All published articles of this journal are available on ScienceDirect.
Ciprofloxacin Resistant Salmonella Typhi Isolated at National Microbiology Reference Laboratory in Harare, Zimbabwe (January to April 2016)
Abstract
Background:
Typhoid is a life-threatening infectious disease requiring the administration of antibiotics for treatment. Ciprofloxacin is the antibiotic of choice for diarrheal cases in Zimbabwe, adopted by the Ministry of Health and Child Care, from current World Health Organisation (WHO) guidelines. However, there has been an increase in the emergence and spread of multidrug resistance against ciprofloxacin and conventional drugs antibiotics for the treatment of typhoid.
Objective:
This cross-sectional study aimed to determine the prevalence of ciprofloxacin-resistant Salmonella Typhi (S. Typhi) isolated in Harare for the first quarter of 2016.
Methods:
This study was carried out at the National Microbiology Reference Laboratory (NMRL), located at Harare Central Hospital, in Zimbabwe. The NMRL carries out confirmatory tests and molecular typing of pathogens isolated at different national laboratories. The current study retrieved demographics, clinical data, and isolates for confirmed typhoid cases out of 402 suspected specimens. The isolates from Harare, confirmed as S. Typhi, between January and April 2016, were evaluated for ciprofloxacin resistance.
Results:
A total of 35 S. Typhi isolates were recovered for the period from January to April 2016. When the 35 isolates were characterised, nine (25.7%) were resistant to ciprofloxacin. The area with the highest recorded cases of typhoid fever was Budiriro High-Density Suburb in Harare. This area has been hit by other diarrheal outbreaks in the past, most likely due to the intermittent supply of safe water.
Conclusion:
Most high-density areas, where S. Typhi positive specimens originated, are overpopulated and have regular water cuts, resulting in a decrease in hygiene. More than a quarter of isolates are resistant to ciprofloxacin, agreeing with other reports from Zimbabwe. The misuse of antibiotics could be associated with resistance, necessitating education on the correct use of antibiotics in the community and other preventive measures. Additionally, molecular research on geographic and phylogenetic relatedness of isolates and other holistic approaches for studying the development of antimicrobial resistance mutations, using whole-genome sequencing, in this setting, are warranted.
1. INTRODUCTION
Salmonella Typhi (S. Typhi) causes typhoid fever, a major public health problem in developing countries [1, 2]. Typhoid fever is common in areas where safe drinking water and sanitation are inadequate. More than 16 million new cases occur worldwide annually, resulting in approximately 600,000 deaths per year [1, 3]. The disease has been a major human pathogen for thousands of years, thriving in conditions of poor sanitation, crowding, and social chaos [3-5]. Typhoid is transmitted mainly by the faecal-oral route [6, 7]. In most cases, an asymptomatic carrier of S. Typhi, or an individual who has recently recovered from the infection, continues to excrete large number of organisms in the stool for up to three months and contaminates food or water, either through direct food handling, through transfer of bacteria by flies and other insects, or by contamination of potable water [8-10]. About 2-3% of patients are permanent carriers [11].
S. Typhi is a gram-negative enteric bacillus, a member of Enterobacteriaceae: ferments glucose, reduces nitrate, and is oxidative negative [12]. This facultatively anaerobic bacillus possesses three major antigens: H or flagellar antigen; O or somatic antigen; and Vi or virulence antigen. Clinical diagnosis of typhoid is confirmed by culture of the organism from blood, duodenal secretions, or stool [4, 13]. Excretion of S. Typhi in the stool is more likely with higher blood bacterial counts, and children tend to have higher bacteraemia than adults [14]. Fluoroquinolones such as ciprofloxacin are recommended by the World Health Organisation (WHO) as they are the most effective orally active, inexpensive, and well-tolerated drugs for the treatment of typhoid fever [15]. Ciprofloxacin is the current first drug of choice for diarrheal cases in Zimbabwe according to the Ministry of Health and Child Care guidelines [16].
S. Typhi has gained resistance to antibiotics like ampicillin, ceftriaxone, and co-trimoxazole, besides developing resistance to efficacious drugs like ciprofloxacin. The emergence of multidrug resistance to the commonly used antibiotics has complicated the treatment [17, 18]. The pathogenesis of S. Typhi depends upon a large number of factors controlled by arrays of genes that synergise into actual virulence of the bacteria [19, 20].
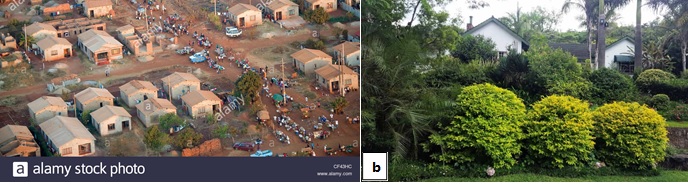
In the case of Harare, Zimbabwe, the city experienced a rise in cases of typhoid fever in Mabvuku and Tafara, both high-density suburbs, in January 2010. From October 2011 to June 2012, there was another typhoid outbreak, whose epicentre was the Harare high-density township of Dzivarasekwa [21, 22]. Such high-density areas of Zimbabwe typically comprise crowded households with high numbers of people (Fig. 1a) while low-density areas are more affluent and less crowded (Fig. 1b). There were unsubstantiated reports of another typhoid outbreak in parts of Harare in the first quarter of 2016, which is the subject of our current study. Hence this study was carried out to determine ciprofloxacin resistance of S. Typhi isolated at the National Microbiology Reference Laboratory (NMRL) in Harare, Zimbabwe between January and April 2016.
2. METHODS
This cross-sectional study was conducted after permission by the Harare Hospital’s Clinical Director and ethical approval from Africa University Research Ethics Committee (AUREC). The study was carried out at the National Microbiology Reference Laboratory (NMRL), located at Harare Central Hospital in Zimbabwe. NMRL receives stool or blood specimens from medical facilities located all over Zimbabwe and provides confirmatory and biochemical typing of pathogenic isolates. Upon receipt, stool and blood samples from Harare laboratories were cultured on Blood Agar (BA) or deoxycholate Citrate Agar (DCA), as appropriate. Kligler Iron Agar (KIA) and Lysine Iron Agar (LIA) were then used for presumptive identification and isolates were further screened using Vi and D slide serology (Fig. 2a).
Demographics and clinical data recovered from Harare patients suspected to be suffering from typhoid were noted. Isolates from stool and blood samples, for the confirmed cases, received during the period from January 2016 to April 2016, were retrieved. The Mueller–Hinton agar disk diffusion method was subsequently used to determine antimicrobial susceptibility profiles of the 35 confirmed S. Typhi isolates against ciprofloxacin (Fig.2b). Results were interpreted according to Clinical and Laboratory Standards guidelines (Table 1).

3. RESULTS
All isolates came from blood or stool cultures of 402 diarrheal cases from Harare Health facilities. In this study, 41 isolates reacted positively with Kligler iron agar, lysine iron agar, and were citrate negative, which is suggestive of S. Typhi. The Salmonella antisera Poly H, Poly O, Monofactor 9, 12, Vi, and dH reacted positively with 35 of the 41 isolates, confirming their identity as S. Typhi. The location of origin for the different samples and the numbers of confirmed S. Typhi isolates per site is shown in Table 2.
Most of the areas with positive cases of S. Typhi are high-density areas. Only two (6%) of the cases were from low-density suburbs (Eastview and Greendale). Thirty-five isolates out of 402 suspected and tested specimens in this study reacted positively with Salmonella Antisera (Poly H, poly O, Monofactor 9,12, Vi, and dH) which confirms their identity as S. Typhi. For the confirmed S. Typhi, resistance to cipro-floxacin was observed in a quarter of isolates (Table 1).
4. DISCUSSION
Most high-density areas, where S. Typhi positive specimens originated are overpopulated and have regular water cuts resulting in a decrease in hygiene [21, 22]. Over 25% of S. Typhi isolates characterised are resistant to ciprofloxacin. Our results agree with overall trends reported prior to this account, with an increase in resistance to ciprofloxacin from 0% in 2012, 25% in 2015 to 22% in 2017 [23]. The reason for the increase in ciprofloxacin resistance in Zimbabwe may be its over-use as a broad-spectrum antibiotic to treat many infectious diseases [23, 24]. Though fluoroquinolone resistance is chromosomally mediated, selective pressures exerted by the overuse of these drugs may see such isolates becoming more common in the future [24].
A similar increase in resistance has been observed in many countries around the world. A study on S. Typhi isolates in the United Kingdom discovered a decrease in susceptibility to ciprofloxacin to 23%, in 1999 [25]. Other studies recommended that possible alternative drugs to treat ciprofloxacin-resistant S. Typhi such as ceftriaxone or cefotaxime could be considered in the treatment and management of typhoid fever [26]. The decrease in ciprofloxacin susceptibility was also observed in Cambodian adults [27]. In another research done in South Africa, 18% of the isolates were resistant to ciprofloxacin [28]. A similar trend was observed on 70 isolates in Bangladesh [29]. The resistance of S. Typhi is mainly due to the accumulation of mutation in the quinolone resistance- determining regions of DNA gyrase and topoisomerase IV genes which are target site alterations [30].
Plasmid-mediated quinolone resistance confers a form of reduced susceptibility, which is thought to promote the accumulation of the target site mutation [31]. The increased resistance of S. Typhi could reflect the overuse of ciprofloxacin in the treatment of typhoid as well as in other unrelated infections. Incomplete treatment may also be a contributing factor to the development of resistance [23, 26, 32]. This might be the reason why there is a high proportion of ciprofloxacin-resistant isolates in the areas studied. In addition, an increase in antimicrobial resistance has been attributed to the selection pressure created by the uncontrolled use of antimicrobials in animal husbandry. The lack of strict control on antimicrobial usage increases the risk of dissemination of foodborne microbes harbouring arrays of resistance genes [33].
Questions still remain regarding the origin of antimicro-bial-resistant mutations and transmission routes of antimicro-bial-resistant pathogens across populations. Antimicrobial resistance monitoring by bacterial whole-genome and 16S ribosomal RNA sequencing is a rapidly growing field and it is reported that such methods are likely to impact public health [34]. This is because molecular research and environmental metagenomics are more holistic approaches for studying the development of antimicrobial resistance mutations. Hence, metagenomic profiles could aid the prediction of antimicrobial resistance from clinical specimens. By leveraging information collected in this field, it is possible to characterize the “resistome” in human samples, from diverse geographical regions.
| Disk potency | Diameter (zone of inhibition) | ||
|---|---|---|---|
| 5μg | >31mm | 21-30mm | <20mm |
| Interpretation | Susceptible (S) | Intermediate (I) | Resistant (R) |
| Geographic distribution of isolates | Sensitivity patterns | ||||
|---|---|---|---|---|---|
| Area | Number | Proportion (%) | Sensitive | Intermediate | Resistant |
| Budiriro HD | 12 | 34.3 | 4 | 3 | 5 |
| Eastview LD | 1 | 2.9 | 1 | - | - |
| Glen Norah HD | 2 | 5.7 | 1 | 1 | - |
| Glenview HD | 9 | 25.7 | 3 | 4 | 2 |
| Greendale LD | 1 | 2.9 | 1 | - | - |
| Hatcliffe HD | 1 | 2.9 | - | - | 1 |
| Hopley HD | 2 | 5.7 | 2 | - | - |
| Kuwadzana HD | 1 | 2.9 | - | - | 1 |
| Mufakose HD | 2 | 5.7 | 1 | 1 | - |
| Tafara HD | 1 | 2.9 | - | 1 | - |
| Warren Park HD | 3 | 8.6 | 3 | - | - |
| Total | 35 | 100.0 | 16 (45.7%) | 10 (28.6%) | 9 (25.7%) |
CONCLUSION
The rise in antimicrobial resistance to the first-line drug used for typhoid treatment in Zimbabwe implies that the drug should be used with due care. According to the ciprofloxacin susceptibility patterns of S. Typhi isolated, antimicrobial resistance must be monitored regularly in order to check effective drug use. When a strain of microorganism acquires resistance to a drug, another drug must be found to treat the resistant infection effectively. Drugs like ceftriaxone and nalidixic acid should be considered for the treatment of typhoid as they are less commonly used in the population and no resistance has been documented. New antibiotics also need to be developed to deal with the global problem of antimicrobial drug resistance. The WHO and the Drugs for Neglected Diseases Initiative (DNDi) are working in collaboration on a partnership to develop novel antibiotics, as well as promoting their responsible use and ensuring equitable access [35].
RECOMMENDATIONS
Larger research involving national data over longer periods of time should be carried out. Whole-genome sequencing to determine the presence of the virulent genes capable of cell invasion and infection, sequencing to check the DNA gyrase mutation, antimicrobial sensitivity assays to monitor first-, second- and third-line drugs and evidence-based vaccination programs for typhoid prophylaxis should be introduced. The global problem of antimicrobial resistance needs to be understood through the use of novel methods, for example designing new drugs informed by genotypic relatedness and geographic and phylogenetic relationships of isolates.
LIMITATIONS OF STUDY
There was a limited number of isolates encountered during the period of study and limited resources to investigate the virulent genes. It is recommended that more focus be given to genotyping methods when studying the development of antimicrobial resistance mutations.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval was obtained from Africa University Research Ethics Committee (AUREC), Zimbabwe with approval number AU452/16.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Permission to access the data and materials were granted by the National Microbiology Reference Laboratory, Zimbabwe to Ndatenda Mutaurwa. Access to the data was for undergraduate training purposes and cannot be publicly shared.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors acknowledge National Microbiology Reference Laboratory, Zimbabwe.


