All published articles of this journal are available on ScienceDirect.
Knowledge and Perceptions Regarding the use of Antibiotics and Self-diagnosis: A Comparative Study of the Urban and Suburban Communities in Karawang, Indonesia
Abstract
Background:
To avoid antibiotic resistance, acute respiratory infections (ARIs) require the use of appropriate antibiotics. As a result, having the appropriate knowledge and perceptions is critical for achieving successful clinical outcomes.
Objective:
The purpose of this study was to determine the relationships and differences in knowledge and perceptions about antibiotics and ARI in urban and suburban communities in the Karawang Regency of West Java Province, Indonesia.
Methods:
We used a validated questionnaire approach to conduct a cross-sectional study in primary health care facilities. We surveyed 440 respondents from urban areas and 464 respondents from suburban areas.
Results:
Respondents in both urban and suburban areas agreed that self-diagnosis should not be used to prescribe antibiotics. False knowledge and perceptions about antibiotic use were more prevalent in suburban respondents than urban respondents. Additionally, a significant correlation between education levels and knowledge and perception was observed in both areas. Furthermore, significant correlations between age and occupation, as well as knowledge and perceptions, were identified in urban areas.
Conclusion:
Our study suggests that additional efforts are needed to increase awareness and ensure appropriate antibiotic use in the community.
1. INTRODUCTION
In 2013, the prevalence of acute respiratory infection (ARI) was approximately 25% [1], and the incidence of ARI in West Java Province, Indonesia’s most populous province, is currently the highest among other diseases, with a prevalence of 33.44% in the Karawang Regency [2]. According to the data from disease eradication programs, there were 14,397 patients diagnosed with ARI in Karawang Regency in 2014 and 175,891 in 2016 [3]. Even without a prescription, antibiotic use is common in patients with respiratory tract infections [4]. Increased antibiotic consumption in patients with ARI results in a 50%–100% increase in excessive and irrational antibiotic use in various countries [5]. Additionally, antibiotics comprised 33% of the total prescriptions that were prescribed to outpatients at Abepura General Hospital [6]. It is, therefore, critical to evaluate inappropriate and excessive antibiotic use to avoid drug resistance, as 90% of antibiotics used were amoxicillin, ciprofloxacin, and cefadroxil [7]. This is because improper antibiotic use can increase mortality, morbidity, and financial costs while contributing to antibiotic resistance [8]. This is a major global concern and a persistent problem in several developing countries, including Indonesia [9, 10], where 84% of hospitalized patients are prescribed antibiotics, with 46% of the prescription being inappropriate [11].
Antibiotic misuse indicates a general lack of education and knowledge on the subject [12]. Knowledge regarding antibiotics has been found to be significantly associated with demographic characteristics such as gender, race, education level, and health care occupation [13]. In comparison, inadequate antibiotic knowledge has been associated with inappropriate and erroneous antibiotic use behaviors and perceptions regarding ARI [14]. Additionally, education, occupation, age, interests, experiences, culture, and information have the potential to improve knowledge [15].
The purpose of this study was to examine the relationships and differences in knowledge and perception regarding antibiotics for ARI in urban and suburban communities in the Karawang Regency of Indonesia.
2. METHODS
2.1. Study Design
2.1.1. Knowledge and Perception Regarding Antibiotics - Measurements
The data was collected using questionnaires adapted from Fredericks et al. ’s study [14]. Validation of the questionnaire indicated that all items had a validity coefficient > 0.30, a p-value < 0.05, and Cronbach’s alpha coefficient > 0.700, indicating that our approach was reliable and valid. The research collected data on the demographics, knowledge, and perceptions of respondents.
2.2. Statistical Analysis
A univariate analysis was performed to evaluate respondents’ demographics, knowledge, and perceptions. Bivariate analysis was used to determine the differences and correlations between these variables. The Kolmogorov-Smirnov test was used to determine the data normality, and the Chi-square test was used to determine the group differences. Furthermore, the Kruskal Wallis test was performed to determine potential correlations between groups regarding antibiotic knowledge and perceptions.
3. RESULTS
3.1. Respondent Demographics
As indicated in Table 1, the following demographic variables were collected: gender, age, education level, occupation, income, and health insurance status. The highest percentage of respondents was females (p > 0.05). The age group of 25–44 years had a significantly higher response rate (p < 0.05). In urban areas, the highest percentage of respondents (42.05%) had completed senior high school, compared to suburban areas, where the highest percentage (56.03%) had completed elementary school (p < 0.05). This report corroborates the findings of the 2015 Karawang Performance Report, which indicated that the level of education in Karawang is quite low (elementary school level). According to Indonesian statistics from 2015, people over the age of ten with a lower or elementary school education or equivalent made up 57.92% of the total population (1,094,940 out of 1,890,426 people) [16, 17]. Urban and suburban respondents had significantly different occupations and incomes (p < 0.05), with respondents in urban areas having significantly higher incomes than those in suburban areas.
Table 1.
| Characteristics | Urban (n = 440) | Suburban (n = 464) | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Gender | 0.328 | ||||
| Female | 299 | 68.0 | 300 | 64.66 | |
| Male | 141 | 32.0 | 164 | 35.34 | |
| Age | 0.002 | ||||
| 18–24 years | 81 | 18.41 | 53 | 11.42 | |
| 25–44 years | 238 | 54.09 | 244 | 52.59 | |
| 45–54 years | 69 | 15.68 | 119 | 25.65 | |
| 55–64 years | 32 | 7.27 | 32 | 6.90 | |
| 65–74 years | 16 | 3.64 | 14 | 3.02 | |
| >75 years | 4 | 0.91 | 2 | 0.43 | |
| Education level | 0.000 | ||||
| Not completed primary school | 0 | 0 | 21 | 4.53 | |
| Elementary School | 101 | 22.95 | 260 | 56.03 | |
| Junior High School | 111 | 25.23 | 94 | 20.26 | |
| Senior High School | 185 | 42.05 | 77 | 16.59 | |
| Vocational School | 21 | 4.77 | 8 | 1.72 | |
| Bachelor and Postgraduate Degree | 18 | 4.09 | 4 | 0.86 | |
| Others | 4 | 0.91 | 0 | 0 | |
| Occupation | 0.000 | ||||
| Student | 8 | 1.82 | 2 | 0.43 | |
| Teacher/Lecturer | 11 | 2.50 | 4 | 0.86 | |
| Private employee | 68 | 15.45 | 23 | 4.96 | |
| Employer/Self-Employed | 74 | 16.82 | 65 | 14.01 | |
| Civil servant/Police/Military | 10 | 2.27 | 3 | 0.65 | |
| Not working | 242 | 55.00 | 251 | 54.09 | |
| Laborer | 0 | 0 | 58 | 12.50 | |
| Others | 27 | 6.14 | 58 | 12.50 | |
| Monthly Income | 0.000 | ||||
| ≤ 85.99 USD | 151 | 34.32 | 264 | 56.90 | |
| 85.99–240.76 USD | 179 | 40.68 | 155 | 33.41 | |
| ≥ 240.76 USD | 110 | 25 | 45 | 9.70 | |
| Health insurance | |||||
| Yes | 265 | 60.2 | 291 | 62.72 | 0.363 |
| No | 175 | 39.8 | 173 | 37.28 | |
3.2. Antibiotics Knowledge and Perception
Table 2 shows the respondents’ knowledge and perception of ARI. We observed differences in knowledge and perceptions between urban and suburban areas (p < 0.05) that were related to physicians’ diagnoses before antibiotic use. Furthermore, our results showed that there was no statistically significant difference in knowledge and perception regarding what constitutes a correct therapy (p > 0.05). We also categorized respondents into groups (Table 2) based on their knowledge and perceptions related to self-diagnosis or non-self-diagnosis and correct or incorrect self-diagnosis (Fig. 1).
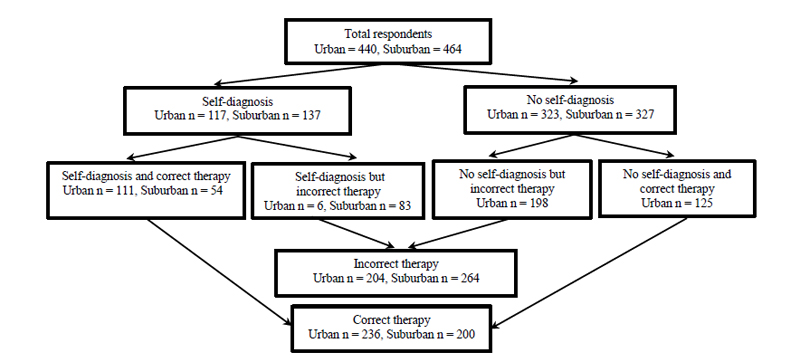
We also recorded data on incorrect ARI knowledge and perceptions from 204 and 264 respondents in urban and suburban areas, respectively, whereas correct ARI knowledge and perceptions were identified in 236 and 200 respondents, respectively, thus highlighting significant differences between urban and suburban areas (p < 0.005). Table 3 demonstrates differences in knowledge and perception regarding self-diagnosis or non-self-diagnosis in urban and suburban areas (Table 3).
| Statement | Area | Responses and number of respondents (percentages) | p-value | ||||
|---|---|---|---|---|---|---|---|
| Strongly agree | Agree | Not sure | Disagree | Strongly disagree | |||
| I know I need antibiotics before I visit my doctor* | Urban (n = 440) |
12 (2.73%) |
105 (23.86%) |
41 (9.32%) |
271 (61.59%) |
11 (2.5%) |
0.000 |
| Suburban (n = 464) |
15 (3.23%) |
122 (26.29%) | 49 (10.56%) |
195 (42.03%) |
83 (17.89%) |
||
| I will recover faster if I take antibiotics when I have a cold or flu+ | Urban (n = 440) |
97 (22.05%) |
180 (40.91%) |
48 (10.91%) |
102 (23.18%) |
13 (2.95%) |
0.310 |
| Suburban (n = 464) |
88 (18.97%) |
176 (37.93%) |
50 (10.78%) |
136 (29.31%) |
14 (3.02%) |
||
| Respondent Groups | I know I need antibiotics before I visit my doctor* | I will recover faster if I take antibiotics when I have a cold or flu+ | Antibiotics cure most bacterial infections | Antibiotics cure all viral infections | Antibiotics have side effects | Resistant bacteria are difficult to treat with antibiotics | Resistant bacteria are found in hospitals and the general public | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urban | Sub Urban |
Urban | Sub urban |
Urban | Sub urban |
Urban | Sub urban |
Urban | Sub urban |
Urban | Suburban | Urban | Suburban | ||
| Self- diagnosis | Mean ± SD | - | 22.82 ± 11.73 |
24.82 ± 12.13 | 23.50 ± 10.53 |
20.15 ± 8.31 |
24.70 ± 10.63 | 23.80 ± 8.92 | 29.06 ± 10.34 | 33.58 ± 11.16 | 24.96 ± 12.84 | 28.39 ± 11.00 | 24.79 ± 11.42 |
25.62 ± 9.92 | |
| No self-diagnosis |
Mean ± SD | - | 24.98 ± 11.43 |
26.42 ± 11.63 |
25.51 ± 9.75 |
21.87 ± 8.09 |
26.47 ± 8.66 | 25 ± 10.38 |
31.08 ± 11.27 | 31.16 ± 11.66 | 21.95 ± 10.35 | 26.18 ± 10.58 |
21.86 ± 9.37 |
24.28 ± 9.10 |
|
| Differences between self-diagnosis and no self- diagnosis | Mean difference p-value** |
- - |
2.16 0.06 |
1.60 0.182 |
2.01 0.03** |
1.72 0.039** |
1.77 0.03** |
2.04 0.045** |
2.02 0.07 |
2.42 0.040** |
3.01 0.05** |
2.21 0.042** |
2.93 0.02** |
1.34 0.160 |
|
| Incorrect therapy | Mean ± SD | 32.44 ± 8.16 | 34.36 ± 11.55 |
- | - | 23.27 ± 7.31 |
20.57 ± 7.95 |
25.66 ± 9.14 | 24.43 ± 9.77 | 31.85 ± 9.88 | 33.41 ± 11.12 |
25.37 ± 9.47 | 29.43 ± 11.14 |
23.80 ± 7.22 |
25.80 ± 9.83 |
| Correct therapy | Mean ± SD | 30.04 ± 12.99 | 34.7 ± 11.51 |
- | - | 24.85 ± 7.35 |
22.40 ± 8.40 |
23.74 ± 9.41 | 26.30 ± 10.24 | 30.04 ± 11.27 | 29.85 ± 11.84 | 23.45 ± 10.15 | 23.40 ± 9.16 |
22.64 ± 9.51 |
23.20 ± 8.49 |
| Differences between correct and incorrect therapy | Mean difference p-value** |
2.40 0.05** |
0.34 0.751 |
- - |
- - |
1.56 0.003** |
1.83 0.013++ |
1.91 0.041** |
1.37 0.046** |
1.81 0.08 |
3.56 0.001** |
1.92 0.03** |
6.03 0.000** |
1.17 0.039** |
2.60 0.003** |
| Self-diagnosis and incorrect therapy |
Mean ± SD | - | - | - | 22.18 ± 9.82 |
19.88 ± 7.24 |
23.68 ± 9.29 | 22.77 ± 8.16 | 29.43 ± 9.07 | 35.54 ± 9.53 | 24.14 ± 11.77 | 31.57 ± 10.76 |
21.95 ± 9.75 |
27.47 ± 9.98 |
|
| Self-diagnosis and correct therapy |
Mean ± SD | - | - | - | 23.60 ± 8.29 |
20.56 ± 9.79 |
26.67± 7.30 | 25.37 ± 9.85 | 31.17 ± 9.02 | 30.56 ± 12.80 | 26.67 ± 8.98 | 23.52 ± 9.55 |
20.99 ± 7.86 |
22.78 ± 9.20 |
|
| No self-diagnosis and incorrect therapy |
Mean ± SD | - | - | - | 24.41 ± 8.12 |
20.88± 8.25 |
26.78 ± 9.33 | 25.19 ± 10.36 | 29.07 ± 10.70 | 32.43 ± 11.67 | 23.05 ± 11.51 | 28.45 ± 11.20 |
26.02 ± 10.14 |
25.03 ± 9.7 |
|
| No self-diagnosis and correct therapy |
Mean ± SD | - | - | - | 28.71 ± 11.96 |
23.08± 7.75 |
26.29 ± 10.47 | 26.64 ± 10.39 | 32.18 ± 13.83 | 29.59 ± 11.50 | 17.98 ± 10.44 | 23.36 ± 9.04 |
21.37 ± 11.14 |
23.36 ± 8.24 |
|
| All respondents | Mean ± SD p-value++ |
- - |
- - |
24.98 ± 9.99 0.00++ |
21.51± 7.49 0.016++ |
26.00 ± 9.25 0.062 |
25.02 ± 9.84 0.047 |
30.55 ± 11.06 0.081 |
31.88 ± 11.56 0.002++ |
22.75 ± 11.13 0.00++ |
26.88 ± 10.76 0.000++ |
22.64 ± 10.03 0.00++ |
24.68 ± 9.36 0.005++ |
||
Based on independent t-tests, we observed significant differences (p < 0.005) between the self- and non-self-diagnosis groups in terms of knowledge and perceptions related to antibiotics in both communities. Data included the antibiotics’ ability to treat bacterial and/or viral infections and the notion that resistant bacteria were difficult to treat with antibiotics. More specifically, our results indicate that urban communities exhibited no differences in knowledge and perceptions regarding antibiotics having side effects (p > 0.005), whereas differences were recorded in the suburban areas (p < 0.005). Furthermore, differences in knowledge and perception regarding resistant bacteria in hospitals and the general public were recorded in the suburban communities (p < 0.005).
In both correct and incorrect groups pertaining to their ARI knowledge and perceptions, we observed significant differences (p < 0.005) in both urban and suburban communities regarding the knowledge that antibiotics can treat most bacterial infections, antibiotics can be used for all viral infections, and resistant bacteria were difficult to treat with antibiotics and the knowledge of resistant bacteria in hospitals and the general public. Moreover, we did not find any significant differences in knowledge and perception regarding antibiotic side effects in the urban areas, as opposed to the suburban areas where significant differences were noted.
Based on the Kruskal Wallis analyses to determine knowledge and perception differences in all respondents (self-diagnosis but incorrect therapy, self-diagnosis, and correct therapy, no self-diagnosis but incorrect therapy, no self-diagnosis, and correct therapy), no significant differences were recorded regarding the statement that antibiotics could induce side effects. Correlations between respondents’ characteristics and knowledge, and perceptions from each area are described in Table 4.
| Characteristics | Respondent groups | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Self-diagnosis and correct therapy |
No self-diagnosis but incorrect therapy | Self-diagnosis but incorrect therapy | No self-diagnosis and correct therapy | p-value | |||||||
| Urban | Suburban | Urban | Suburban | Urban | Suburban | Urban | Suburban | Urban | Suburban | ||
| Gender | |||||||||||
| Female | 70 | 51 | 85 | 35 | 65 | 111 | 79 | 103 | 0.17 | 0.325 | |
| Male | 41 | 32 | 33 | 19 | 22 | 70 | 45 | 43 | |||
| Age Group | |||||||||||
| 18–44 years | 76 | 54 | 85 | 35 | 51 | 116 | 103 | 92 | 0.002 | 0.559 | |
| 45–64 years | 31 | 29 | 27 | 17 | 26 | 59 | 17 | 46 | |||
| ≥65 years | 4 | 0 | 6 | 2 | 7 | 6 | 4 | 8 | |||
| Education level | |||||||||||
| Did not finish elementary school | 0 | 5 | 0 | 1 | 0 | 11 | 0 | 4 | 0.005 | 0.011 | |
| Elementary School | 32 | 45 | 24 | 35 | 32 | 100 | 13 | 78 | |||
| Junior High School | 22 | 18 | 34 | 14 | 20 | 38 | 35 | 24 | |||
| Senior High School | 47 | 13 | 50 | 1 | 28 | 27 | 60 | 36 | |||
| Vocational School | 6 | 0 | 4 | 3 | 2 | 4 | 9 | 1 | |||
| Bachelor and Postgraduate degree | 3 | 0 | 5 | 0 | 3 | 1 | 7 | 3 | |||
| Others | 1 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | |||
| Occupation | |||||||||||
| Student | 0 | 0 | 4 | 0 | 3 | 0 | 1 | 2 | 0.036 | 1. 0.235 | |
| Teacher/Lecturer | 2 | 1 | 3 | 2 | 2 | 1 | 4 | 0 | |||
| Private Employee | 12 | 4 | 13 | 3 | 15 | 9 | 28 | 7 | |||
| Employers/Self-Employed | 21 | 11 | 20 | 7 | 13 | 34 | 20 | 13 | |||
| Civil Servants/Police/Military | 0 | 0 | 5 | 1 | 1 | 1 | 4 | 1 | |||
| Housewife | 73 | 49 | 64 | 29 | 46 | 87 | 59 | 86 | |||
| Laborer | 0 | 7 | 0 | 9 | 0 | 23 | 0 | 19 | |||
| Others | 3 | 11 | 9 | 3 | 7 | 26 | 8 | 18 | |||
| Income | |||||||||||
| <Rp 1,250,000 | 42 | 47 | 35 | 32 | 34 | 95 | 40 | 90 | 0.401 | 0.380 | |
| Rp 1,250,000–Rp 3,500,000 | 44 | 24 | 57 | 18 | 29 | 70 | 29 | 43 | |||
| ≥Rp 3,500,000 | 25 | 12 | 26 | 4 | 25 | 16 | 35 | 13 | |||
| Health insurance | |||||||||||
| Yes | 62 | 53 | 64 | 32 | 60 | 116 | 79 | 90 | 0.106 | 0.910 | |
| No | 49 | 30 | 54 | 32 | 27 | 65 | 45 | 56 | |||
In urban areas, we observed significant correlations (p < 0.005) between age and occupation and knowledge and perception, whereas, in suburban areas, no differences were found. In both areas, the education level was significantly correlated with knowledge and perception, as opposed to gender, income, and insurance status.
4. DISCUSSION
It is critical to conduct community studies to ascertain public knowledge and perceptions about antibiotics in ARI. According to a recent study, 79% of 203 patients taking ARI antibiotics used their medication incorrectly [18]. This erroneous use, likely to result in antibiotic resistance and exacerbate disease severity [19, 20], appears to be defined by community knowledge and perceptions on the subject [13].
In urban areas, the proportion of respondents with incorrect knowledge and perception was lower than the proportion with correct responses, whereas, in suburban areas, the situation was completely reversed. This is in accordance with a previous study, wherein the respondents in suburban areas used antibiotics when they suffered from flu [4]. According to Oh et al., 67.2% of their study respondents believed antibiotics could be used to treat viral infections and were unable to differentiate between viral and bacterial diseases [21].
Although antibiotics are not always necessary, they are frequently used in patients with respiratory infections [22, 23]. Our study found no correlation between respondents' age and their antibiotic knowledge and perceptions. An Australian study reported no significant correlations between age, public knowledge, and perception regarding antibiotic use [14]. Additionally, an Ecuadorian study found that mothers (respondents) aged 18–44 years had a higher level of knowledge about antibiotic use in children than mothers (respondents) aged <18 years [24]. Another study conducted in Jordan found that respondents aged 18–39 took improved self-medication measures, particularly concerning antibiotics, and that age was associated with antibiotic use [25]. Conversely, education levels were found to be significantly associated with antibiotic knowledge and perceptions. In this regard, a recent study also reported similar correlations between education and knowledge regarding antibiotic use [26]. Similarly, our findings indicate that respondents with lower educational attainment and those living in rural areas had significantly lower levels of knowledge about antibiotics [27]. Additionally, a European study suggested that respondents with low levels of education harbor a decreased awareness regarding antibiotics [28].
Thus, the level of education of respondents was found to be associated with their knowledge and perceptions about antibiotics. Previous research has revealed a knowledge and perception gap between communities and health care providers [13]. One factor influencing knowledge is occupation, implying that individuals may gain experience and knowledge through their work environments [15].
However, there was no correlation between knowledge and perception, and income [29]. Additionally, we observed no correlation between health insurance status and knowledge and perceptions of antibiotic use. However, previous studies have demonstrated that patients without health insurance exhibited inappropriate behaviors concerning antibiotic use [30]. Thus, health insurance may play a significant role in determining antibiotic use and associated erroneous practices [11]. On the other hand, in rural communities in China, some parents demonstrated a lack of knowledge about antibiotics while harboring a high prevalence of self-medicating their children with antibiotics [31].
The current study also examined subjects’ knowledge and perceptions regarding antibiotics, which can be influenced by geographical factors. Simandan (2016) explained that certain distances and geographic locations affect the subjectivity and objectivity of knowledge and perception. Additionally, the uncertainty of factors such as positionality, partiality, reflexivity, crossing, and strongly politicalized positioning aided in subject knowledge. In another study, Simadan (2020) confirmed the role of geography and diversity in personal and social change [32-34].
LIMITATION OF STUDY
As is the case with the majority of studies that rely on self-reported measures, the accuracy of respondents’ data is difficult to verify. Additional techniques, such as interviews, could be used to gain a complete understanding of the factors that influence students’ attitudes. It is likely that a variety of different attitude responses remain undiscovered in this area. Furthermore, our study relied on a self-administered questionnaire, which could have introduced subjectivity bias.
CONCLUSION
Our study used a self-administered questionnaire, and data were derived from respondents’ recall and memory. While this may introduce some subjectivity, the data indicated that respondents in both urban and suburban areas generally agree that antibiotics should not be taken based on self-diagnosis. Consequently, it is necessary to increase awareness and promote the proper use of antibiotics in the community.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Ethical Board for Health Research of Universitas Padjadjaran (registration number: 876/UN6.C.10PN/2017), Indonesia.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written and informed consent was obtained from the participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from the corresponding author on request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


