All published articles of this journal are available on ScienceDirect.
How Much Do We Know? Assessing Public Knowledge, Awareness, Impact, and Awareness Guidelines for Epilepsy: A Systematic Review
Abstract
Background:
Epilepsy misconceptions are widespread; these influence the quality of life of people living with epilepsy (50 million people worldwide) and their families.
Objective:
The review’s objective was to highlight the public knowledge and awareness of epilepsy with an emphasis on its impact, gaps, and available guidelines for public awareness.
Methods:
The search databases included PubMed, EBSCOhost, Google Scholar using keywords, index terms as well as the Boolean search. Twenty-seven studies were included, which yielded three themes and six sub-themes.
Results:
Three themes emerged from the data: knowledge, beliefs, and awareness of epilepsy, the impact of epilepsy, and epilepsy awareness guide. From these themes, six sub-themes were established.
Implications:
Generally, people in Africa continue to hold misconceptions about epilepsy. This study shows that there is a need for further research examining the level of knowledge and awareness held in different contexts to develop a means to educate the general public as it has been revealed that there is generally inadequate knowledge and awareness of epilepsy. Furthermore, this study gathers knowledge that is now accessible as a threshold to much-needed research on epilepsy education, awareness and knowledge in Africa.
1. INTRODUCTION
Epilepsy is a common neurological disorder worldwide. It affects over 50 million people irrespective of age, nationality, and ethnicity [1]. It is expected that this number increases along with life expectancy, making this a constantly increasing global crisis. Epilepsy has been claimed to be the fourth greatest common neurological disorder [2]. World Health Organization statistics show that 7.6 in 1000 persons have had epilepsy at a point in their lives [3]. In Africa alone, 10 million people live with epilepsy, and 1 in every 100 people are affected with epilepsy in South Africa, which adds up to more than a million people per South Africa’s estimated population [4, 5].
The prevalence of epilepsy needs increasing attention from the authors, researchers, health practitioners, and worldwide health institutions to prioritize and invest in its treatment, management, and public awareness. To emphasize its significance, the World Health Assembly in 2018 drew policymakers’ attention to incorporate epilepsy with non-communicable diseases and mental health [3]. In the past, there has been a preoccupation with one aspect of epilepsy, thus the focus was on control of seizures. This focus resulted in neglecting the disorder’s social, contextual, and culturally congruent impact as well as its knowledge, which mostly comes from ideas held by the general public. It should be indicated that there are social, contextual, and cultural effects that vary from country to country, and the stigma and discrimination that surround epilepsy worldwide seem to be often more problematic to deal with than the seizures themselves [6]. People living with epilepsy can be subjected to being targets of prejudice and alienation [6, 7]. The stigma attached to epilepsy had been marked to discourage people from seeking treatment for symptoms as well as to avoid being identified with or attached to the disease [6].
Misconceptions about epilepsy present the absence of factual knowledge on epilepsy. In Sub-Saharan Africa, misconceptions related to epilepsy are prevalent, resulting in poor public knowledge of epilepsy [8, 9]. Furthermore, the level of knowledge is subject to an economic and societal status, indicating that people in urban areas respond more positively and accurately to tests on knowledge and awareness of epilepsy as compared to those residing in rural areas [9, 10]. Most people have little knowledge about epilepsy as well as negative attitudes toward epilepsy [11]. However, amongst the general public, levels of knowledge are reported to be moderate in countries such as Ethiopia [12]. We find that though there may be insufficient knowledge on epilepsy, within Sub-Saharan Africa, individuals who are not living with epilepsy have a positive attitude toward people living with epilepsy [8]. Additionally, attitudes toward people living with epilepsy have also been reported to be gender-specific as well as based on a strong hold of unfavourable attitudes towards epilepsy itself [10].
However, the authors found that the investment in public health education and management is evident mostly in developed countries such as the United States of America (USA) and Europe, where funding for public campaigns and extensive research is easily accessible. It is only recently that African countries such as Nigeria, Ghana, and Egypt have begun exploring the knowledge and impact of epilepsy to disregard cultural and religious misconceptions and restore the quality of life for people living with epilepsy. After careful assessment, the Institute of Medicine (IOM) in Nepal studied regarding public knowledge and awareness of epilepsy and concluded that the public lacks elementary knowledge about epilepsy and seizures [2]. The IOM conducted their study in the United States of America as to find out how much more knowledge would be required on epilepsy in undeveloped and developing countries?
1.1. Understanding Epilepsy
Epilepsy has been defined and understood in different ways pertaining to era/period, religious beliefs, and level of exposure to scientific knowledge. Culture has a strong influence on the way people understand epilepsy and religious factors also impact the understanding and interaction with the disease [13, 14]. It is relevantly clear that people attain information about epilepsy from several different sources, including (but not limited to) the internet, family, social media, entertainment, media, and friends. These are just some of the ways that the general public filters their understanding of epilepsy. The public idea of what the disorder is, what causes it, and how it can be treated/managed/cured has been mostly a misrepresentation of the disorder.
Misconceptions on epilepsy persisted until the 17th and 18th centuries when European neurologists certified epilepsy to be a brain disorder and further scientifically defined it as an occasional disorder that involves the discharge of grey matter from nerve tissue on muscles resulting in altered sensations, behaviour, and consciousness. Since then, more definitions have immerged expanding the scientific explanation of the disorder. Epilepsy has also been defined as a condition that is characterized by experiencing unprovoked seizures caused by synchronous or excessive neural activity [2]. Additionally, epilepsy is characterized by an enduring predisposition to seizures and results in neurobiological cognitive, psychological, and social consequences [2, 14, 15]. The definition of epilepsy is one amongst several misconceptions that people often hold concerning the disorder. These misconceptions are important to know and understand to develop culturally relevant interventions and awareness programs, as suggested by Mbelesso et al. [16]. This review aims to highlight the public knowledge and awareness of epilepsy with an emphasis on its impact, gaps, and available guidelines for public awareness.
2. METHODS
2.1. Search Strategy
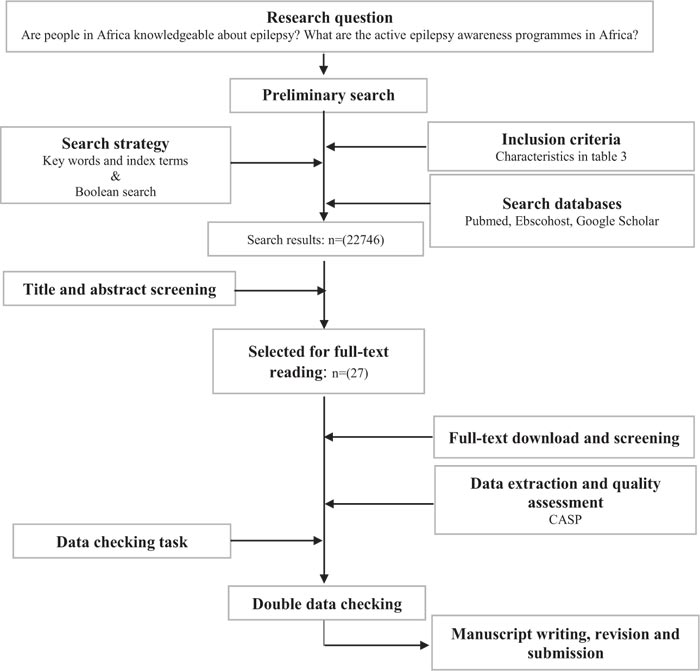
The guideline for conducting a systematic review has been adapted for this review, as shown in Fig. (1) [17]. The researchers used the keywords and conducted a search on titles and abstracts within the article. In addition, the Boolean search was also adapted, wherein researchers combined different search terms. Index terms, which considered the article content to find similar terms, were also used to search available literature. Search words like epilepsy, public awareness, public knowledge, education, guidelines, programs, epilepsy awareness, epilepsy knowledge, the impact of epilepsy, and awareness guidelines were used as represented in Table 1.
The systematic review guide by Tawfik et al. [17] was adopted, modified and some steps from the guide have been excluded as methods did not coincide with the nature of the study. The search databases included PubMed, EBSCOhost (incl. CINAHL; Academic Search Complete; MEDLINE; Psych INFO; Health Resource- Nursing/academic edition), and Google Scholar. The selection of the three (3) databases provided a wide range of medical journals. Furthermore, the EBSCOhost encompassed within it other sub-databases which added more value to the search. The search databases and keywords for the review are indicated in Table 1.
| Database | Key search words |
| PubMed, Ebscohost, and Google Scholar | Epilepsy, public awareness, public knowledge, education, guidelines, programs, epilepsy awareness guidelines and programs, epilepsy awareness, epilepsy knowledge, the impact of epilepsy, and awareness guidelines. |
2.2. Study Inclusion and Exclusion Criteria
A time-based search was done only including publications from 2014-2020. Studies conducted globally and only those reported in English have been included. These studies were found to be concentrating on either public knowledge of epilepsy, the impact of epilepsy and prescribed guidelines for the epilepsy awareness program. The review excluded data focusing on epilepsy treatment/management, professional knowledge (health workers, teachers/educators, and medical students) and diagnosis.
2.3. Study Selection
Several research studies have been found to be conducted on the knowledge and public and professional practitioners’ awareness of epilepsy as well as its treatment. To select relevant studies for this systematic review, the authors reviewed the topics and abstracts of the search results of all studies before independently reading through articles and documents to ensure relevance. This process is presented in Fig. (2) as a PRISMA flow chart which gives the summary of the study sampling process. Fig. (2) shows the study selection process within the review, data obtained, as well as inclusion and exclusion criteria of the study.
Prisma is a scientific method of accumulating transparent knowledge of items in a systematic review. The Prisma flow chart presented in Fig. (2) has been adapted from Liberati et al. [18]. Prisma is a four-phased diagram that summarises a checklist to ensure clear reporting of data. The overall search provided 2274 studies. After title and abstract review, 2216 studies were excluded from full-text screening. Studies excluded were studies whose topics did not coincide with the study aim, studies on epilepsy management, epilepsy treatment and practices regarding epilepsy. The remainder of the studies to be read in full were 27, from which 22 studies were found to be relevant to the study pertaining to the purpose of the study. However, the included studies were also critically analysed for reliability.
2.4. Appraisal of Included Studies using CASP
The Critical Appraisal Skills Programme is a tool to resolve the quality of the included studies [19]. The program provides a standardized checklist from which the weaknesses and strengths of the study can be identified. This assisted in assessing the relevance, validity, and reliability or trustworthiness of the data included in this current study. The authors used the CASP checklist to critically assess and appraise the included studies. For each study, the following questions were answered: are the results of the study valid, what are the results of the study, and will the results be applied locally? The total score out of 10 was then converted to percentages (from the highest to the lowest) ranging from 55% to 95%, as indicated in Table 2, based on how the authors scored the study with respect to each of these questions. According to the authors, the higher the score, the more valid the study is, and the lower the score, the less valid the study is.

| Study author(s) | Title | Design | % |
| Al-Dossari et al. [20] | Public knowledge awareness and attitudes toward epilepsy in Al-Kharj Governorate Saudi Arabia. | Cross-sectional study | 77% |
| Armah-Ansah et al. [21] | Population and Health Students Knowledge, Attitude and Perception towards Epilepsy Patients | Cross-sectional study | 76% |
| Benson et al [22]. | The stigma experiences and perceptions of families living with epilepsy: Implications for epilepsy-related communication within and external to the family unit. | Sequential exploratory design | 92% |
| Braga et al. [23] | Education and epilepsy: Examples of good practice and cooperation. Report of the IBE Commission on Education | Literature Review | 66% |
| England et al. [2] | Erasing Epilepsy Stigma: Eight Key Messages | Commentary | 70% |
| Fekadu et al. [24] | Community’s Perception and Attitude towards People with Epilepsy in Ethiopia | Cross-sectional study | 81% |
| Henok et al. [11] | Knowledge about and Attitude towards Epilepsy among Menit Community, Southwest Ethiopia. | A cross-sectional descriptive study. | 93% |
| Herrmann et al. [26] | Epilepsy misconceptions and stigma reduction: Current status in Western countries. | Systematic review | 92% |
| Holmes, et al. [27] | Attitudes towards epilepsy in the UK population: Results from a 2018 national survey. | Cross-sectional survey. | 95% |
| Kaddumukasa et al. [8] | Epilepsy misconceptions and stigma reduction interventions in sub-Saharan Africa, a systematic review. | Literature review | 87% |
| Karimi et al. [28] | Knowledge and Attitude toward Epilepsy of Close Family Members of PWE in North of Iran | Cross-sectional survey study. | 72% |
| Keikelame et al. [29] | Psychosocial challenges affecting the quality of life in adults with epilepsy and their carers in Africa: A review of published evidence between 1994 and 2014 | Literature review | 60% |
| Keikelame et al. [30] | “I wonder if I did not mess up....”: Shame and resistance among women with epilepsy in Cape Town, South Africa. | Qualitative exploratory design | 95% |
| Mbelesso et al. [16] | Sociocultural representations of epilepsy in the Central African Republic: A door-to-door survey | Cross-sectional survey | 78% |
| Mula, et al. [31] | Psychosocial aspects of epilepsy: a wider approach. | Literature review | 66% |
| Murthy et al. [32] | Potential for Increased Epilepsy Awareness: Impact of Health Education Program in Schools for Teachers and Children | Pre-test post-test experimental design. | 55% |
| Murugupillai et al. [33] | Parental concerns towards children and adolescents with epilepsy in Sri Lanka—Qualitative study. | Qualitative study | 80% |
| Schachter et al. [34] | Successful health communication in epileptology | Literature review | 70% |
| Scott et al. [35] | Anxiety and depressive disorders in people with epilepsy: a meta‐analysis. | Meta-analysis | 70% |
| Singh et al. [36] | Marriage in epilepsy: The impact of the question in knowledge, attitude, and practice surveys | Systematic review | 80% |
| Siriba et al. [13] | The experiences of people living with epilepsy in Nzhelele, Limpopo Province. | Phenomenological study | 88% |
| Thapa et al. [37] | Knowledge, Beliefs, and Practices on Epilepsy among High School Students of Central Nepal | Cross-sectional study | 78% |
2.5. Characteristics of the Included Studies
The study characteristics (Table 3) were found to further justify the studies included. The included studies were those published within the previous 7 years with the acceptance that the area of interest is less researched. The characteristics of the included studies involved the author, studies’ year of publication, design, setting where the study was conducted, study sample, findings, and limitations (Table 3).
| Author/s | Country | Purpose of the study | Design | sample | Findings | Limitations |
| Al-Dossari et al. 2018 [20] | Saudi Arabia | Assess public knowledge awareness and attitudes toward epilepsy in Al-Kharj Governorate Saudi Arabia. | Cross-sectional study | 422 adults living in Al-Kharj governorate | Found that 94.79% of participants have read or heard about epilepsy, 63% knew someone who’s living with epilepsy, and 49.75% have seen a seizure attack. Limited misconceptions, good knowledge, and positive attitudes. | |
| Armah-Ansah et al. 2018 [21] | Ghana | Determine the level of knowledge and attitude towards epilepsy among University Health students at selected universities. | Quantitative Cross-sectional study | 200 participants | 97% of the participants have heard about epilepsy and showed to have good knowledge of epilepsy but exhibit negative attitudes toward epilepsy. | This was a relatively small sample, the study was only limited to health students according to the results, which may have been different if other students from different faculties were included. |
| Benson et al. 2016 [22] | Dublin | Explore sigma experiences of children with epilepsy and their parents. Outline the relationship parents’ and children with epilepsy’s perceptions of stigma, seizure variables, demographics, and communication within the family and external family regarding epilepsy. | Mixed-methods sequential exploratory design | 33 children with epilepsy, 40 parents (qualitative phase 1). 47 children with epilepsy, 72 parents (quantitative phase 2). |
Families generally face stigma, there is little dialogue about epilepsy. Some families do not reveal or aren’t open with diagnosis to others. | The study only focused on parents, more data would have been collected and significant information revealed if other family members were included. There was an over-representation of the mothers which may bring gender obscure perspectives. |
| Braga et al. 2019 [23] | Global-View | Illustrate its noncurricular approach to education on epilepsy, sharing some of the more representative initiatives that have been developed, generally on a local/regional level and which are usually underrecognized | Review | Addressing persons with epilepsy and their families Addressing other target groups and professionals who interact with patients with epilepsy and families Delivering educational courses on epilepsy: tutors, timing, and tools Need for: -Sharing of information -Developing guidelines/processes for chapters who would like to develop courses -Creation of a repository with educational material (necessarily not limited to English) -Include and regularly update useful information on educational activities around the world in the IBE website, with all necessary information and contact data, so they can be reproduced in other countries/regions. |
||
| England et al. 2014 [2] | USA | Outline IOM committee recommendations for public awareness and recommended 8 key messages for communication to promote epilepsy education amongst health workers. | Commentary | IOM recommendations and recommended 8 key messages | Regardless of efforts, misconceptions, and misrepresentations persist, the absence of correct information reinforces negative attitudes and misconceptions. | Recommendations would have had more validity had they been compared with other messages or available methods for public awareness. |
| Fekadu et al. 2019 [24] | Ethiopia | Explore the community’s Perception and Attitude towards People with Epilepsy in Ethiopia. | Cross-sectional study | 701 participants | Participants held misconceptions about the cause, nature of epilepsy, and shared negative attitudes towards epilepsy and people living with epilepsy. | Social desirability in some aspects of the questionnaire. Place of residence may be a limitation. |
| Henok et al. 2017 [11] | Ethiopia | To assess the knowledge and attitude of epilepsy in the selected community. | A community-based, cross-sectional descriptive study. | 840 participants, the majority were 21- 30 years of age. |
The majority (91.1%) had never heard about epilepsy while others thought it was a mental disease, a curse from God, hereditary or contagious. Ethnicity and level of education were associated significantly with knowledge and attitudes. | The methodology of the study was not clear which could have affected the collection and analysis of data. |
| Herrmann et al. 2016 [26] | UK | Exploring the current status of epilepsy misconceptions and stigma reduction. | Systematic review | 61 studies | Different types of misconceptions were similar in reports published and a few interventional studies focus on epilepsy stigma specifically. | |
| Holmes et al. 2019 [27] | UK | To measure stigma that comes from negative attitudes held toward epilepsy in the UK. | Cross-sectional web-based survey. | 4,000 responses collected, 3875 were analyzed. | There’s a relatively low stigma toward people with epilepsy and epilepsy (90%) | On analysis, there may be a possibility of sampling bias. Because the survey was done online through a marketing panel, results may be influenced by reducing external validity. |
| Kaddumukasa et al. 2018 [8] | Sub Saharan Africa | To describe epilepsy misconceptions or stigma and research interventions attentive toward reducing these misconceptions in sub-Saharan Africa. | Literature review | 23 publications included | In Sub-Saharan Africa, Epilepsy stigmatizing cultural beliefs, misconceptions are extensively prevalent. There is a need for stigma reduction interventions. Present stigma- reduction educational methods may be unviable for the general population for successful implementation. | Researchers may not have acknowledged all relevant articles, and review and search strategy may have introduced some bias. Due to the difference in designs, frequency, and nature of misconceptions could not be compared. |
| Karimi et al. 2016 [28] | Iran | To evaluate the knowledge and attitudes of family members of people living with epilepsy on epilepsy. | Cross-sectional survey study | 124 participants were surveyed. | There is good knowledge (50%) and a positive attitude (87.9%) of family members. | Reported there is insufficient information regarding incorrect beliefs, this may be due to a nonreliable questionnaire. |
| Keikelame et al. 2017 [29] | Africa | From the published studies conducted in Africa between 1994 and 2014 on psychological challenges faced by adult people who have epilepsy as well as their caregivers, examine the type of psychological challenges. The aim was also to identify gaps in current scientific knowledge. | Literature review | Sample unknown | People with epilepsy and their caregivers experience psychological challenges at different health systems levels, this, in turn, affects their quality of life. There is a need for research on psychological challenges on adults with epilepsy in different health care sectors. | Important information may have been lost based on inclusion and exclusion criteria. The aim of the study was more modest and the method was not a systematic review. Researchers’ views, background, and gender may have influenced the interpretation of findings. |
| Keikelame et al. 2018 [30] | South Africa. | To understand shame and resistance strategies of women with epilepsy. | Qualitative exploratory design | 4 adult Xhosa -speaking women | Women with epilepsy experience shame but they show resistance to discrimination as a coping mechanism. Suffering persists due to a lack of support and socio-economic inequalities. | Small scope. Not all types of shame were explored. |
| Mbelesso et al. 2019 [16] | The Central African Republic. | To describe the sociocultural representations of epilepsy. | Cross-sectional door-to-door survey | 1023 participants | Misconceptions are prevalent in Sub-Saharan Africa | Prevalence might be underestimated due to the sample. The study mostly involved women and individuals under 29. Researchers were not able to determine the association between sociodemographic data and social consequences. |
| Mula et al. 2016 [31] | UK | To discuss epilepsy psychosocial issues with an emphasis on the relationship between psychiatric comorbidities and stigma. discuss psychosocial issues in epilepsy with a special focus on the relationship between stigma and psychiatric comorbidities. |
Literature review | Sample unknown | The burden of epilepsy also results in psychological consequences like negative attitudes of people (social stigma, social segregation, and absence of support). | The literature review didn’t provide methodology. Review only focused on people with epilepsy, different findings would have resulted if psychological problems were explored from parent/caregiver’s perspectives. |
| Murthy et al. 2020 [32] | India | Evaluating the impact of health education programs in schools. | Pre-test post-test experimental design. | 39 teachers from eight schools and 50 children from a government school participated. | Including health education programs in education is a crucial way to cause a change in behaviour, attitude, and practices concerning epilepsy. | |
| Murugupillai et al. 2016 [33] | Sri Lanka | To identify concerns parents have regarding their children and adolescents with epilepsy. | Qualitative study | 16 participants of which some were sampled for a focus group. | Concerns that parents hold show a multidimensional construct. Key influential factors (seizure unpredictability, fear of stigma, epilepsy unawareness) mould personal concerns. | The sample may not represent the total population. The inclusion of participants who have another illness may have created confounding effects during data collection. |
| Schachter 2017 [38] | USA | Discuss what motivates changing communication patterns on epilepsy and barriers that persist, and tools available to enhance communication. | Literature review | Sample unknown | Rising knowledge and changing epilepsy attitudes and perceptions will demand an increase in ongoing efforts to provide more educational programs. Establishing new models for epilepsy care will need effective communication procedures to send educational tools. | |
| Scott et al. 2017 [35] | Australia | Evaluate the correlation between anxiety and depressive disorders in people with epilepsy. | Meta-analysis | 27 studies | Findings suggest the prevalence of anxiety and depressive disorders in PWE are equivalent. | |
| Singh et al. 2018 [36] | Globally | Examine stigma and perceptions associated with epilepsy in marriage. | A systematic review (meta-proportion with meta-regression analysis) | 103 included studies for qualitative synthesis | Questions regarding an individual marrying or family member marrying someone with epilepsy result in more negative attitudes as compared to general questions on marriage worthiness of person with epilepsy. | There was a lack of available data. Social desirability data may have resulted in studies that collected their data using a telephonic survey. |
| Siriba 2014 [13] | Limpopo province, Nzhelele village. | Explore the personal experiences of people living with epilepsy in a selected area, as well as understanding their responses to what causes epilepsy. | Qualitative phenomenological study | 3 males, 3 female Venda-speaking people with epilepsy | Participants understand epilepsy based on their experiences. Different methods of treatment are tried and for them epilepsy causes distress. | The omission of data due to translation, results cannot be generalized due to a small sample. |
| Thapa et al. 2017 [37] | Central Nepal | To assess the knowledge, practices, and beliefs of epilepsy. | Cross-sectional study | 1360 High School Students | Overall inadequate knowledge, beliefs, and practices. There is a need for further epilepsy educational. | Only included private school students making it not representative. Results may have been different if government students were included also. |
2.6. Thematic Analysis of Selected Studies
Thematic analysis was done according to the method proposed by Caulfield [38]. After reading the abstracts, the main researcher read the full articles to further familiarise themselves with the data. Following this, coding was done where the main researcher read and highlighted common words, expressions and findings within the data. From these, themes were created as illustrated in Table 4, named and reviewed by the primary author and co-authors, which later led to writing of the article. The thematic analysis yielded three themes including the impact of epilepsy (n=11) [11, 14, 19-27], the level of knowledge and awareness (n=11) [8, 13, 22-24, 29-33, 36] and available epilepsy awareness guidelines (n=4) [2, 23, 32, 38]. From these three themes, seven subthemes emerged.
| Themes | Sub-themes |
| Misconceptions regarding knowledge and awareness of epilepsy | • Misconceptions and stigma |
| • The nature of epilepsy | |
| • Cause of epilepsy | |
| • Beliefs regarding epilepsy treatment | |
| The impact of epilepsy | • Impact on people living with epilepsy |
| • Impact on families and the surrounding community | |
| Epilepsy awareness guide | • Developing an awareness guide for public education |
3. RESULTS
All the included articles highlighted two parts to the knowledge of epilepsy that the public has. Thematic analysis was applied for this study. The first part being misconceptions held about people living with epilepsy and epilepsy. The second part includes the overall knowledge of the disease. Unfortunately, the misconceptions/understanding of epilepsy as represented by the general public, people with epilepsy and their families affect how people treat and relate to people with epilepsy. It also affects how people living with epilepsy react to these treatments and behave as well as how much their families are impacted by the person with epilepsy. These results (summarized in Table 4) highlight the focus that is put on misconceptions regarding knowledge and awareness of epilepsy (n= 11) [8, 11, 13, 16, 20, 21, 26-28, 31, 37], the impact of epilepsy (n= 11) [8, 13, 22-24, 29-33, 36] and less on awareness programs and guidelines (n= 4) [2, 23, 32, 38] that can sufficiently correct misconceptions and empower people with epilepsy. The co-authors of the study verified the themes and subthemes, presented in Table 4, before proceeding with the writing of the article for quality assurance.
3.1. Misconceptions Regarding Knowledge and Awareness of Epilepsy
There is a noticeable gap in the level of knowledge about epilepsy between African countries, European countries, Asian countries, and America. Amongst the Western and Australian population, a national survey carried out showed very low stigma and satisfactory knowledge levels regarding epilepsy [11]. In Asia, although people living with epilepsy have somewhat adequate knowledge about the disease, there is marked inadequate knowledge in the general public regarding epilepsy [28, 37]. Because of this, we find that close family members of people living with epilepsy have strong conceptions and good knowledge about epilepsy. In that, they believe that epilepsy is a brain disorder (87.1%) or an infectious/contagious disease (96%) and is not from a supernatural origin (88.7%) [26, 28]. However, they have less information about the triggers of epilepsy. General awareness of the disease is not certain in Asia, especially because some hold that sleep deprivation, certain drinks and foods trigger seizures [28]. With this, it may be argued that different population groups filter their understanding of epilepsy through their cultural experiences. Western and Australian populations have more access to scientific knowledge on epilepsy compared to people from less developed countries. Inadequate knowledge, false beliefs and awareness of epilepsy result in misconceptions about epilepsy and stigma toward people living with epilepsy.
A study in Ghana stated that although about 97.5% of people said to have heard about epilepsy, they still shared negative attitudes towards it, resulting in segregation and stigma [21]. A couple of studies conducted in African countries give an overview of how knowledgeable people in Africa are about epilepsy. In Ethiopia, 97% have ever heard about epilepsy of which 85.6% proved not to be knowledgeable regarding epilepsy and 86.8% expressed a generally negative attitude towards epilepsy and people living with epilepsy [11]. These statistics are incomparable to the 5.9% who had never heard of epilepsy in the study conducted in Asia [37].
3.1.1. Misconceptions and Stigma
Misconceptions and stigmatization are associated with low socioeconomic status and low levels of education [26, 27]. In rural Sub-Saharan African countries, there is a persistent prevalence of epileptic misconceptions [20]. Perceptions, stigma, and misconceptions on epilepsy are based on culture and wrong information taught [20]. This speaks into the misconceptions concerning the nature of epilepsy, causes of epilepsy, and beliefs regarding treatment.
3.1.2. The Nature of Epilepsy
Epilepsy is believed to be a disease that is contagious and can be transmitted through saliva [16, 20]. Besides, there are reports that it is suggested to be a blood pressure disease [16, 20]. While, others believe it to be a psychiatric disorder. The findings of this review indicate that 79.5-85.3% believe epilepsy to be a psychotic condition or mental disease [11, 21]. Another perception of the nature of epilepsy is that it is understood solemnly as a sickness that is characterized by falling [13]. In addition to this, 75.3% of people confuse epilepsy to be a contagious mental disorder and view it as associated with witchcraft, an evil curse, or pure bad luck [16]. People generally view epilepsy to be hereditary and contagious [11, 13, 21]. Misconceptions about the nature of epilepsy ultimately shape the attitudes that people have regarding epilepsy, people living with epilepsy as well as their families. It is also most likely that these myths are the reason behind negative conduct or behaviour toward people living with epilepsy, keeping in mind that ideas associated with the nature of epilepsy are often closely related to beliefs regarding its causes.
3.1.3. Causes of Epilepsy
Literature reveals that epilepsy is believed to be caused by different factors. Epilepsy can be caused or triggered by stress or extreme heat; it may also be caused by supernatural factors which include witchcraft, a curse from God or demonic evil spirits [11, 13, 20, 21]. This understanding has grown vastly in most African countries, suggesting even further that misconceptions and insufficient knowledge are more prevalent in less developed countries with a lower socioeconomic status.
3.1.4. Beliefs Regarding Epilepsy Treatment
Most studies (n= 3) report that epilepsy can be cured traditionally, and others indicate that it is incurable. Thus, people believe that epilepsy can be cured by traditional means [16] such as wearing an amulet, while others believe it is incurable [8]; majority of the population (67%) reported that epilepsy is not treatable [21]. The public also reported other measures that in the case a person is having a seizure, those with the patient should either sprinkle them with olive oil, place the spoon between their teeth, have them smell the smoke of a lit match, pour water on their face or give them a sweet during the seizure to stop the seizure [20]. Beliefs regarding the treatment of epilepsy show a connection thread where beliefs regarding the causes and nature of epilepsy influence the type of treatment pursued or is lacking thereof. In addition to this, beliefs regarding the causes and nature of epilepsy have an impact on people living with epilepsy and their families/ caregivers’ life experiences and day-to-day social living.
3.2. The Impact of Epilepsy
Due to stigmatization and misconceptions held, epilepsy has a negative impact on the person who has epilepsy (n=10) [8, 13, 22-24, 29-33, 36], their family members and the world as a global community (n=3) [23, 31, 33]. The data collected showed several challenges that different stakeholders face because of having epilepsy or being associated with people living with epilepsy. These challenges include education, marriage, psychological wellbeing, psychosocial challenges, economic stability, social life, employment, and attaining treatment.
3.2.1. Impact on People Living with Epilepsy
People living with epilepsy are believed to experience issues in their marriages, which reduces the prospects of getting married [24]. As revealed, about 53.5% of the population believed people living with epilepsy should not marry at all [8]. Additionally, people living with epilepsy have a negative attitude towards marriage due to experienced low levels of satisfaction within marriage and increased divorce rate [24]; on the other hand, people living without the disease refuse to marry people living with epilepsy [20]. It is possible that following the believed causes and nature of epilepsy, it is understood as impossible to manage because some people consider epilepsy to be unmanageable. This makes the disease seem burdensome.
People living with epilepsy are excluded from community involvement; they are not allowed to play with other people as epilepsy is believed to be contagious, adding to their isolation and segregation [20]. People living with epilepsy are marginalized in terms of driving and employment; they are considered as burdens in their careers and it is believed that they should not be touched or shaking hands with them is also seen forbidden [36]. Literature has also highlighted that 30% of a study’s sample believed that people living with epilepsy should be isolated from society, 40% said they exclude themselves from them and have their children isolated from any known person with epilepsy [21]. Murugupillai et al. [33] show that their families take measures to isolate them as a form of precaution, and these are the same people that abandon them because of their condition [36]. Children with epilepsy under the supervision of adults are not allowed to play with others, their diet is monitored so as not to provoke seizures, and they are also not allowed to cycle or climb trees.
Their general rights are taken from them due to being isolated; it is believed that they should not be allowed to work or study with other people as well have children of their own [8]. In addition to shared rights that are not extended to people living with epilepsy, they are excluded from competing equally with people without epilepsy for an employment position [20]. Living with epilepsy is also believed to have the potential to also result in poor academic achievement and limited career prospects [13]. The findings indicate that epilepsy may result in poor performance in school as it sometimes causes learning difficulties like slowness, difficulties in memorizing and understanding concepts [29]. Additionally, people living with epilepsy feel that epilepsy disrupts them from attaining their goals educationally [33].
How others view epilepsy and their attitude toward it causes great distress for people living with epilepsy. This results in interpersonal challenges and they become impatient with other people expressing general consistent agitation [13]. People living with epilepsy often experience shame, which in turn evokes feelings of guilt that often come from the feeling of burdening others, grief, and anger, and for most of them, epilepsy leads to fear and anxiety [33, 13]. It has also been revealed that epilepsy can have an impact on people’s (living with epilepsy) speech and add to their language difficulties [30]. In addition to that, people living with epilepsy generally experience anxiety disorders and mood disorders. The weight of stigma, discrimination, and social limitation often leads to low self-esteem and depression which also contributes to suicide. People living with epilepsy may not be able to perform day to day tasks and they may also lead to physical injuries [29]; this may often make them feel helpless and anxious.
3.2.2. Impact on Families and the Surrounding Community
Epilepsy has a clear impact on caregivers or families, especially if seizures start at an early age [30]. Having an epileptic child makes parents/guardians worry constantly [29]. Parents are in constant distress and worry about the safety of the child when they are away from them and a seizure is to occur. As a response to internalized negative feelings and the impact of epilepsy, people with epilepsy become bullies, detached, and violent [33]. Literature reveals that some authors argue that people living with epilepsy often develop aggression, stubbornness, and anger, which makes them hostile toward others [24]. Consequently, as much as people with epilepsy are excluded, their families’ activity is also excluded [36]. This exclusion and stigma are mostly from community members and external family members. Besides exclusion, they also experience teasing and bullying [33]. This results in the patients having internalized negative feelings towards others or their family members.
3.3. Awareness Guide
This section is composed of developing an awareness guide for public education (n= 4) [2, 23, 32, 38]. Generally, there are guidelines made for professional training, and guidelines used to develop campaign content are not made available to the public. Although found necessary, there is a shortage of epilepsy educational programs which results in rare limited published content [23]. The researcher did not come across any awareness program or recommended guide for public education. There are, however, a couple of guides available to educate and equip professionals [38], and in terms of educating the general public, the researcher found eight key messages and the Institute of Medicine (IOM) recommendations to include when developing an awareness guide [2]. These messages are widely used in different education processes such as campaigns and may serve as a basis for epilepsy education program development due to their comprehensiveness and flexibility to contextualization.
3.3.1. Developing an Awareness Guide for Public Education
There are eight key messages recommended for educational content as prescribed by England et al. [2]. In their study, they highlight different campaigns for education that has been centralized around information from the Centre for Disease Control and Prevention [2, 32].
| Eight Key messages for Epilepsy education: |
| 1. Epilepsy is a common brain disorder that affects 1 in 26 people during their lifetime; this includes men, women, and children of all ages, races, ethnicities, and socioeconomic conditions. |
| 2. Epilepsy is a spectrum disorder that varies in severity, causes, treatments, and outcomes, and is not contagious. |
| 3. Epilepsy can be a serious, life-threatening disorder with a great impact on health and quality of life, including increased risk of injury and death. |
| 4. Nearly two out of three people with epilepsy control their seizures with medication. |
| 5. Epilepsy specialists and centers have the expertise to treat and manage complex cases with both time-tested and new therapies and procedures, including surgery. |
| 6. Anyone can learn basic first aid to help someone when a seizure occurs. |
| 7. Most people living with epilepsy are fully functioning members of society, with responsibility for jobs, families, and all aspects of life. |
| 8. The stigma associated with epilepsy can cause serious harm to the physical, mental, and social well-being of a person with epilepsy. |
Source: England et al. (2014)
Although they suggested that education must include accurate and relevant information on epilepsy and appropriate seizure response, the messages are centered around erasing stigma. This shows that there is still a need for developing a guideline for epilepsy education and shared awareness programs that are inclusive of different stakeholders, addressing different issues in epilepsy.
| Recommendation: “Inform Media to Improve Awareness and Eliminate Stigma” | Recommendation: “Coordinate Public Awareness Efforts” |
| • Promote accurate TV storylines and depictions of epilepsy. • Encourage high-profile individuals living with epilepsy to serve as spokespersons. • Partner with stakeholders (e.g., those in the mental health community) to educate journalists. • Promote epilepsy research and human-interest stories among news media. Disseminate regular updates on epilepsy advances via electronic and social media and face-to-face meetings. |
• Establish an advisory council of stakeholders and audience members to inform efforts throughout all phases of education and campaign activity. • Develop shared messages among partners. • Explore and develop an ongoing, multimedia campaign to reduce stigma. • Ensure culturally sensitive campaigns and formative and summative research. |
Table 5 shows recommendations for epilepsy education from the IOM. The eight key messages had been highlighted for the sake of uniformity during the development of an awareness program, campaign, or any epilepsy education material [2].
Although not widely used, Schachter [38] reported having adapted these IOM recommendations to establish healthy communication in epilepsy. Additionally, it was clear that amidst the IOM recommendations adaptation, the best methods for communicating knowledge in epilepsy are still needed. Unlike the key messages of epilepsy that speak regarding epilepsy stigma, these recommendations focus on how messages about epilepsy can reach the public and provide pathways of communication. Together, the eight key messages and IOM recommendations provide a basic message to share aimed at curbing and eliminating stigma and provide the suggested means to disseminate the message across the general public.
4. DISCUSSION
How much people know is informed by different beliefs and information gathered through experiences or information made available. According to the results of this review, developing countries still have prevailing misconceptions about epilepsy because they do not have access to comprehensive and readily available information. Misconceptions arise due to ill-education or no education. These misconceptions bring about certain behaviours that people present towards those living with epilepsy and their families. Taking a closer look at the results of the review, there is not enough being done to correct the misconceptions held. Not enough interventional studies are taking root considering that there are some studies highlighting the impact of epilepsy as negative and exploring different ideas that people hold about it.
Some individuals believe that epilepsy is simply a disease of falling; describing a disorder by one of its characteristics may be a result of two things: ignorance or lack of knowledge. Based on the findings of this review, the latter seems to be the cause. Most individuals hold that epilepsy originates from supernatural power (either as punishment from God or as being possessed by evil spirits). This view is strongly influenced by culture and faith, and this could be because, in Africa, most of the people filter their experiences through their beliefs. Literature proposes that more initiatives should be invested in educating lesser privileged countries about epilepsy as they still carry misconceptions [37]. This may be because these beliefs on epilepsy are attached to their faith, their way of life and there has been little to no attempt to correct these conceptions medically.
Adding on to this, there seems to also be a connection between what people think epilepsy is, what they believe is the cause, and how they choose to remedy the disorder. There may be an association between the belief that epilepsy is caused by spiritual forces like God or witchcraft and seeking treatment from churches or traditional healers. As well as a correlation between the belief that epilepsy is a psychiatric disorder and people with epilepsy wear a helmet. This shows that to change misconceptions, one aspect (like cause alone) cannot be investigated because one aspect influences another. Correcting misconceptions may reduce the impact that people living with epilepsy, their families, and communities experience.
This current study shows that there is an obvious impact of epilepsy on the person living with epilepsy, their close family, and globally. Since epilepsy is not dependent on age, studies show that younger people with epilepsy experience more emotional, psychosocial, and psychological impacts as they have not yet developed a sense of self that could contribute to their resilience to stigma and segregation. This puts pressure on parents and guardians, although evidence highlights that parents also avoid talking to their children about their condition [30].
Families of people living with epilepsy often alter their lives to fit the needs of the person with epilepsy as they may be unable to care for themselves. This leads to feeling burdened, worry, and anxiety, and to some degree shame, based on community’s perception of epilepsy. It has also been reported that people living with epilepsy often feel guilty for burdening caregivers, which often leads to anger, shame, depression and anxiety. All these feelings are derived from how the external world around them behaves, speaks about them, and relates to them. This often leads to suicide, as stated in the results. Besides suicide, mortality may increase due to extreme injury or when a person has a seizure in places that are hazardous like fire, near a pool, or the first floor. These impacts stress even more the need for epilepsy awareness programs that will educate individuals on the nature, cause, and management of epilepsy as well as provide training on a first responder’s conduct during an occurrence of an epilepsy seizure. Altogether, levels of knowledge related to epilepsy amongst the African general public are hardly satisfactory but are too often reported to be moderate or poor.
Although sustainability is unknown, looking into initiatives put toward epilepsy awareness globally has provided many results as studies in the UK, Asia, and the USA show somewhat an adequate knowledge and awareness of epilepsy. With adequate funding, African countries can as well pick up momentum on epilepsy communication and education. The focus has been widely on describing the perspectives held on epilepsy, exploring the stigma held by the general public, and clinical knowledge of the disorder. Not enough attention is being given toward contextually educating (according to their beliefs and perceptions) the general public about the disorder to reduce misconceptions and stigma. It also becomes evident that more research is needed to develop a sustainable model for communication about epilepsy that involves different stakeholders such as health care professionals or practitioners, family members, community health workers, campaigners, media, and schools.
The key messages are, however, considered as central messages that can be employed within the content of any program, guide, or campaign. Although the messages were prescribed for reducing and stopping stigma, these messages do not include a specific focus on disregarding misconceptions. The messages are generalized and not misconception focused based on different cultural backgrounds and contexts. The key messages along with the IOM recommendations can serve as a fundamental idea for the development of an awareness program for the dispatch of epilepsy knowledge and reduction of stigma and discrimination. Disregarding the fact that stigma is caused by a lack of knowledge or awareness about epilepsy, not speaking into the root causes and beliefs about the nature of epilepsy (context-specific) may result in slow progression and delay in change of behaviour towards epilepsy.
CONCLUSION AND RECOMMENDATION
This current study sought to examine how much knowledge and awareness people have regarding epilepsy. This was done through analysing the study sample, which included 22 studies that went through critical appraisal and PRISMA. The study inclusion and exclusion criteria were followed. From the included studies, 3 themes and 7 sub-themes were extracted. The key findings showed that although epilepsy is a global issue, there is a somewhat satisfactory level of knowledge and awareness in developed countries compared to developing countries. Evidently, there is a remarkable gap in intervention and epilepsy education, especially in less privileged countries. What people believe regarding the cause and nature of epilepsy is found to influence treatment preferences which have the potential to hinder intervention and successful education if it is not contextualised. Epilepsy is an under-researched health issue in developing countries which not only requires attention from authors but health workers, the general population as well as policymakers. There is a strong need for further research and development of epilepsy awareness programs to promote epilepsy education and awareness as this current study reveals that all together, there is generally inadequate knowledge and awareness of epilepsy. Policymakers should support efforts initiated towards improving the knowledge and lives of people living with epilepsy to reduce the burden of epilepsy, stigma and related misconceptions.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors are grateful to the GladAfrica Foundation Trust for funding the project that this study falls under.


