes when we asked whether workplace arrangements for conferences, speeches or meetings were related to updating the new MoC system. These results indicate that primary health care staff have high levels of knowledge and awareness of the new MoC system. These findings are consistent with those of (Alomari et al., 2021), who found that participants had a high level of knowledge and acceptance of the system and that it would have a positive effect on their careers [22]. Haji (2023) emphasized that it is important to understand the factors affecting the integration of the new MoC system in the early stage of implementation to ensure appropriate integration of this new intervention into the routine work of PHCCs, ensuring further implementation of the new MoC system and enhanced primary care initiatives [19].
This study assessed the familiarity of pathways; the highest percentage of primary health care staff were aware of the urgent care, chronic care, and safe birth pathways, while one of the pathways of which they were least aware was the last phase care pathway. Jey et al. (2024) highlighted that the ongoing education and professional development help close knowledge gaps, strengthen multidisciplinary collaboration, and ensure patient-centered care that improves the quality of life for patients and their families [23]. These results are consistent with those of (Alomari et al., 2021), who reported that the “last phase” system represented the lowest percentage of awareness among PHCCs [22]. The highest percentage of awareness of “keep well” was in hospitals, whereas the lowest rate of awareness was in PHCCS. The highest percentage of awareness of the “planned care” system was among the PHCCs.
This study assessed primary health care staff perceptions of the new MoC system and their perspectives on the potential to connect the different areas of the health care sector and improve workflow pathways. The participants agreed that the system would connect the PHCCs, specialized clinics, and hospitals together (37.32%), have clear guidelines that allow the health care provider to track the patient’s condition through the care coordinator (28.87%), and provide staff with information they need to provide appropriate patient care (30.28%). The implementation of the new MoC system is appropriate for the current conditions in PHCCs (34.50%). These results are consistent with those of (Yousef et al., 2023). The implementation of the new MoC system improved data management, collection, and visualization, and enhanced patient and community engagement [24].
With respect to the role of the new MoC system in health care transformation from the perspective of primary healthcare staff, the research found that most of the participants agreed that the system would increase access to health care services (45.77%), improve the quality of care (34.50%), and reduce patient waiting time (33.09%). According to the article by (Chowdhury et al., 2021), the new MoC system is an important focal point for enhancing the value placed on personalized care for individuals by improving treatment methods and the care provided [14]. Moreover, according to (Haji, 2023), the article will target the continuous improvement of health services by focusing on beneficiaries' experience and satisfaction in line with international standards and best practices [19].
In this study, most of the participants agreed that the new MoC system would reduce the cost of health services (38.02%), help individuals be proactive and aware of their own health (31.69%), help in the early detection of diseases (42.95%), and improve patient health (38.02%). These results are consistent with those of (Aldhamin et al., 2023), who reported positive outcomes in patients who were overweight at the Eastern Health Cluster in Saudi Arabia. Under the keep well pathway, the Health Coach Program targets several behaviour-related issues, such as smoking, anxiety, unhealthy diet, and physical inactivity. They reported a statistically significant difference between the initial and final weights. The percentage change in weight was found to be approximately -3% kg, with more than a quarter of participants achieving at least a 5% weight loss after 12 to 26 weeks of the health coaching program [25].
When primary health care staff were asked if they were willing to implement the new MoC system and if it could be integrated into existing systems, this study revealed that participants strongly agreed that they were willing to implement it and that it could be integrated into existing systems. Similarly, (Al-Zahrani et al., 2023) reported good inclusion scores for the health staff included in the TBC model. More than eighty percent of the people surveyed agreed/strongly agreed that participation in the TBC model is a legitimate part of their role and are open to working with colleagues in the new model and continuing to support it. They strongly agree that the feedback on the TBC model may be useful for its future improvement [20].
In conclusion, when assessing the perceptions of primary health care staff in the Eastern Health Cluster, this study revealed that they have knowledge and awareness of the new model and that they are familiar with the system and its pathways, which is consistent with the findings of a previous study conducted in a similar field.
5. STRENGTH(S) AND LIMITATION(S)
The limitation of the current study was the study design. A cross-sectional design can lead to biased data and make it more difficult to investigate causal relationships. Another limitation of this study was its geographical nature. This study was conducted in one region, the Eastern Health Cluster. It did not represent all primary health care staff. This may limit the generalizability of the findings to a wider range of health care providers. Additionally, the study sample was smaller than the minimum targeted sample size calculated. Despite these limitations, this research has several strengths. This study is among the few conducted in the Eastern Health Cluster that explored primary health care staff's knowledge and perceptions of the new MoC system. In this study, primary health care staff were assessed because they are the first health care providers patients see, underscoring the importance of understanding their readiness, knowledge, perceptions, and practices regarding the new MoC system.
CONCLUSION
This research revealed that primary health care staff have high levels of knowledge and awareness of the new MoC system, pathways, and guidelines. The greatest awareness was of the urgent, chronic, and safe birth pathways, while one of the lowest percentages of awareness was of the last phase pathway. Most of the participants agreed that the system would connect different areas of the health sector together and provide staff with the necessary information. Most of the participants agreed that the new MoC system would increase access to health care services, improve the quality of care, and reduce patient waiting time, which are the aims of health care transformation. Finally, most of the participants agreed that the new MoC system would reduce the cost of health services, help individuals be proactive and aware of their own health, help in the early detection of diseases, and improve patient health. This study highlighted the importance of targeted training and continuous professional development to ensure full comprehension and effective implementation of all pathways. These insights provide valuable information for stakeholders in planning and scaling interventions across the health care system.
RECOMMENDATION
Future studies could be conducted in another geographical region in Saudi Arabia where the same system is applied. Furthermore, demographic details would be valuable to investigate regarding knowledge, awareness, and familiarity with the new model.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: S.S.A: Study conception and design; B.A.B.: Research supervision, academic guidance, regular feedback, manuscript review, and final approval; A.A.B.: Final review, validation of content, accuracy check, and ensuring consistency with standards. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| MoC | = Model of Care |
| HSTP | = Health Sector Transformation Program |
| TBC | = Team-Based Care |
| PHCCs | = Primary Health Care Centers |
| SoC | = Systems of Care |
| MOH | = Ministry of Health |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Dammam Medical Complex Institutional Review Board (IRB Protocol No: MNG-02, Date: 12/09/2023, and IRB log No: 44), Saudi Arabia.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the participants to participate in this study.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
ACKNOWLEDGEMENTS
Declared none.


