All published articles of this journal are available on ScienceDirect.
The Impact of The COVID-19 Pandemic on the Management of Chronic Disease in South Africa: A Systematic Review
Abstract
Introduction:
The abrupt development of the coronavirus (COVID-19) pandemic has posed a threat to persons with chronic diseases' compliance with treatment, which is critical to improving their health, life expectancy, and lowering death and morbidity rates. The public health control measures for the pandemic have been heavily politicized. The focus on the COVID-19 epidemic has resulted in a neglect for chronic disease management. As a result, the goal of this study was to review the literature in order to gain a broader perspective on how the COVID-19 pandemic has impacted chronic disease management, as well as to investigate various strategies to deal with similar occurrences in the future when faced with medical emergencies, in order to reduce the potential harm of these measures to non-communicable disease control.
Methodology:
To analyze and identify full-text studies relevant to the influence of COVID-19 on the management of chronic diseases conducted in an African environment from 2019 to 2021, the suggested reporting items for systematic reviews and meta-analyses were used. Six databases were searched to find relevant studies, which include CINAHL Plus (EBSCO), PubMed, Google Scholar, Medline, ProQuest, and APA PsychINFO. Researchers performed a quality assessment for each included paper prior to data synthesis, as well as a formal risk-of-bias assessment.
Results:
Out of 119 abstracts reviewed, 17 full-text studies were included. Three themes were identified: the impact of COVID-19 on the healthcare system; the psychological impact on people with chronic diseases and healthcare providers; and the digitalization of healthcare services. The majority of studies were conducted in South Africa and other African countries in collaboration with western countries. The majority of studies focused on lessons learned during periods of strict public health measures, however a few empirical investigations of patients or healthcare providers were done. It is recommended that African countries should develop an integrated community-based non-communicable disease (NCD) and infectious disease care model and protocols, initiate innovative ways of central dispensing, pre-packaging and home delivery of medications to stable patients, use of telemedicine, and emphasize mental health services during medical emergencies.
Contribution:
The study’s findings could improve policy implementation regarding the management of chronic diseases during a medical emergency; in this case, COVID-19. It could also improve self-care management. The main goal is to maintain adherence and compliance with treatment to reduce complications and the disease burden. The study mainly focused on the African context.
Conclusion:
The literature revealed that the COVID-19 pandemic has had a severe impact on the management of chronic diseases and disrupted access to related healthcare services in terms of prevention, diagnosis, routine clinical care, and self-care. In addition, the mental health of both patients and healthcare providers has been affected. Chronic diseases should also be considered a public health emergency and should be given the same attention and priority as infectious diseases during a pandemic to reduce the burden of disease, especially in low and middle-income African countries already experiencing a shortage of resources. Rather than depending on the researcher's opinion, viewpoint, and notes taken during the COVID-19 lockdown, primary investigations should be done to address the inadequacies brought to light on the management of chronic diseases due to COVID-19.
1. INTRODUCTION AND BACKGROUND
Chronic diseases are the leading cause of death and disability worldwide and account for 80% of deaths in people with chronic diseases [1]; moreover, this threat is growing, especially in low-and middle-income countries (LMICs) instead of achieving the goal of reducing death by 2% through comprehensive and integrated actions at a country-led level [2]. The abrupt emergence of the virus known as COVID-19 has disrupted the access to and utilization of priority programs and services worldwide due to the implementation of lockdown regulations [3]. Even though the chronic disease is one of the priority programs aimed to reduce the burden of disease, the current management measures for COVID-19 prevention are not in compliance with the World Health Organization’s (WHO’s) approach for the prevention, control, and management of chronic diseases [3]. In South Africa, the COVID-19 pandemic control was highly politicized; this has exerted even more pressure on the country’s healthcare system which is already overwhelmed by the burden of diseases, which include the human immunodeficiency virus (HIV, acquired immune deficiency syndrome (AIDS), tuberculosis (TB), diabetes mellitus (DB), cardiovascular disease, cancer and hypertension (HPT) [4]. HIV and non-communicable diseases (NCDs) are more prevalent in LIM countries, mainly in sub-Saharan Africa [5]. According to [6], out of 56 million deaths reported globally, 38 million were associated with NCDs, which raised from 59% in 2002 to 69% in 2010. The number of people living with HIV (PLHIV) increased from 31 million in 2010 to 38 million in 2018, even though there has been a significant improvement since 2017, 50% of new HIV infections have occurred among important populations [5, 7]. According to [6], NCDs are usually neglected during medical emergencies since the focus would be on infectious disease outbreaks and such NCDs are not taken into consideration as part of emergency response [5, 7]. HIV and NCDs are now regarded as major chronic diseases of public concern, especially in lower-middle-income (LMI) countries [8]. The sudden shift in healthcare priorities was observed when countries were trying to curb the spread of COVID-19. Such disruptions to health priorities affect people with chronic diseases [9]. In addition, traveling was banned and changes in the operation of transport services affected the access [10, 11]. Fear and feelings of uncertainty among healthcare providers (HCPs) and the community about the disease were observed as there was not enough information regarding the surveillance, prevention, control, and management of COVID-19. Furthermore, compliance and retention to care and treatment were disrupted and identified through a high number of missed appointments. Consequently, this has prompted the researchers to conduct a detailed study investigating the impact of the COVID-19 pandemic on the management of chronic diseases in South Africa and the African healthcare community, aimed at mitigating the potential harm of the pandemic’s public health measures to NCD control.
2. AIM OF THE STUDY
The goal of the study was to review the available literature to obtain a broader perspective on the impact of the COVID-19 pandemic in the management of chronic diseases, which include HIV and NCDs to propose strategies to policymakers, patients and HCPs in order to improve health outcomes and mitigate the potential harm of public health measures to NCDs control. The study was guided by the following questions: What is the impact of the COVID-19 pandemic on the management of chronic diseases in South Africa?
3. DEFINITION OF CONCEPTS
3.1. Chronic Disease(s)
Chronic disease, according to [1, 12], is defined as a disease that lasts a long time and progresses slowly, such as non-communicable diseases (NCDs); instances include patients with a communicable disease (CD), such as HIV patients on antiretroviral therapy (ART). HIV has shifted from a devastating epidemic to a manageable chronic disease through the use of life-long ART. Generally, chronic diseases cannot be prevented by vaccines or cured by medication. In this study, NCDs refer to the four burdens of disease in South Africa, which include hypertension, diabetes mellitus, cardiac disease, and people living with HIV on ART (operational).
3.2. Coronavirus Disease
Refers to a newly discovered viral strain of infectious disease caused by the severe acute respiratory syndrome-associated coronavirus (SARS-Cov-2) virus, which was not previously identified in humans. While most people will experience mild, common cold to more severe symptoms, mild cases can recover without treatment, while moderate to severe cases may become seriously ill and require special treatment and hospitalization; especially in people with chronic diseases regarded as comorbidities (operational definition).
3.3. Pandemic
refers to an outbreak of a disease throughout a whole country or the world; in this study, the term refers to the coronavirus disease (operational definition).
3.4. Contribution of the Study to the Management of Chronic Disease
The study intends to present a broader perspective on the impact of the COVID-19 pandemic in the management of chronic diseases during a medical emergency to inform policymakers of the gaps and recommend strategies to address them in the future; thus, the findings of this study may ultimately reduce the burden of disease on the healthcare system, community, and the global economy.
4. MATERIALS AND METHODS
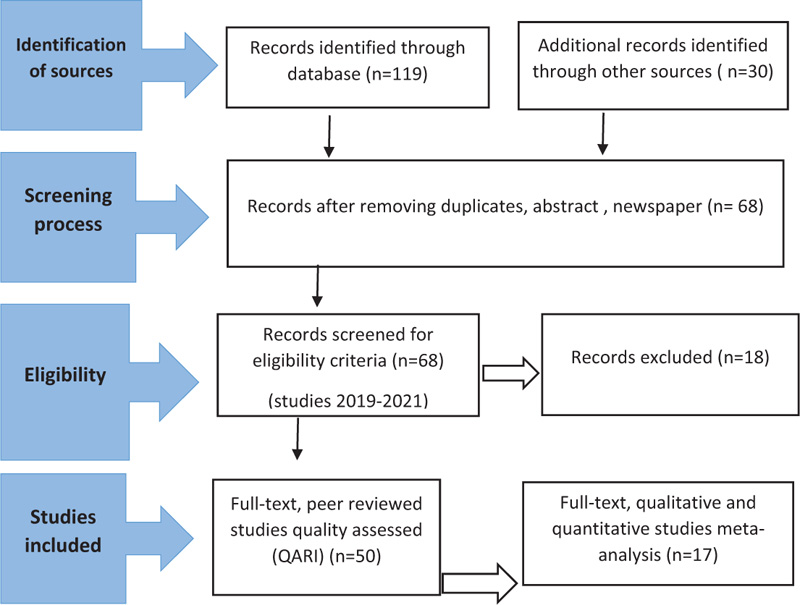
The review was conducted following the preferred reporting items for systematic review and meta-analysis (PRISMA) and a quality assessment and review instrument to synthesize qualitative and quantitative studies to identify key findings and answer the review question [13], (Fig. 1 and Table 1).
4.1. Information Sources and Search
A manual search of information was conducted with the assistance of an experienced librarian, using the following search keys or terms: COVID-19 and chronic disease or COVID-19 and experience of people with chronic diseases; COVID-19 and access to health services by people with chronic diseases from December 2019 to August 2021. Different search sources and databases were used to access information, including CINAHL Plus (EBSCO), PubMed, Google Scholar, Medline, ProQuest, APA, PsychINFO, various academic journals, South African publications, electronic resources, and Academic Search Ultimate, as illustrated in Fig. (1). The search strategy was documented, saved, and stored online.
| Author and Year | Country | Purpose | Participants | Methodology (Data Collection and Analysis) | Key Findings |
QARI Score |
|---|---|---|---|---|---|---|
| Chadasama et al., 2020 | 47 countries Africa, America, Asia, Europe |
To evaluate the global impact of COVID-19 on routine care of chronic disease | 202 healthcare professionals | The quantitative online survey, consent online | Changes in routine care to virtual communication. Impacted conditions were DM, chronic obstructive pulmonary disease, and HPT due to a reduction in access to care. 80% of the HCP reported that the mental health of the patients worsened during COVID-19. There were issues with digital technologies and virtual health care, appointments and telemedicine adapted to reduce face-to-face, self-management apps, and lack of technology in LMICs. | 8 |
| Grimsud, A. and Wilkison, L., 2021 | South Africa | To evaluate differentiated services delivery for HIV treatment during COVID-19 in sub-Saharan Africa | Lesson learned | Lesson learned | Expanding legibility criteria for differentiated service delivery (DSD) of HIV treatment to include children, adolescents, pregnant and breastfeeding women, those stable on the second-and third-line regimen, extending multi-month dispensing (MMD), reducing the frequency of clinical consultation, emphasizing community-based models or distribution out of the facility, integrating and aligning with TB-preventative therapy, NCDs and family planning. | 6 |
| McKinney, E.L., McKinney, V. and Swartz, L., 2020 | South Africa | Explore challenges that people with disability currently experience during COVID-19 in South Africa (and LMICs) concerning access to healthcare facilities | People with disability from chronic disease | Commentary | Marginalized and excluded, unable to access health care, receive therapeutic interventions or rehabilitation or medication. Those who access experienced discrimination regarding accessing life-saving treatment, ICU, and ventilator support, are at a higher risk of contracting COVID-19, due to factors that include the need for interpersonal caregivers and living in residential facilities. | 6 |
| Siedner, M.J., Kremer, J.D., Meyer, M.J. et al., 2021 | South Africa | To evaluate whether the implementation of lockdown orders in South Africa affected ambulatory clinic visitation in rural KZN | 46 523 individuals, 89 476 clinic visits during the observation | Observational cohort, 11 PHC clinics, interrupted time series analysis from pre-lockdown to level 5, 4, and 3 period | Reduction in clinic visits especially to stringent level 5, HIV from 37.5 to 45.6, the resilience of adults to access care, focusing on child health, perinatal, family planning, HIV, NCDs. | 7 |
| Ng, W.H., Tipih, T., Makoah, N.A., Goedhals, D. et al., 2021 | South Africa | To evaluate the correlation between comorbidities and their role in exacerbating diseases in COVID-19 and meta-analysis | 53 articles of which eight were eligible for meta-analysis | Systematic literature review, meta-analysis | HPT, obesity, and DM were identified to be the most prevalent comorbidities in COVID-19, independently associated with mortality in COVID-19 patients, chronic kidney leading stats to death. | 7 |
| Haque, O.S., Stein, MA, 2020 | South Africa | Perspective on clinical-based experiences of patients with disabilities during COVID-19 pandemic. | People with disability from chronic disease | Lesson learned | Stigma affecting equal access to health care requires implementation of human rights to prevent biases, rights of persons with disability, and COVID-19 patients with paraplegia. | 6 |
| McKinney, E.L., McKinney, V., Swartz, L., 2020 | South Africa | Notes in time of the pandemic | People with disability from chronic disease | Notes in time of the pandemic | During scarce resources and care, health care was faced with making decisions and prioritizing patients receiving life-saving resources over others, a triage policy was developed, and excluded or disadvantaged disabled people, and those with physical and intellectual impairment from gaining ICU access, and receiving ventilators, against the South African Constitution, where people are regarded as equal, have the right to life, dignity, right to access health care, as well as protection of dignity, rights of people with disability as per United Nations Convention, the debate was raised on whose lives are worth saving over others. | 6 |
| Nyoni, T. and Okumu, M., 2020 | South Africa | Description of ways in which COVID-19 public health responses are stressful to PLHIV and disruption of access and adherence to ART | Lesson learned during the COVID-19 pandemic on HIV treatment adherence interventions | Program review | In measures to prevent PLHIV from accessing needed ART, policymakers drew on resources and strategies to curb COVID-19. The government should develop strategies that minimize disruptions in access to treatment regimens for PLHIV. | 8 |
| Mash, R.J., Presence-Vollenhoven, M., Adeniji, A., et al., 2021 | South Africa | To describe the characteristics, clinical management, and outcomes of patients with COVID-19 at the district hospital | All patients presented to the hospital with COVID-19 between March and June 2020 | Descriptive observational cross-sectional study, primary and secondary data | Most patients had a high level of comorbidity – 67% were patients with comorbidity, HPT, DM, overweight, HIV, TB, chronic obstructive pulmonary disease (COPD), and needed oxygen and ventilators. | 8 |
| Nyashanu, M., Chinese, R., Mashawa, F. and Ekpenyong, M.S., 2021 | South Africa/ Zimbabwe | Explore the challenges of women taking ART during COVID-19 pandemic lockdown in a peri-urban areas | Women accessing ART | Explorative qualitative, semi-structured interviews, thematic analysis | Transport problems, confusing COVID-19 restrictions, abuse by police and soldiers at roadblocks, shortage of medication, lack of health check-up routines, involuntary default of ART, and shortage of PPE. | 8 |
| Ahmed, S, Ajisola, M., Azeem, K. et al., 2020 | Kenya, Nigeria, and Pakistan | Explore access to health care before and during COVID-19 with those working and living in slum communities | Seven slums, 860 community leaders, residents, health workers, and local authority representatives to explore stakeholders’ perspectives and experiences to access health care | Qualitative, semi-structured interviews, thematic analysis, March 2018 to May 2020 | They describe various preventive, diagnostic, and treatment services, antenatal care (ANC) and immunization, HPT screening, TB, HIV, and vector bone disease, that were not available due to the COVID-19 pandemic. GBV and mental health services were perceived to be limited or unavailable. It was reported that COVID-19 led to reduced access to healthcare services, cost increased, household income decreased, residents had difficulty reaching healthcare services, fear of being diagnosed with COVID-19 discouraged health seeking, health care was provided by phone, pharmacists and vendors extended credit, residents received philanthropic or government support, which was inconsistent and inadequate. | 8 |
| Mash, R., Goliath, C., and Perez, G., 2020 | South Africa | Commentary | Health facilities | Commentary | Two goals guided the re-organization – the need to prepare for the influx of people with COVID-19, the need to maintain social distancing and reduce risk to people using the services, facilities were re-organized to have screening and streaming at the entrance, patients were separated into hot or red, and cold or green/yellow streams. Both streams were seen and treated for minor ailments, patients with stable chronic diseases were provided with home delivery of medications by community health workers (CHWs), and CHWs engaged in community-based screening and testing. The challanges of primary health care (PHC) were poor infrastructure and difficulty to keep streams separate, and managers frequently had to address the fears and anxiety of healthcare workers. Attention was needed to prevent non-COVID-19 conditions, as utilization of services had ceased, exposing intra- and intersectoral fault lines, especially accessing social services. Community screening had to be refocused due to limited laboratory capacity and long turnaround times. | 7 |
| Nshimyiryo, A., Barnhart, D., Cubaka, V.K., Dsengimana, J.M.V. et al., 2021 | Rural Rwanda | Explore and describe barriers and coping mechanisms to accessing health care by people with chronic diseases during the COVID-19 lockdown | Chronic care patients, HIV, mental health, oncology | Cross-sectional study, active patients with an appointment scheduled from March to June 2020, and phone numbers recorded in the electronic medical record were eligible, telephone interviews, Fisher’s exact test was used to measure association, logistic regression analysis for associated factors | A large number of chronic disease patients experienced barriers to accessing health care during COVID-19. Large-scale physical distancing and movement restrictions imposed to contain COVID-19, often referred to as lockdown, abruptly and ubiquitously restricted access to routine health care. The study reported lack of access to emergency care medication, skipping appointments, oncology severely affected, and far distances from the facility with no transport, walking long distances, contacting clinicians via telephone for guidance and rescheduling appointments, and delegating someone else to collect medication. | 8 |
| Anjorin, A.A., Abioye, A.L., Asowata, O.E., Soipe, A., Kazeem, M.I, et al., 2020 | Nigeria | Exploration of the impact of differences in the epidemiology of key comorbidities in Africa | Notes in time of pandemic comparing HIV/TB epidemic to malaria pandemic | Document review and experiences | There is a great need to generate empirical data in Africa on clinical profiles and the predictors of morbidity and mortality from COVID-19. Improved health protocols for acute febrile illness and access to diagnostic facilities not just for COVID-19 but other infections as chronic diseases have a significant effect on COVID-19 prognosis. It requires the adjustment of the fragility of care delivery systems to clinical procedures and re-organizing care delivery; the one-size-fits-all response is not optimal. The lessons learned should be used to improve policy and the COVID-19 response framework. The disruption of HIV/TB, DM due to the COVID-19 pandemic can constrain HIV/TB control efforts and result in coinfection on clinical prognosis. | 8 |
| Ogeng, O.J., Karau, P.B., Misiani, M., Cheruiyot, L. et al., 2020 | Kenya | To describe possible long-term effects on the burden of atherosclerotic disease among Kenyans | 6 190 cases, patients with chronic disease | Document review | Common risk factors in Kenya, for COVID-19, include HPT, DM, obesity, cigarette smoking, respiratory tract infections, pulmonary embolism, and COPD. | 7 |
| Adams, S., Mulubwa, M., Van Huyssteen, M. et al., 2021 | South Africa | To investigate chronic patients' preferences for the last kilometer delivery service model | 116 patients | Exploratory quantitative study at four public PHC facilities in Cape Town, structured questionnaire, chi-square, and SPSS | Most chronic patients were interested in medicine delivery service, a mobile application for ordering treatment, preferred home delivery, a few willing to pay, gender, employment and distance to facility, and average long waiting time at the clinic. | 8 |
| Amu, H. et al., 2021 | Ghana | Explore the practices and challenges associated with the management of chronic NCDs by patients and healthcare professionals | 82 patients, 30 healthcare professionals | Qualitative, face-to-face interviews, thematic analysis | Education, specific practice based on the type and stage, patient self-management practices, self-restrictions, exercise, use of equipment to monitor health status at home, heavy workload, poor utility supply, and financial incapacity of patients to afford the cost of managing conditions. | 8 |
4.2. Studies Selection Process
A systematic literature review was conducted on both qualitative and quantitative studies published in English in Africa, which includes sub-Saharan Africa and South Africa, from December 2019 to August 2021 to analyze and describe the impact of the COVID-19 pandemic on the management of chronic diseases, such as hypertension, diabetes mellitus, cardiac diseases, and PLHIV on antiretroviral therapy (ART). The following papers were excluded during the screening process: studies that included children and adolescents; abstracts, duplicates; newspaper articles; magazines, and studies as they are not subject to peer review to ensure quality. Refer to Fig. (1), which presents the flow chart of the systematic literature review.
4.3. Data Extraction and Quality Assessment
Out of 119 abstracts reviewed, 17 (n=17) full-text studies were extracted and considered for the systematic review and quality assessment. These studies were critically evaluated using a quality assessment research instrument (QARI) designed by the Joanna Briggs Institute (JBI) in 2014. This instrument is used to assess and analyze both qualitative and quantitative studies (as can be seen in Table 1. Data were extracted and captured in Microsoft Excel, after which they were sorted and arranged alphabetically according to the first author's name, and then all duplicates were removed. Studies that scored 5 or fewer points were also excluded from the review to ensure quality.
4.4. Data Synthesis
Thematic data analysis was conducted to synthesize the full-text studies that complied with the quality assessment criteria of 5 or more. Data were coded, categorized to develop themes [17]. An experienced researcher was used to check the synthesis process and to ensure quality and compliance with the inclusion criteria.
5. STUDY RESULTS
A total of 17 studies were reviewed and analyzed. The majority of these included South African (52.9%) and other African countries' studies conducted in collaboration with western countries. Most studies were researchers’ commentaries, notes, lessons learned, and perspectives during the COVID-19 pandemic (52,9%) while a few empirical studies were conducted on patients (64,7%) and healthcare providers (17,6%); this may impose a risk of bias and quality as it is based on researchers’ personal opinions or perspectives. The types of chronic diseases included hypertension, diabetes mellitus, PLHIV on ART, cardiovascular disease, and stroke. Studies were conducted using quantitative and qualitative designs. The majority of studies were published in 2020 and 2021, and participants were mainly people with chronic diseases and healthcare providers. Three themes were identified, which are listed as follows: the impact of the COVID-19 pandemic on healthcare services; the impact of the COVID-19 pandemic on the management of people with chronic diseases; and the digitalization of healthcare services as illustrated in Table 2 below:
| Theme | Category | Subcategory |
| 1. COVID-19 impact on chronic healthcare service management | 1.1. Poor access to healthcare services | 1.1.1. Triage criteria to access specialized care |
| 1.1.2. Unavailability of transport services | ||
| 1.1.3. Frequent and abrupt closure of healthcare facilities | ||
| 1.1.4 Long waiting times | ||
| 1.1.5. Interrupted community-based services | ||
| 1.1.6. Postponement of healthcare services | ||
| 1.1.7. High rate of missed appointments | ||
| 1.1.8. Shortage of staff | ||
| 1.2. Inadequate/lack of resources | 1.2.1. Impact on patient care | |
| 1.2.2. Poor infrastructure | ||
| 1.2.3. Inadequate or interrupted supply of medications and other supplies | ||
| 1.3 Inadequate/poor implementation of the chronic care model | 1.3.1 Re-organization of health facilities into triage streams | |
| 1.3.2. Changes in eligibility criteria for decanting | ||
| 1.3.3. Inadequate screening, early detection, diagnosis and ongoing monitoring of chronic diseases | ||
| 1.3.4. Support groups and adherence counseling clubs suspended | ||
| 1.3.5. Financial inadequacy | ||
| 1.3.6. Reduced frequency of clinical consultation | ||
| 1.4. Psychological effect of the COVID19 pandemic on healthcare providers managing chronic diseases | 1.4.1. Fear of contracting COVID-19 infection | |
| 1.4.2. Stress, anxiety and depression | ||
| 1.4.3. Overwork and exhaustion | ||
| 2. COVID-19 pandemic impact on people with chronic disease | 2.1. Poor self-care management | 2.1.1. Inactivity |
| 2.1.2. Inability to use self-care instruments | ||
| 2.1.3. Diet | ||
| 2.1.4. Poor access to Internet in rural areas | ||
| 2.2. Psychological impact | 2.2.1. Fear of contracting COVID-19 and comorbidity | |
| 2.2.2. Stress, anxiety and depression | ||
| 2.2.3. Isolation from family members | ||
| 3. Digitalization of health- care services | 3.1. Transition to digital care without support | 3.1.1. Use of telemedicine in consultation |
| 3.1.2. Use of technological applications to access information about self-care management |
6. THEME 1: COVID-19 IMPACT ON CHRONIC HEALTHCARE SERVICES MANAGEMENT
6.1. Category 1.1: Poor Acess to Healthcare Services
6.1.1. Triage Criteria to Access Specialized Care
The literature revealed that patients with disabilities caused by chronic diseases such as stroke were discriminated against concerning access and use of scarce specialized care such as intensive care or ventilators, during the COVID-19 pandemic. Even though the health institutions tried to align it with South African and ethical international standards, this was against the Constitution, as well as the United Nations Convention on The Rights of People with Disabilities that all people have the right to life and access to health services [15, 16].
6.1.2. Unavailability of Transport Services
Restrictions of transport services during lockdown limited traveling to access chronic healthcare services such as clinical consultation, education on self-care management, collection of medications, and monitoring of conditions. The majority of patients with chronic diseases missed appointments to health institutions to collect their medication and for further management and care [9, 17].
6.1.3. Frequent and Abrupt Closure of Healthcare Facilities
Healthcare facilities, private or public, were frequently and abruptly closed due to COVID-19 cases and left chronic patients unattended and without medication [18, 19].
6.1.4. Long Waiting Times
Chronic disease patients had to wait for long hours for care due to changes in facility streams and the shortage of healthcare providers. The focus was mostly on screening and testing for COVID-19 [19, 20].
6.1.5. Interrupted Community-Based Services
Community-based services that normally provide screening, education, support, and management of chronic diseases were disrupted and focused on screening and testing of COVID-19 [7, 9, 21].
6.1.6. Postponement of other Healthcare Services
A chronic patient who suffered a stroke and required rehabilitation services were not attended to and this is key to a healthy recovery; the focus was only on prevention and control of COVID-19 [16, 22].
6.2. Category 1.2: Inadequate/lack of Resources
6.2.1. Impact on Patient Care
Literature indicated that healthcare providers reported high levels of lack of personal protective equipment (PPE) that exposed them to infection. Those who had access to PPE reported that it was of poor quality and that they feared contracting the virus. This had a negative impact on the care of patients with chronic diseases as well because healthcare providers without PPE contracted COVID-19 and had to stay in quarantine; for a while, the healthcare institution remained short-staffed. The limited number of healthcare providers on duty were prioritized to focus on COVID-19 management while neglecting other services, including care to patients with chronic diseases [9].
6.2.2. Poor Infrastructure
Some health facilities are poorly structured, not maintained, not well ventilated, and so small that it became difficult for healthcare providers to conduct triage, trying to separate patients with COVID-19 symptoms and those without, including implementing infection control measures such as practicing social or physical distancing. Hence patients receiving immediate care were those with COVID-19 and the rest were neglected [9].
6.2.3. Inadequate or Interrupted Supply of Medications and other Supplies
People with chronic disease experienced a lack or shortage of medication and they had to go buy or come back again for the medication interfering with adherence to and compliance with medication. Due to poverty in LIMCs, very few patients could manage to return to the institution for medication collection, hence affecting patients' adherence and leading to more health complications such as stroke and other challenges [13, 17, 21].
6.3. Category 1.3: Inadequate/Poor Implementation of the Chronic Care Model
6.3.1. Re-organization of Health Facilities into Triage Streams
South African health facilities were reorganized during the COVID-19 pandemic into a color-coded triage instead of a stream. Different colors used for patient classification included red representing severe illness, which means this patient requires immediate urgent resuscitation and emergency management. Orange requires very urgent management, yellow urgent management, and lastly green which means this patient may have to wait longer if patients red and orange are attended to. This confused and contributed to longer waiting times for people with chronic diseases who may not be classified in the top three classifications which are red, orange, and yellow [7, 9].
6.3.2. Changes in Eligibility Criteria for Decanting
Because of limited access to chronic healthcare services and the fear of contracting the virus, the criteria of repeat prescription collection strategies for chronic disease patients who are stable and adherent to treatment should be changed. These include those who do not need to be seen by a healthcare provider for review and other patients who normally require continuous consultation and management such as pregnant and breast-feeding women and adolescents living with HIV, PLHIV on second-line and third-line regimens and those with NCDs who require a six-month treatment instead of a 12-month treatment and are stable on treatment [8, 23].
6.3.3. Inadequate Screening, Early Detection, Diagnosis, and Ongoing Monitoring of Chronic Diseases
Routine screening of NCD and those eligible for HIV counseling and testing was suspended during the COVID-19 pandemic lockdown and interrupted for early detection, diagnosis, and ongoing monitoring of the chronic disease. This disrupted the goal of investing in the prevention, control, and management of chronic diseases to reduce the burden of disease [7, 21, 22].
6.3.4. Support groups and adherence counseling clubs suspended
Well-established support groups and adherence clubs were disbanded to prevent cross-infection and to comply with the infection prevention and control policies of COVID-19 and chronic disease patients were denied access to education, support, and care. Some of the people with chronic diseases are illiterate and have difficulty reading and understanding written instructions related to self-care management and need the support of these groups [18, 23].
6.3.5. Financial Inadequacy
Some people with chronic diseases lost their jobs and those with small businesses closed during the lockdown and were not able to pay for their medication, transport, and a balanced diet. Hence these patients ended up abandoning their chronic medications and faced more health complications [13, 21].
6.4. Category 1.4: Psychological Effects on Healthcare Providers
6.4.1. Fear of Contracting the COVID-19 Infection
Healthcare providers managing people with chronic diseases worked under a cloud of uncertainty and feared contracting COVID-19 in their health facilities or on the transport they used to come to work [7].
6.4.2. Stress, Anxiety, and Depression
Healthcare providers managing people with chronic diseases suffered stress and anxiety due to limited knowledge about the virus and the effects related to comorbidity should their patients become infected. Some had to be quarantined or self-isolated after exposure to COVID-19 cases and suffered from depression [7, 21].
6.4.3. Overworked and Exhausted Healthcare Providers
Due to a long-existing shortage of staff in the healthcare system and some healthcare providers being in isolation, quarantine or hospitalized, the remaining staff were overworked and suffered exhaustion and burnout worsened by fear of contracting COVID-19 [13, 17, 21].
7. THEME 2: COVID-19 IMPACT ON PATIENTS WITH CHRONIC DISEASE
7.1. Category 2.1: Poor self-care management
Studies revealed disruption in self-care management practices by people with chronic diseases that affected patients’ health outcomes [13, 24].
7.1.1. Inactivity
The study revealed strict lockdown regulations, which did not allow people to move around. The restriction of movement and being indoors resulted in physical inactivity, which is not healthy for patients with chronic disease [13]
7.1.2. Inability to use Self-care Instruments
The limited movement of caregivers and visitors left people with a chronic disease without support regarding the use and maintenance of self-care instruments such as BP or blood glucose machines, as visitors or caregivers exposed them to possible infection [13].
7.1.3. Diet
The control over the number of visitors and fear of going out shopping affected people with chronic disease dietary plans. They also lacked support in the preparation of their meals [13].
7.1.4. Poor Access to the Internet in Rural Areas
People with a chronic disease living in rural areas lack access to the Internet due to poor ICT infrastructure and are denied access to information regarding self-care over the Internet or access to telemedicine [9].
7.2. Category 2.2: Psychological Impact of the COVID-19 Pandemic on People with Chronic Disease
7.2.1. Fear of Contracting COVID-19 Infection and Comorbidities
Most people with chronic diseases missed appointments due to fear of contracting COVID-19 infections in health facilities or on public transport and complications related to comorbidities [5, 14, 25].
7.2.2. Stress and Anxiety
People with chronic diseases also suffered stress and anxiety due to fear, limited knowledge about the virus, and effects related to comorbidity, should they become infected, and some end up suffering from depression. Access to psycho-social services for mental health, such as gender-based violence, was limited [21, 24].
7.2.3. Isolation from Family Members
People with chronic diseases experienced isolation from family members and friends due to fear of cross-infection and comorbidities and suffered from boredom and depression [14].
8. THEME 3: DIGITALISATION OF HEALTHCARE SERVICES
8.1. Category 3.1: Transition to Digital care Without Support
The restriction of movement and fear of contracting COVID-19 infection resulted in the implementation of telemedicine, while people with chronic diseases lacked knowledge of technology and had inadequate support as visitors were restricted or controlled [9, 24].
8.2. The use of Technological Applications to Access Self-care Management Information
Some healthcare services use Internet apps, which has been a serious challenge to those who have never used it before; they were denied access to health and self-care management information as a result of this. Some people don't have cellphones or Internet access, therefore they can't use these apps. Due to the use of telephone consultations or WhatsApp for information and counselling on adherence, the healthcare system evolved away from routine clinical visits, and older people needed assistance to use such apps [13].
9. RECOMMENDATIONS
The WHO and the national Department of Health in South Africa and other African countries should develop an integrated NCD and infectious disease chronic care model and protocols for screening, diagnostic, prevention, and treatment using a community-based approach during medical emergencies to reduce mortality and comorbidity in the African region. This would also address inequalities in accessing health services, mitigate future effects, and enhance preparedness for future pandemics.
healthcare institutions should initiate and implement innovative ways of central dispensing, pre-packaging, and home delivery of medication during medical emergencies to reduce facility congestion, long waiting times, and improve access to treatment using local pharmacies, volunteers, non-governmental and community-based organizations, and community health workers via Uber, courier, bicycle, vehicles and electric scooters.
The use of telemedicine or digital technology during medical emergencies should be enhanced and adopted as new, normal interventions with support to cater to people with chronic diseases as an initiative to prevent comorbidities.
Mental health services should be optimized to provide support, counseling, and assist patients and HCPs to develop positive coping skills or mechanisms; and ensure the continuity of care, including social services to deal with gender-based violence and loss of jobs.
10. DISCUSSION OF STUDY FINDINGS
The sudden emergence of COVID-19 with little or non-preparedness of the healthcare system has harmed the management of NCDs. Chronic diseases are high in LMICs, which include South Africa and Africa as a whole, and contribute to 60% of deaths annually [1].
The literature reveals that access to chronic healthcare services has been severely interrupted by the COVID-19 pandemic and lockdown regulations intended to prevent and control the spread of infection. This has led to changes in facility triage criteria to receive specialized care, reorganization of facility streams, frequent and abrupt closure of health facilities, transport services and movement, disruption of routine chronic disease management, disturbance of community-based services, and long waiting times. The following studies [3, 18, 26-28], argue that there is clinical bias and discrimination when conducting triage in persons with a disability. Other studies claim that patients who needed healthcare services were denied access to specialty care such as rehabilitation and COVID-19-related care, intensive care, and ventilators. This is relevant to what the literature revealed that services for people with chronic diseases such as stroke were interrupted and not given priority [29].
This is against human rights and the United Nations Convention on the Rights of People Living with Disabilities and worsening health inequalities and such barriers should be dealt with decisively. The prevention and treatment services of NCDs have been severely disrupted by the pandemic, especially in LMICs, and are of high concern as people living with NCDs are at higher risk of severe COVID-19-related illness and death [17, 30-33]. In addition, reduced access to healthcare services and the disruption of chronic disease management during the COVID-19 pandemic increased the burden of NCDs on the healthcare system, community, and economy of the country, especially in LMICs. A study conducted in Nigeria by [34], confirms the need to reinforce and scale up interventions proactively rather than reactively. Therefore, the prevention and management of chronic diseases may reduce health expenditure in many African countries [35].
The South African healthcare system is already experiencing the challenges of poor infrastructure, shortage of staff, and medical resources, which were made worse by the current pandemic and were confirmed by studies conducted by [2, 3, 27, 28]. The reduced frequency of clinical consultation, changes in eligibility criteria for stable patients on treatment, and self-care management by people with chronic diseases due to COVID-19 have affected the investment and progress made so far concerning the reduction of the burden of disease [3]. Studies conducted by [18, 19] indicate that a reduction in clinical visits was observed during the stringent lockdown levels 5 to 4, while [11, 13] maintain that the eligibility criteria for a repeat prescription of chronic patients stable and adherent to treatment was expanded to children, adolescents, and pregnant and breast-feeding women with chronic disease and living with HIV and ART [16]. state that COVID-19 has had a negative impact on the diet, lifestyle, exercise, income, access to health care, anxiety, and stress levels of people with chronic diseases. Therefore, the psychological or mental health impact of the COVID-19 pandemic on both people with chronic diseases and their related healthcare providers has affected the safety and quality of care. This was supported by a study conducted in China by [7, 36-39], on the psychological impact of the COVID-19 pandemic, which revealed anxiety, stress, depression, insomnia, and somatic illness among healthcare providers and patients.
The transition to digital care without prior knowledge, support, and poor access to the Internet or ICT infrastructure limits self-care management and information and needs serious attention to achieve the intended outcomes of good adherence to and compliance with treatment [8, 10], found that COVID-19 brought changes in routine care to virtual communication and people with chronic diseases as they have to adapt and adjust to digital technology and telemedicine that is not available in LMICs.
10.1. Implications of the Study
The study findings may contribute to the adaptation and adjustment of healthcare policies and protocols in the management of chronic and infectious disease protocols. This may help to ensure the integration of services as they are both public health conditions of concern. It may also contribute to the nursing body of knowledge by providing insight into the impact of medical emergencies on the management of chronic disease.
10.2. Limitations of the Study
The study only focused on full-text, peer-reviewed studies conducted in Africa and South Africa; other international sources were excluded as they did not comply with the inclusion criteria. As studies conducted in South Africa are the researchers’ commentaries, perspectives, and notes made during the COVID-19 pandemic, so more primary studies are required to close the gap.
CONCLUSION
The purpose of the study was to analyze full-text studies to obtain a broader view of the impact of the COVID-19 pandemic on the management of chronic diseases. The literature revealed that COVID-19 significantly harmed NCDs hence affecting the healthcare system, people with chronic diseases, and healthcare providers. The study was limited to an African and South African context and further studies can be conducted to assess its global impact. COVID-19 and chronic diseases are both international public health concerns and call for equal attention.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus disease |
| NCD | = Non-communicable disease |
| HIV | = Human immunodeficiency virus |
| HCPs | = Healthcare providers |
| PLHIV | = People living with HIV |
| ART | = Antiretroviral therapy |
| DM | = Diabetes mellitus |
| HPT | = Hypertension |
| LMICs | = Low- and middle-income countries |
AUTHORS’ CONTRIBUTIONS
S.H. Mboweni and P.R. Risenga conceptualized, designed, conducted data collection through literature search, independently analyzed and wrote the manuscript, and edited and approved the manuscript for the final submission to the journal.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA Guidelines were followed.
FUNDING
None.
CONFLICT OF INTEREST
No financial or personal relationship influenced the writing of this article.
ACKNOWLEDGEMENTS
Special thanks to the librarian for support, guidance, and assistance in the literature search.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


