All published articles of this journal are available on ScienceDirect.
Spectrum of Initial Computed Tomography Findings in RT-PCR Positive Patients with Novel Coronavirus 2019 Disease – A Systematic Review of 2327 Cases
Abstract
Coronavirus disease 2019 (COVID-19) is a highly infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of April 17, 2020, the total number of cases all over the world read as 2,182,823 positive cases with 145,551 deaths and 547,679 recovered cases. In India, the total number of affected cases has alarmingly increased up to 13,430, crossing the 10 thousand mark with 11,214 active cases and 1768 recovered cases. There have been multiple studies and reviews published regarding the nature of the disease, its clinical symptoms and their progression, as well as findings on chest radiography, computed tomography, and positron emission computed tomography.
A systematic literature search of the PubMed database was performed on April 8, 2020, using the suitable keywords and publications on novel coronavirus infection were also searched for in the WHO database. Only those articles published in the year 2020 were included. Data were collected, extracted, and tabulated for systematic reviewing from 26 original articles and 4 case series. The typical radiological findings on computed tomography for COVD 19 were ground-glass opacity with and without consolidation, isolated consolidation, air bronchogram, crazy paving, and interlobular septal thickening with subpleural lines.
With the progression of the disease, other atypical radiological findings are noted, such as pulmonary atelectasis, peribronchial thickening, pleural effusion, pericardial effusion, mediastinal lymphadenopathy, reverse halo or atoll sign, and tree in bud appearance with bronchiectasis. Computed tomography proved as a useful tool for screening COVID 19 cases to delineate the status and severity of lung pathology.
1. INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a highly infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. The disease was first identified in December 2019 in the city of Wuhan, the capital of Hubei province, China, which has now spread to other countries giving it the form of a pandemic [2, 3]. The World Health Organization(WHO) declared the 2019–20 coronavirus outbreak as a Public Health Emergency of International Concern(PHEIC) on January 30, 2020, and a pandemic on March 11, 2020 [4, 5].
As of April 17, 2020, the total number of cases all over the world read as 2,182,823 positive cases, with 145,551 deaths and 547,679 recovered cases. In India, the total number of affected cases has alarmingly increased up to 13,430 cases, crossing the 10 thousand mark with 11,214 active cases and1768 recovered cases [6].
As the primary site of involvement of novel coronavirus 2019 infection is the respiratory tract, both chest radiography and computed tomography are go-to modalities to screen the suspected cases. However, when both are compared in terms of accuracy, computed tomography fares better than the former, reinforcing its importance in both initial screenings of suspected cases and follow-up scans of such cases with the progression of timeline [7-9]. The existing information regarding the dreaded disease is diffused and seemingly incomplete, owing to its scattered nature. There have been multiple studies and reviews published regarding the nature of the disease, its clinical symptoms and their progression, as well as radiological findings on chest radiography, computed tomography, and positron emission computed tomography [10-13].
Therefore, the purpose of this systematic review article is to delineate the initially presented radiological findings on computed tomography in real-time polymerase chain reaction positive cases for COVID-19 infection so as to assist the radiologist in pinpointing the desired direction in such scenarios.
2. MATERIALS AND METHODS
A systematic literature search of PubMed database was performed on April 8, 2020 using the keywords “(((((( (((“COVID 19”[Title/Abstract] OR “COVID 19”[Title/ Abstract]) OR “COVID 19”[Title/Abstract]) OR “SARS-CoV-2”[Title/Abstract]) OR “severe acute respiratory syndrome coronavirus 2”[Title/Abstract]) OR “ncov*”[Title/ Abstract]) OR “corona virus”[Title/Abstract]) OR “corona- virus”[Title/Abstract]) OR “coronavirus”[MeSH Terms]) OR “sars virus”[MeSH Terms]) AND ((((((((((((“radiolog*” [Title/Abstract] OR “radiograph*”[Title/Abstract]) OR “X-ray”[Title/Abstract]) OR “ct”[Title/Abstract]) OR “computed tomograph*”[Title/Abstract]) OR “MRI”[Title/Abstract]) OR “magnetic resonance imaging”[Title/Abstract]) OR “sonography” [Title/Abstract]) OR “ultrasound”[Title/ Abstract]) OR “ultrasonograph*”[Title/Abstract]) OR “radiography”[MeSH Terms]) OR “tomography, x-ray computed”[MeSH Terms]) OR “ultrasonography”[MeSH Terms]). Publications on novel coronavirus infection were also searched for in the WHO database[15]. Only those articles published in the year 2020 were included.
2.1. Eligibility Criteria and Study Selection
Studies included in this systematic review were those published in the perspective of novel coronavirus 2019 disease and included computed tomography as the diagnostic intervention. All studies other than original articles were excluded. All included studies were reviewed by two reviewers on the basis of criteria for eligibility [16]. Any discrepancy between reviewers was resolved by discussion.
3. RESULTS
3.1. Results of the Search Strategy
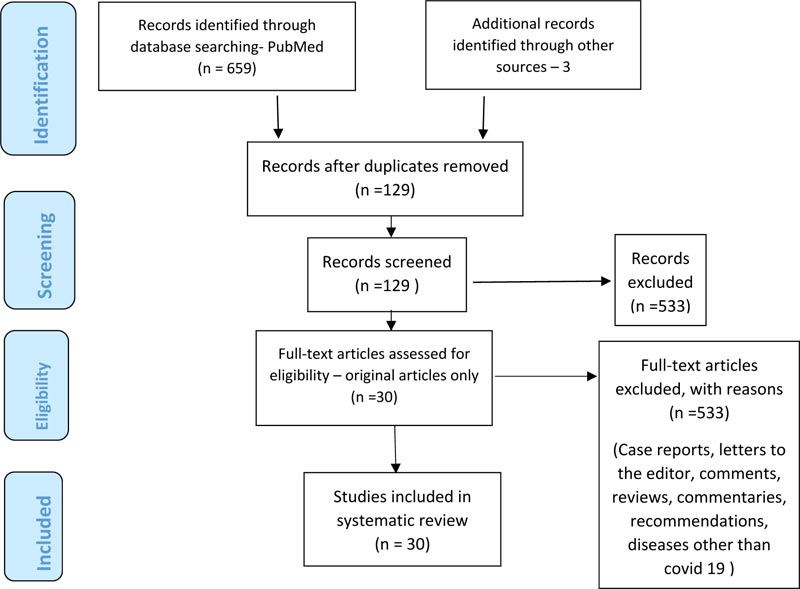
Upon systematic searching of the PubMed database using suitable keywords, a total of 659 articles were retrieved. Additional literature search added 3 more articles. Upon removal of duplicate search records, a total of 129 records were identified. After the search records were screened, 30 studies consisting of 26 original articles and 4 case series with a total of 2327 patients were included in the final review (Fig. 1).
3.2. Overview of the Included Studies and Assessment of the Risk of Bias
Out of the included studies (n=30), 29 studies were from China and only one study was from Korea. Four studies were prospective, whereas 26 were retrospective. Studies with minimum and maximum number of participants, the total number of participants, and the characteristics of the included studies are presented in Table 2.
NIH quality assessment tool for systematic reviews and meta-analyses was referred for quality assessment of the included studies [17]. The quality assessment of included studies was carried out by two reviewers on the basis of NIH quality assessment criteria as represented in Table 1, where the included studies have been assessed using NIH quality assessment tool. Out of 30 included studies, 4 were rated as poor by both observers and 26 were rated as fair by both.
| Study ID (year) |
Question | Overall rating | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| K C Liu et al. (2020) [17] | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Reviewer 1 | Reviewer 2 |
| JFW Chan et al.(2020) [25] | Yes | No | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Chaolin Huang et al.(2020) [37] | Yes | No | NA | CD | NA | Yes | CD | No | No | Poor | poor |
| Chunbao xie et al.(2020) [38] | Yes | No | NA | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Fang liu et al(2020) [39] | Yes | No | NA | CD | NA | Yes | CD | No | No | poor | Poor |
| Xi xu et al.(2020) [40] | Yes | NA | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Xiao wei et al(2020) [41] | Yes | NA | No | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Yang s et al.(2020) [26] | Yes | NA | No | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Soon ho yoon et al(2020) [27] | Yes | NA | CD | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Mingli yuan et al.(2020) [28] | Yes | NA | CD | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Li y et al.(2020) [42] | Yes | CD | CD | CD | NA | Yes | CD | No | No | poor | Poor |
| Chung m et al.(2020) [30] | Yes | CD | CD | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Bernheim et al.(2020) [31] | Yes | CD | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Zhao et al.(2020) [32] | Yes | CD | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Xia w et al.(2020) [43] | Yes | CD | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Feng pan et al.(2020) [29] | Yes | CD | NA | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Wei li et al.(2020) [44] | Yes | CD | NA | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Han r et al.(2020) [45] | Yes | CD | NA | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Xiong et al.(2020) [46] | Yes | No | NA | NA | NA | Yes | CD | No | No | poor | Poor |
| Jiang wu et al.(2020) [47] | Yes | No | NA | NA | NA | Yes | CD | No | Yes | fair | fair |
| Xiaoli Zhang et al.(2020) [48] | Yes | No | NA | NA | NA | Yes | CD | No | Yes | fair | fair |
| Wu jing et al.(2020) [49] | Yes | No | NA | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| Chun shuang guan et al.(2020) [50] | Yes | NA | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Feng xiang song et al.(2020) [51] | Yes | NA | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Yu huan xu et al.(2020) [52] | Yes | NA | CD | CD | NA | Yes | CD | NA | Yes | fair | fair |
| Yicheng fang et al.(2020) [53] | Yes | No | CD | CD | NA | Yes | CD | NA | Yes | fair | fair |
| Wang et al.(2020) [34] | Yes | CD | CD | CD | NA | Yes | CD | NA | Yes | fair | fair |
| Heshui shi et al.(2020) [54] | Yes | CD | CD | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Yang et al.(2020) [55] | Yes | CD | No | CD | NA | Yes | CD | Yes | Yes | fair | fair |
| Pan et al.(2020) [9] | Yes | No | No | NA | NA | Yes | CD | Yes | Yes | fair | fair |
| S. No. | Study ID (Year) | Country | Study design | Participant details (median age in years) |
Diagnostic test details | Outcomes (of interest) reported |
|---|---|---|---|---|---|---|
| 1 | K C Liu et al. (2020) [17] | China | Retrospective | Total #:73 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram, crazy paving, interlobular septal thickening |
| Age:41.6+_14.5 | ||||||
| M/F:41/32 | ||||||
| 2 | JFW Chan et al.(2020) [25] | China | prospective | Total #:5 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram, |
| Age:38 | ||||||
| M/F:3/2 | ||||||
| 3 | Chaolin Huang et al.(2020) [37] | China | prospective | Total #:41 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation |
| Age:49 | ||||||
| M/F:30/11 | ||||||
| 4 | Chunbao xie et al.(2020) [38] | China | prospective | Total #:9 | High resolution CT chest – thin section | GGO |
| Age:38.3 | ||||||
| M/F:4/5 | ||||||
| 5 | Fang liu et al.(2020) [39] | China | prospective | Total #:10 | High resolution CT chest – thin section | GGO, consolidation |
| Age:42 | ||||||
| M/F:4/6 | ||||||
| 6 | Xi xu et al.(2020) [40] | China | retrospective | Total #:90 | High resolution CT chest – thin section | GGO, consolidation, crazy paving, interlobular septal thickening |
| Age:50 | ||||||
| M/F:39/51 | ||||||
| 7 | Xiao wei et al.(2020) [41] | China | retrospective | Total #:62 | High resolution CT chest – thin section | GGO |
| Age:41 | ||||||
| M/F:35/27 | ||||||
| 8 | Yang s et al.(2020) [26] | China | retrospective | Total #:44 | High resolution CT chest – thin section | GGO, air bronchogram |
| Age:48.5 | ||||||
| M/F:25/19 | ||||||
| 9 | Soon ho yoon et al.(2020) [27] | Korea | retrospective | Total #:9 | High resolution CT chest – thin section | GGO with consolidation, consolidation, air bronchogram, crazy paving |
| Age:54 | ||||||
| M/F:4/5 | ||||||
| 10 | Mingli yuan et al.(2020) [28] | China | retrospective | Total #:27 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidationair bronchogram |
| Age:60 | ||||||
| M/F:12/15 | ||||||
| 11 | Li y et al.(2020) [42] | China | retrospective | Total #:51 | High resolution CT chest – thin section | GGO with consolidation, consolidation, air bronchogram, crazy paving |
| Age:58 | ||||||
| M/F:28/23 | ||||||
| 12 | Chung m et al.(2020) [30] | China | retrospective | Total #:21 | High resolution CT chest – thin section | GGO with consolidation, consolidation, air bronchogram, crazy paving |
| Age:51+_14.5 | ||||||
| M/F:13/8 | ||||||
| 13 | Bernheim et al.(2020) [31] | China | retrospective | Total #:121 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation |
| Age:45.3+_16 | ||||||
| M/F:61/60 | ||||||
| 14 | Zhao et al.(2020) [32] | China | retrospective | Total #:101 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation |
| Age:44.4 | ||||||
| M/F:56/45 | ||||||
| 15 | Xia w et al.(2020) [43] | China | retrospective | Total #:20 | High resolution CT chest – thin section | GGO, consolidation, crazy paving |
| Age:2.15 | ||||||
| M/F:13/7 | ||||||
| 16 | Feng pan et al.(2020) [29] | China | retrospective | Total #:21 | High resolution CT chest – thin section | GGO, consolidation, crazy paving |
| Age:40+_9 | ||||||
| M/F:6/15 | ||||||
| 17 | Wei li et al.(2020) [44] | China | retrospective | Total #:5 | High resolution CT chest – thin section | GGO |
| Age:3.4 | ||||||
| M/F:3/2 | ||||||
| 18 | Han r et al.(2020) [45] | China | retrospective | Total #:108 | High resolution CT chest – thin section | GGO, air bronchogram, crazy paving |
| Age:45 | ||||||
| M/F:38/70 | ||||||
| 19 | Xiong et al.(2020) [46] | China | retrospective | Total #:42 | High resolution CT chest – thin section | GGO with consolidation, air bronchogram, interlobular septal thickening |
| Age:49.5+_14.1 | ||||||
| M/F:25/17 | ||||||
| 20 | Jiang wu et al.(2020) [47] | China | retrospective | Total #:80 | High resolution CT chest – thin section | GGO, consolidation, crazy paving, interlobular septal thickening |
| Age:44+_11 | ||||||
| M/F:42/38 | ||||||
| 21 | Xiaoli khang et al.(2020) [48] | China | retrospective | Total #:645 | High resolution CT chest – thin section | GGO |
| Age:46.65+_13.82 | ||||||
| M/F:328/317 | ||||||
| 22 | Wu jing et al.(2020) [49] | China | retrospective | Total #:130 | High resolution CT chest – thin section | GGO, GGO with consolidation, interlobular septal thickening |
| Age:43+_15 | ||||||
| M/F:78/52 | ||||||
| 23 | Chun shuang guan et al.(2020) [50] | China | retrospective | Total #:53 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram, crazy paving |
| Age:42 | ||||||
| M/F:25/28 | ||||||
| 24 | Feng xiang song et al.(2020) [51] | China | retrospective | Total #:51 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram, crazy paving, interlobular septal thickening |
| Age:49+_16 | ||||||
| M/F:25/26 | ||||||
| 25 | Yu huan xu et al.(2020) [52] | China | retrospective | Total #:50 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram, interlobular septal thickening |
| Age:43.9+_16.8 | ||||||
| M/F:29/21 | ||||||
| 26 | Yicheng fang et al.(2020) [53] | China | retrospective | Total #:51 | High resolution CT chest – thin section | GGO, consolidation |
| Age:47 | ||||||
| M/F:29/22 | ||||||
| 27 | Wang et al.(2020) [34] | China | retrospective | Total #:114 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation |
| Age:53 | ||||||
| M/F:58/56 | ||||||
| 28 | Heshui shi et al.(2020) [54] | China | retrospective | Total #:81 | High resolution CT chest – thin section | GGO, air bronchogram, crazy paving, interlobular septal thickening |
| Age:49.5 | ||||||
| M/F:42/39 | ||||||
| 29 | Yang et al.(2020) [55] | China | retrospective | Total #:149 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation, air bronchogram |
| Age:45.11+_13.35 | ||||||
| M/F:81/68 | ||||||
| 30 | Pan et al.(2020) [9] | China | retrospective | Total #:63 | High resolution CT chest – thin section | GGO, GGO with consolidation, consolidation |
| Age:44.9+_15.2 | ||||||
| M/F:33/30 |
3.3. Radiological Findings from Included Studies
3.3.1. CT Scan as a Screening Tool – Typical Findings
After taking into consideration the initial radiological findings noted in the included studies(Table 3), it was observed that there was a proper spectrum to it which included a rainbow in the form of ground-glass opacities which were isolated, then ground-glass opacities which coexisted with consolidation, followed by isolated consolidation patches, air bronchogram, crazy paving appearance, and interlobular septal thickening with subpleural lines.
Ground glass opacities were defined as ill-defined hazy areas with increased attenuation where bronchial, as well as vascular margins, were intact. Consolidation was defined as intra alveolar air being replaced by abnormal fluid and tissue due to an increase in attenuation, rendering bronchial and vascular margins obscured. Crazy paving was defined as thickened interlobular septa with superimposition on a surrounding ground-glass opacity. Air bronchogram referred to an air attenuation bronchus on a background of the hyperattenuating opaque atelectatic lung. Subpleural line referred to a thin curvilinear opacity having a maximum width of 1 to 3 mm and located within a distance of 1 cm from the pleural surface and parallel to the adjacent pleural surface [18].
The total number of studies included in this systematic review article is 30 and the total number of cases reflected herein is 2327. Isolated ground-glass opacities were noted in 70.43% of cases (n=1639), ground-glass opacities coexisting with patchy consolidation were seen in 629 cases (27.03%), followed by isolated consolidation patches seen in 15.72%(n=366) cases.
3.3.2. CT Scan as a Diagnostic Tool – Atypical Findings
Other findings noted were interlobular septal thickening, crazy paving appearance and air bronchogram, which were noted in 312 (13.40%), 191 (8.20%), and 364 cases (15.64%), respectively. Subpleural lines were noted in 237 cases (10.18%).
The radiological findings which were far less common or atypically noted were pulmonary atelectasis(n=1, 0.04%), peribronchial thickening (n=38,1.63%), pleural effusion (n=72,3.09%), pericardial effusion (n=5,0.21%), mediastinal lymphadenopathy (n=36,1.54%), reverse halo or atoll sign defined as a focal rounded GGO surrounded by a more or less complete ring-like consolidation (n=9,0.38%), tree in bud appearance (n=2,0.08%) with bronchiectasis (n=88,3.78%) respectively. Amongst the included studies listed in Table 3, the total number of cases showing unilateral lung involvement was 19.03% (n=443) and those showing involvement of bilateral lungs were 74.17% (n=1726). Also, there was a number of cases that did not show any abnormal radiological findings on computed tomography in their initial scan (n=149, 6.40%) inspite of being tested positive for COVID 19 infection via real-time polymerase chain reaction testing.
The time period of the included cases from being tested positive for COVID-19 on RT-PCR testing and getting a CT chest done ranged in between 1 to 5 days.
Most of the included studies showed a predominant involvement of the peripheral one-third of the lung field irrespective of the laterality of the lesion with or without the involvement of the central two-thirds of bilateral lung fields. No isolated central lung involvement was noted in the included studies, which is consistent with the findings of Ooi GC et al. [18, 19] and Wong KT et al. [20].
| S. No. | Study ID (Year) | Total # of participants (N) | GGO without consolidation(n) | GGO with consolidation (n) |
consolidation (n) | air bronchogram (n) |
Crazy paving (n) |
Interlobular septal thickening (n) |
|---|---|---|---|---|---|---|---|---|
| 1 | K C Liu et al. (2020) [17] | 73 | 28 | 3 | 5 | 3 | 15 | 4 |
| 2 | JFW Chan et al.(2020) [25] | 5 | 5 | 3 | 3 | 3 | - | - |
| 3 | Chaolin Huang et al.(2020) [37] | 41 | 41 | 40 | 1 | - | - | - |
| 4 | Chunbao xie et al.(2020) [38] | 9 | 9 | - | - | - | - | - |
| 5 | Fang liu et al.(2020) [39] | 10 | 9 | - | 1 | - | - | - |
| 6 | Xi xu et al.(2020) [40] | 90 | 65 | - | 12 | - | 11 | 33 |
| 7 | Xiao wei et al.(2020) [41] | 62 | 52 | - | - | - | - | - |
| 8 | Yang s et al.(2020) [26] | 44 | 43 | - | - | 17 | - | - |
| 9 | Soon ho yoon et al.(2020) [27] | 9 | - | 9 | 1 | 2 | 1 | - |
| 10 | Mingli yuan et al.(2020) [28] | 27 | 18 | 8 | 5 | 8 | - | - |
| 11 | Li y et al.(2020) [42] | 51 | 18 | 28 | 3 | 35 | 36 | - |
| 12 | Chung m et al.(2020) [30] | 21 | 15 | 6 | 0 | 0 | 4 | - |
| 13 | Bernheim et al.(2020) [31] | 121 | 41 | 94 | 2 | - | - | - |
| 14 | Zhao et al.(2020) [32] | 101 | 87 | 65 | 44 | - | - | - |
| 15 | Xia w et al.(2020) [43] | 20 | 12 | - | 10 | - | 4 | - |
| 16 | Feng pan et al.(2020) [29] | 21 | 15 | - | 19 | - | 4 | - |
| 17 | Wei li et al.(2020) [44] | 5 | 3 | - | - | - | - | - |
| 18 | Han r et al.(2020) [45] | 108 | 65 | 44 | - | 52 | 43 | - |
| 19 | Xiong et al.(2020) [46] | 42 | - | 34 | - | 26 | - | 29 |
| 20 | Jiang wu et al.(2020) [47] | 80 | 73 | - | 50 | - | 23 | 47 |
| 21 | Xiaoli khang et al.(2020) [48] | 645 | 573 | - | - | - | - | - |
| 22 | Wu jing et al.(2020) [49] | 130 | 70 | 60 | - | - | - | 100 |
| 23 | Chun shuang guan et al.(2020) [50] | 53 | 47 | 8 | 30 | 36 | 42 | - |
| 24 | Feng xiang song et al.(2020) [51] | 51 | 38 | 30 | 28 | 41 | - | 38 |
| 25 | Yu huan xu et al.(2020) [52] | 50 | 30 | 25 | 15 | 22 | - | 33 |
| 26 | Yicheng fang et al.(2020) [53] | 51 | 36 | - | 14 | - | - | - |
| 27 | Wang et al.(2020) [34] | 114 | 30 | 50 | 30 | - | - | - |
| 28 | Heshui shi et al.(2020) [54] | 81 | 53 | - | - | 38 | 8 | 28 |
| 29 | Yang et al.(2020) [55] | 149 | 149 | 68 | 81 | 81 | - | - |
| 30 | Pan et al.(2020) [9] | 63 | 14 | 54 | 12 | - | - | - |
4. DISCUSSION
In the present study, 70.43% of cases presented with ground glass opacities in isolation as the most common and frequent radiological finding, followed by 27.03% and 15.72% cases presenting with ground glass opacities in coexistence with patchy areas of consolidation and isolated patches of consolidation without ground-glass opacities, respectively. This resultant finding can be seen to envisage computed tomography as a perfect screening tool for investigating suspected cases.
According to an article published by theprint.in online (reference), the present scenario of COVID 19 in India states certain bitter facts that may prove true sooner than later if the present situation does not get hilted properly. According to its author, “It took India forty days to reach the first 50 cases, five more days to reach 100 cases, three more days to reach 150 cases and then just two more days to reach 200 cases.” It states that India has already hit the phase where it is showing exponential growth in the number of patients infected with COVID 19 disease, with special emphasis upon the meagre number of beds available per 1000 people in different states. According to the declared statistics in 2017, the official overall number of beds available per 1000 people in India is as less as 0.5. It also reinforces the fact that the rate of doubling of cases in India is as present about 5 days or less and, in not much later timeframe, it will grow less, putting India upon the same trajectory of affected cases as the USA where the same rate is about 2 days. At this rate, it is going to be a very difficult time to handle such cases for Indian healthcare workers [21].
Coming to the radiological front, according to a Fleischner Society consensus statement published on April 07, 2020 [22]:
- Imaging is not indicated in suspected cases of COVID 19 until and unless there is a potential risk of worsening of the disease.
- It is strongly indicated in positive COVID 19 case with deteriorating respiratory status.
- Imaging is indicated for medical triage of suspected COVID 19 cases with moderate to severe spectrum of clinical findings with high disease probability before the diagnostic test has been carried out.
Computed tomography of the chest is a strongly advised modality that can be used to screen cases affected by COVID 19 infection as well as for suspected cases that happen to come under the above-mentioned criteria by Fleischner [7, 22].
The main presenting features noted in a patient of COVID 19 are fever, dry cough with or without a sore throat, muscle fatigue, sputum production, and difficulty in breathing. Also, the patients of COVID 19 who succumbed to its brute nature either belonged to the age group of more than 60 years of age or had one or the other comorbidities, such as diabetes mellitus and hypertension being the most common ones [23].
The typical radiological findings noted in chest computed tomography are of ground-glass opacities which were isolated, then ground glass opacities which coexisted with consolidation, followed by isolated consolidation patches, air bronchogram, crazy paving appearance, interlobular septal thickening with subpleural lines. With the progression of the disease, other atypical radiological findings are noted, such as pulmonary atelectasis, peribronchial thickening, pleural effusion, pericardial effusion, mediastinal lymphadenopathy, reverse halo or atoll sign, and tree in bud appearance with bronchiectasis. The appearance of atypical findings denotes the progression of the disease with an added possibility of superadded bacterial infection giving rise to focal enlargement of mediastinal lymph nodes.
There are two zoonotic viruses from the family of coronaviruses that affect humans – COVID 19 being caused by one of them and the other one being Middle East Respiratory Syndrome virus. Both of these give a presentation of viral pneumonia in the affected lungs. As per Cotran, there are 4 stages of pneumonia – congestion, red hepatization or consolidation, grey hepatization, and lastly, resolution. Different types of viral pneumonia affect different areas, but the timeline progression of lung tissue damage and recovery is more or less the same throughout. The progression is chronological from the stage of congestion, which is marked by vascular engorgement around the pulmonary alveoli with intra alveolar fluid leak. The second stage sees an increase in vascular engorgement and congestion with leakage of blood cells into the intra alveolar fluid. This blood being rich in fibrin leads to a collectively hyperdense appearance to the affected part of the lung – solidification or consolidation. The third stage, called grey hepatization, sees the degeneration of these existing blood cells and deposition of fibrin in the intra alveolar compartment, the lung still giving consolidated appearance. Lastly, the stage of resolution sees the development of pulmonary fibrosis – marking the phase of recovery of affected lung tissue [24].
Amongst the included studies, COVID 19 was graded by KC Liu into the mild type, common type, severe type, and the critical type. Mild type was defined as a case showing lung hilar enlargement with thickening of lung texture. The common type was defined as patchy GGO with crazy paving, air bronchogram, and interlobular septal thickening. The severe type was defined as extensive multilobular GGO, pulmonary consolidation, and peribronchial thickening. The critical type was defined as confluent GGO with pulmonary atelectasis, pleural effusion, and pulmonary fibrosis. They concluded that the size of the lesion as well as the type of the lesion is in direct proportion with the severity of the presenting disease. Also, they concluded that the disease severity also lies in direct proportion with the patient's age [17].
Viral load of COVID 19 was reflected in the study by JFW Chan, indicating that the cycle threshold values for samples from patient sputum were 8-13 cycles earlier than samples taken from nasopharyngeal swabs meaning higher viral load of the present disease causative agent in the lower respiratory tract which can be regarded as a point of similarity between COVID 19 and MERS. Also, the viral load was noted in the stool samples of the included cases, indicating a possible fecal-oral route of infection for COVID 19 [25].
Yang S et al. graded the included cases in their study into 4 types on the basis of their type and size. Type 1 was defined as pure GGO with a mean lesion size of 1.37+_1.08cm. Type 2 was defined as GGO with pulmonary consolidation having a mean lesion size of 2.12 +_2 cm. Type 3 was defined as GGO with interlobular septal thickening having a mean size of 4.7 +_2.58 cm. Type 4 was defined as pure wide consolidation with a mean lesion size of 1.52+_0.88cm [26].
A study conducted by Soon Ho Yoon et al. in Korea, the only study in this systematic review outside of China, graded the disease on a 5 point scale – 1 as normal findings, 2 as patchy GGO with or without hyperinflation with or without bronchial wall thickening, 3 as unifocal alveolar consolidation in a single lung segment or a lung lobe, 4 as multifocal alveolar consolidation in multiple lung segments or lung lobes whereas 5 as diffuse alveolar consolidation [27]. Out of the included 2327 patients, 10 patients died. These were reported in a study conducted by Mingli Yuan et al. with the study mortality rate being equal to 2.7% [28]
Another study by Feng Pan et al. graded COVID 19 cases on the basis of patient quartiles observed from the day of first CT examination of chest till the 26th day as follows: Stage 1 (0-4 days): ground-glass opacities (GGO); Stage-2 (5-8d days): increased crazy-paving pattern 9; Stage-3 (9- 13days): consolidation; Stage-4 (≥14 days): gradual resolution of consolidation without crazy-paving pattern [29].
Taking selective involvement of lung lobes, a study conducted by Chung M et al. reported that the right lower lobe was the most affected, followed by right upper, left upper, and left lower lobes equally [30]. On the same note, Bernheim reported that the most affected lung lobe was the right lower lobe, followed by the left lower lobe, left upper lobe, right upper lobe and right middle lobe at last [31]. Therefore, the right lower lobe was reported as the most affected lobe in 2 different independent retrospective studies.
The role of computed tomography as a screening modality remains incomplete without proper points of differentiation of COVID 19 from its distant relatives – adenovirus pneumonia, H1N1 influenza, SARS, and MERS. There are some points of differentiation, which are subtle but notable. Adenovirus pneumonia mostly affects children and presents with pleural effusion, pneumothorax, enlargement of lung hila, emphysematous changes in both mediastinum as well as the subcutaneous planes [32].
Typical CT features in H1N1 influenza include GGO and consolidation along with peribronchial thickening, whereas those of SARS include large areas of consolidation along with air bronchograms [33, 34]. MERS-CoV shows ground-glass opacity followed by consolidation. Both ground-glass opacity and consolidation are apparent in 1/10 th of cases. Consolidation can be patchy, confluent, or nodular with an intertwined air bronchogram, as well as a peripheral mid lung zone and peripheral lower lung zone predominance with lung parenchymal abnormalities eventually spreading to the central area and bilateral upper lobes. Unifocal involvement is more common than multifocal involvement [35, 36].
Therefore, it is clear that there exists an increasing resemblance between the radiological features of these two siblings – COVID 19 and MERS CoV apart from a single feature that unifocal involvement is more common in MERS, which is quite the opposite in the case of COVID 19. It is on this note that computed tomography of the chest derives its importance as a screening modality and makes itself well accounted for in this perspective.
5. STUDY LIMITATIONS
Most of the included studies were limited in terms of proper demographic details as well as the availability of data and detailed methodology therein.
CONCLUSION
This systematic review article aims at disseminating and clarifying the initial presenting radiological features on computed tomography scan of the chest in an RT-PCR positive case, providing a map for the radiologist to diagnose COVID 19 and help in differentiating it from its potential mimics, planning further treatment and management of such cases, thus cementing its position as a priceless screening modality for the same.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


