All published articles of this journal are available on ScienceDirect.
The Assessment of Community Knowledge and Prevention Practices of Malaria in a Rural Community in South Africa
Abstract
Background:
Malaria is a serious public health problem in sub-Saharan Africa and affects the health and wealth of nations and of individuals. Malaria became a public health issue killing more than 627 000 people in sub-Saharan Africa. In South Africa, Malaria is endemic in 3 provinces namely: Limpopo, Mpumalanga, and Kwazulu Natal. Limpopo contributes more cases than the other provinces in the country.
Objective:
The study assessed the knowledge and preventive practices regarding malaria in a rural community in South Africa.
Methodology:
A quantitative cross-sectional study was conducted using systematic probability sampling to select 151 household members. All the households in each village were visited and the head of each household was interviewed. Data was collected through close-ended questionnaires and analysed through the Statistical Package for Social Science version 24. The analysed data is presented in tables, graphs, and percentages.
Results:
The findings revealed that most participants 103(67.8%) have secondary education, and all (100%) had heard about malaria. The main source of malaria information was nurses 48%. Most participants knew that malaria is transmitted through mosquito bites (86%) by an infected mosquito (77%.%). About 63% of the participants knew the basic signs of malaria such as headache, shivering, and high fever. About 59 (39%) said they used mosquito coils and wore long-sleeved clothes in their household to avoid mosquito bites.
Conclusion:
Malaria poses a threat to the lives of people living in malaria-endemic areas. Community members of Masisi Village know how malaria is transmitted, what causes it, and its signs and symptoms. However, malaria prevention practice is still cited as a public health challenge. Therefore, health education should emphasize methods of malaria prevention and control.
1. INTRODUCTION
Malaria remains a major cause of morbidity and mortality worldwide and a global public health issue especially in sub-Saharan Africa(SSA) [1, 2]. An estimated 228 million malaria cases occur globally, and 15 countries carry about 80% of the global malaria mortality [3]. However, nearly half of the global population still lives in malaria-endemic areas and 435 000 people die from malaria every year [4]. Significantly, the international health community has increased its spending on the prevention and treatment of malaria resulting in the lowering of malaria incidence and mortality over the past fifteen years [5].
Studies revealed that children who are under five years are the most affected by malaria, accounting for 67% of malaria mortality worldwide. Besides, malaria has an impact on health expenditure, lost workdays, and school absenteeism [6-8]. South Africa is also experiencing this public health challenge. Early diagnosis and treatment of malaria are crucial to reducing morbidity and mortality rates. Malaria-infected patients should be treated within 24 to 48hrs after the onset, to prevent further parasites transmission. Therefore, it is advisable for the population living in malaria-endemic areas to have access to reliable diagnostics and have effective treatment to control the disease [9, 10].
A survey in the United States of America revealed that most malaria cases are imported and that travelers had little knowledge about malaria. The study also revealed that the appropriate prevention measures were still inadequate [11]. In Evrotas, Greece, migrants had challenges in recognizing malaria symptoms and prevention methods. They believed that after recognizing malaria symptoms, they would seek medical attention within 24hrs [12].Studies conducted in sub-Saharan Africa have revealed that the growing knowledge and awareness of vector control tools may increase the acceptance of new malaria control interventions. And the repellent products such as mosquito coils, topical repellent creams and spatial repellent emanators have been proven to be effective in protecting from malaria disease [13]. Khairy [14] reports that most participants in Saudi Arabia had heard about malaria, and knew that it is a communicable disease that can be prevented and mentioned social media as their main source of information.
South Africa is one of the frontline malaria eradication countries in the Southern African Development Community (SADC) and plays an important role in assisting neighboring countries to eradicate malaria. About ten percent of the South African population lives at the risk of contracting malaria in the three malaria-endemic provinces, namely: Limpopo, Mpumalanga, and Kwazulu Natal [15]. Malaria outbreaks are seasonal and unstable, with the transmission limited to warm and rainy summer months from September to May [16].South Africa achieves its reduction strategies through numerous vector control interventions including Indoor Residual Spraying (IRS) which is the application of insecticides on the walls and ceilings of residential structures in malaria areas [17].
Assessment of community knowledge, attitude, and practices about malaria is important in its control. This also helps to determine the level of overlapping with the biomedical views as it plays a significant role in improving the suitability and success of programs intended for reducing malaria transmission. In addition, malaria is an exceptional disease since its roots lie very deep within human communities. Practices and beliefs associated with malaria are often linked with culture as they can influence the effectiveness of control methods. Scholars note that the practice of malaria prevention is associated with the level of knowledge and the beliefs of people [18, 19].The understanding of the possible causes, mode of transmission and the decision about the adoption of preventive and control measures vary from community to community and among individual households. A lot of misconceptions regarding malaria still exist. Therefore knowledge, attitude, and preventive practice associated with malaria are vital for the implementation of culturally appropriate and effective interventions. Malaria diseases cannot be controlled by the health sector alone. Multiple strategies must be followed with other health-related sectors to help in the control of malaria. Control measures include insecticide-treated nets (ITNs) and Long Lasting Insecticides Treated Nets (LLITNs). However, there are many challenges to ITNs distribution, acceptance, and proper utilization in the regions of the world which stand to benefit the most. This contributes to low knowledge of malaria transmission in many malaria-endemic communities due to low levels of education and poor socio-economic status in the rural community [19, 20]. Despite measures that have been put in place by governments, malaria still remains a public concern and a cause of mortality and morbidity, especially in pregnant women, nursing mothers, and children under five years in sub-Saharan Africa [19].
Most patients in Nigeria and Kenya indicated adequate knowledge about transmission and prevention of malaria but had poor knowledge regarding malaria practices such as not using a mosquito net and mosquito repellent [21-23]. Participants acknowledged that malaria is a deadly disease. Chukwurah et al. [24] also revealed that participants sought treatment at the hospital after recognizing symptoms. However, in Ethiopia, participants had poor knowledge regarding malaria transmission but had sufficient knowledge about malaria prevention methods such as the use of insecticides in treating malaria bed nets (ITNs) [25]. Studies from rural areas show that people understand the risk of malaria but have poor knowledge and bad practices regarding healthy behavior for not seeking malaria treatment early. However, Arroz notes that in Mozambique, people have little knowledge about malaria due to illiteracy and this has negative effects on controlling malaria [26] and accessing health care. Patients often resort to consulting traditional practitioners instead of getting medication from medical institutions.
In Limpopo Province, malaria incidents declined from 9 487 in 2000 to 4 215 in 2010. Despite this reduction, the province is still the largest contributor to malaria incidence among the three provinces where the disease is endemic [27]. The province has five malaria-endemic municipal districts, namely Capricorn, Greater Sekhukhune, Mopani, Vhembe,and Waterberg. The province significantly contributes to South Africa’s malaria burden, accounting for most cases in 2010-2014 [28].
Vhembe District contributed more than 60% of the national malaria burden among the five-provincial malaria-endemic districts and is in the control phase of the elimination process. Vhembe is the highest burdened district, followed by Mopani, with the remaining three districts mainly reporting imported cases [29]. Furthermore, the number of locally-acquired cases increased significantly in the Vhembe district over the study period from 2478 in 2010 to 4116 in 2014 and unclassified cases dropped to 1175 in 2010 and 118 in 2012 but thereafter increased significantly to 1058 in 2014 [29, 30]
Many factors contribute to malaria transmission in the Vhembe District such as high temperature, humidity and rainfall. Besides the climate factors, the transmission of malaria infection is also determined by the socioeconomic conditions and access to malaria prevention tools as well as healthcare services. There is little information about the malaria knowledge, attitudes, and preventive practices in the population. Therefore, this study assessed the knowledge, and preventive practices regarding malaria at Masisi, a rural community in Limpopo Province of South Africa.
2. METHODOLOGY
2.1. Study Design
A descriptive cross-sectional survey design using a structured questionnaire, including demographic characteristics, knowledge, and practices of people about malaria prevention was used among 152 households to assess community members of Masisi Village regarding their knowledge of malaria and prevention practices.
2.2. Study Setting
The study was conducted in Masisi village under Musina Local Municipality, which is one of the five (5) local municipalities in the Vhembe District. The village is serviced by one clinic which is Masisi Clinic. The area is mostly rural and dry and very hot in summer with a maximum temperature of 40 degrees Celsius.
2.3. Study Population
The study population comprised all households in Masisi Village with household heads being the respondents. Where household heads were not available, their spouse or another consenting member of the household answered the questionnaire.
2.4. Sample and Sampling Method
Masisi village is comprised of 260 households. Systematic sampling was used to select households to participate in the study from the Masisi Register in the office of the local council. The study involves both males and females between the ages of 18 years and 65 years. Only those who are permanent residents of Masisi were allowed to participate in the study. Based on the sampling frame of 260 households, a sample size of n=151 was calculated using Slovin ‘s formula [n=N/{1+Ne2}].
2.5. Procedure
The researcher visited Masisi Village and obtained the permission of the traditional leader and later informed the community about the study. The questionnaire was administered by the researcher to the participants. The participants were given a questionnaire to complete on their own. Participants who could not read and write were assisted to complete the questionnaire. Questions were read and answers were written as they were given by participants. The questionnaires were completed on-site to reduce non-responses in a case where the participant needed assistance and clarity from the researchers.
2.6. Data Collection Method
The study questionnaire was developed in English and translated into Tshivenda, the local language spoken in the study area. Questionnaires with close-ended questions were administered by the researcher and the research assistant. The questionnaire was divided into four sections namely: Section A: demographic information, Section B: malaria knowledge, and Section C: prevention practices related to malaria and cross-tabulation with regard to age, level of education, and the relationship regarding what to do when participants see malaria symptoms.
2.7. Validity and Reliability
To ensure validity, the instrument development was guided by the study objectives and reviewed literature. The instrument was also reviewed by experts in the field of public health before data was collected. Ten households were used during the pre-test to check if respondents would understand the questions in the research tool. The respondents’ comments helped the researcher to adjust the questionnaire and make corrections. These respondents did not form part of the main study. This was done in one day and comparisons were made based on the respondents’ responses. This type of reliability measures how participants respond to one set of questions. Cronbach’s alpha was used to analyze the report. A Cronbach of 0.85 was obtained indicating a strong relationship as it was closer to 1.
2.8. Data Analysis Method
The statistical analysis was carried out through the Statistical Package for Social Sciences (SPSS version 24.0) to analyse the data because the findings of the study were recorded in numbers. During data analysis, each questionnaire was coded and all sections were thoroughly checked. Missing data were checked with the data collection form and questionnaire. Data were presented through figures and tables.
3. RESULTS AND DISCUSSION
A total of 152 participants were surveyed from October-November 2018 (Table 1). Out of 151 participants, 60% were females and 40% were males. About 34% of the participants were between the ages of 25 and 34 years, while 3% were over 65 years. With respect to the educational level, the majority (68%) of the participants had attained schooling up to secondary level while 7% never went to school. The majority (73%) of participants were unemployed. Almost half (53%) of the participants lived in formal houses and 47% in informal houses (Mikhukhu). More than half (64%) of the participants have been staying in the study area for more than five years.
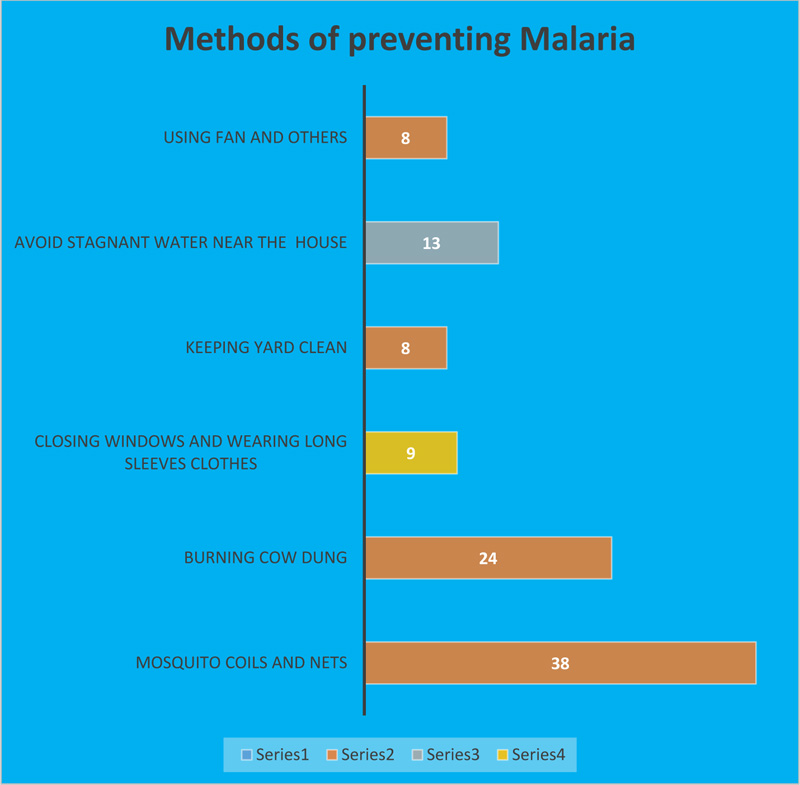
Table 2 shows the level of knowledge and preventive measures against malaria adopted by the study participants. Of the 151 participants, all (100%) had heard about malaria. The majority (73%) of the participants indicated that they had malaria at least once. More than half (56%) of them knew people who had died due to malaria. The main source of malaria information was nurses (48%) followed by the community health worker at 32%. The majority (86%) of participants knew that malaria is transmitted through mosquito bites by an infected mosquito (77%). And these bites occurred mostly during the night (65%). Ninety-five (63%) of the participants knew the basic signs of malaria. Furthermore, the majority (86%) knew that malaria should be treated within 24 hours of suspecting malaria symptoms and that an infected person should seek treatment at a hospital or clinic (67%). However, 33% mentioned that a malaria-infected person should be helped by traditional healers. Prevention of stagnant water, and wearing long-sleeve clothes were the most commonly mentioned preventive measures by 39% and 34% participants, respectively. In addition, participants (92%) specified that they would allow IRS spraying in their houses. Fig. (1) shows the methods of malaria prevention and practice. Fifty-eight (38%) participants said they used mosquito coils and 36 (24%) burned cow dung to prevent mosquito bites.
Table 3 indicates the relationship between participants’ age, level of education, and knowledge regarding where to seek medical attention after recognizing malaria symptoms. The study shows that there is an association between the age of participants and the type of malaria health-seeking behavior.The majority (71%)of the participants whose age was above fifty-six years preferred traditional healers as compared to those between 18-24years (72.2%)who preferred to go to the clinic.The study shows that there is no association between the level of education and utilization of a clinic when one is having malaria symptoms. Participants with no formal education(68%) stated that they preferred to go to the clinic if they recognized malaria symptoms (Table 3).
| Characters | Category | Frequency | Percentages |
| Gender | Female Males |
91 60 |
60.2% 39.7% |
| Age | 18-24 25-34 35-44 45-55 56 and above |
36 52 30 16 17 |
23.8% 34.4% 19.9% 10.6% 11,3% |
| Level of education | Never went to school Grade-1-7 Grade 8-12 Diploma/Degree |
25 24 92 10 |
16.5%% 15.9% 61,0% 6.6.% |
| Employment | Unemployment Employed |
110 41 |
72.8% 27.2% |
| Type of housing |
Formal housing
Informal housing/Shacks |
80
71 |
53.0%
47.0% |
| Duration of stay in the area |
Less than 5years
More than 5years |
53
98 |
35%
65% |
| Statement | Category | Frequency | Percentage |
| Have you ever heard about malaria | Yes No |
151 0 |
100% |
| Have you ever suffered from Malaria for the past 5years |
Yes
No |
110
41 |
73%
27% |
| Have ever heard of Malaria deaths: past 5years |
Yes
No |
85
66 |
56%
44% |
| Source of malaria information | Community health worker Nurses Media(TV & Radio) Family member/friends |
48 73 14 16 |
31.7% 48% 9.2% 10.5% |
| Causes of malaria | Rainfall Mosquito bite Temperature above 37 |
12 130 9 |
8% 86% 6% |
| How is malaria transmitted | By using contaminated water By eating rotten food Infected mosquito bite I don’t know |
19 5 117 10 |
13% 3% 77% 7% |
| Knows about the basic signs of malaria(High fever, shivering and headache) | Yes No |
95 56 |
63% 37% |
| When do malaria mosquito bites |
During the night hours
Anytime of the day |
98
53 |
65%
35% |
| When to seek medical attention after suspecting malaria | Within 24hours After 24hours |
129 22 |
86% 14% |
| Where to seek treatment after suspecting malaria | Clinic/hospital Traditional healers/self-treatment |
101 50 |
67% 33% |
| Main malaria preventive measures mentioned |
Sleeping under a mosquito net
Prevent water stagnation Covering of body with clothes Cleaning the house |
16
59 51 25 |
11%
39% 34% 16% |
| Allow Indoor residual spraying of the house by the government |
Yes
No |
139
12 |
92%
8% |
| Variable | Where to Seek Medical Attention | Total | |||||
| Private Doctor | Traditional Healer | Nearest Clinic | |||||
| Frequency | % | Frequency | % | Frequency | % | ||
| Age 18-24 25-34 35-44 45-55 56 and above |
7 | 19.4% | 3 | 8.3% | 26 | 72.2 | 36(23.8%) |
| 14 | 30% | 2 | 3.8% | 36 | 69.2 | 52(34.4%) | |
| 8 | 27% | 7 | 23.3% | 15 | 50,0 | 30(20%) | |
| 2 | 12% | 4 | 25.0% | 10 | 62.5 | 16(10.6) | |
| 3 | 17.6% | 10 | 70.5% | 4 | 23.5 | 17(11.2) | |
| Total | 34 | 26 | 91 | 100 | |||
| Level of education | |||||||
| Never went to school | 3 | 12% | 5 | 20% | 17 | 68% | 25(16.5) |
| Grade 1-7 | 5 | 20.8% | 8 | 33.3% | 11 | 45,8 | 24(15.) |
| Grade 8-12 | 25 | 27.2% | 8 | 8.7% | 59 | 64.1 | 92(61.0) |
| Diploma and degree | 5 | 50% | 1 | 10% | 4 | 40% | 10(6.6) |
| Total | 38 | 22 | 91 | 100 | |||
4. DISCUSSION
The study assessed participants’ knowledge and preventive practices about malaria. There were more females (60%) than males who participated in the survey. This is likely because most females are unemployed and do household chores. Similar study findings were reported by Sigh [30] in Nigeria and by Manana, Kuonza, Musekiwa, Mpangane, and Koekemoer [31] in Kwazulu Natal where there they were more female participants than males. Tshivhase and Mashau [32] also reported similar study results. However, the results obtained by Shimaponda in Zambia [33] indicated a high number of males than females. Literacy level is an important determinant of health status and is closely linked to poverty. Furthermore, poverty can affect malaria treatment-seeking and prevention behaviors [34].The level of education in this study setting was low because most participants had no formal education. This means that those who had no formal education did not view and understand things the same way as those who had secondary and tertiary education.
WHO states that literacy levels may affect one’s ability to recognize signs and symptoms of malaria and knowledge of the available treatment [30]. Our study concurs with Hlungwane’s findings [35] in South Africa who reported that a high number of participants who had secondary education quickly recognized malaria symptoms. However, Hanafi-Bojd, Vatandoost, Oshaghi., et al. [36] reported a high rate (44.2%) of illiteracy level in their southern Iran study. The number of participants who lived in formal housing was slightly higher (53%) than those who lived in informal housing, locally known as Mikhukhu. Most participants had been staying in the study area for more than five years and had weekly municipal waste removal. The type of housing played an important role in malaria prevention. Participants who live in formal houses and receive indoor residual spraying can prevent mosquito infestation for longer than those who live in shacks. Wanzirah, Tusting, Arinaitwe., et al. [37] and Ondiba, Oyieke, Ong’amo., et al. [38] observed that IRS remained longer in plastered walls than in shacks. Study findings revealed that most participants had adequate knowledge regarding the cause of malaria disease, transmission, and when to seek treatment. This might be because most participants have had malaria before and knew people who had died from the disease.These findings are similar to those by Munzhedzi, McQuade, Guler.,et al. [39] who reported that malaria is a dangerous disease if not treated early. The most common source of malaria information were nurses and community health workers. Similar findings were observed in other studies conducted elsewhere in South Africa, Ethiopia, Zambia, and Swaziland where most participants mentioned health organizations as the main source of malaria information [39-41]. Although most participants correctly indicated the bite of an infected mosquito as a malaria transmission route, eating rotten food and drinking contaminated water were mentioned by some participants. These participants likely confused malaria transmission with that of cholera. Similar findings were obtained in Vhembe District, Southern Africa where it was revealed that one in ten participants linked drinking bad water with malaria and 1 in 5 associated dirty surroundings with malaria [41, 42,]. Forero et al. [43] studied participants who said that malaria is transmitted through blood transfusion and had obtained this information from television and radio. Participants' knowledge of modern and traditional malaria treatment used in clinics and hospitals was insufficient. Almost half of the participants said they would seek treatment within 24 hours from a health facility after suspecting malaria infection. However, thirty-three percent of the participants indicated they preferred consulting a traditional healer before going to the clinic or hospital. This shows that traditional healers still play a major role in this study setting since villagers use them as their first contact before visiting health facilities. Similar studies were conducted by Yaya, Bishwajit, Ekholuenetaleet al [44]. and Musoke et al. [45] in Uganda and Zambia where participants went to health facilities within 24 hours upon noticing signs and symptoms of malaria. However, in Kenya, Ondari [46] found that participants preferred to self-medicate before going to the hospital. These patients said they knew effective traditional malaria medicine. They used cow dung, and herbs and ate goat offal and cypress leaves as malaria medication. Parallel results were also reported in Zimbabwe where participants used leaves, roots, bitter fruits, and salty water as malaria medication. Also, participants only visited the hospital after consulting traditional healers [47]. In the current study, participants said the removal of stagnant water was the main malaria preventive measure. Saha, Sarker, Kabir, Lu, and Muller [48] reported similar findings that preventing water from being stagnant and clearing vegetation were practiced regularly by their study participants. This shows that participants knew that stagnant water and thick vegetation habor mosquitos that can cause malaria. However, there was a poor use of bed nets in the current study and this is likely due to the unavailability of bednets. The South African government does not provide bednets to its citizen as part of the vector control intervention. Similar findings were reported by Munzhedzi et al. [39] in their South African study. By contrast Saha et al. [48], found that sleeping under a mosquito net was the most mentioned malaria preventive practice in their study.
The findings revealed that most participants had good understanding of the prevention of malaria at the household level. Mosquito coils (38%) were the main malaria prevention measure that participants reported. Twenty-four percent of the participants indicated the use of unproven preventive measures for malaria controls such as the burning of cow dung. They pointed out that cow dung reduces mosquitoes in the house. Some participants have said they make sure that there is no stagnant water near their homes to prevent mosquitoes from breeding. Similarly, other studies conducted in South Africa, Uganda, and Ethiopia found that participants knew about malaria prevention measures. These studies reported the use of long-sleeved clothing, removing stagnant water to prevent mosquito breeding, and the use of traditional methods such as burning cow dung among other methods [33, 45, 49]. Gupta, Aneja and Rana [50] and Aderaw and Gedefaw [51], also reported that their participants removed stagnant water and burned cow dung or used certain plants as measures to reduce mosquitoes in the house. Fullman, Burstein, Lim, Medlin and Gakidou [52] stated that most participants in Colombia control indoor malaria transmission by insecticides treated nets (ITN) for malaria protection, and a few participants used home sprays.
5. LIMITATIONS
The study was conducted in one municipality and therefore the results cannot be generalized to the whole Vhembe District. Further studies of malaria and its vectors are recommended. The other limitation of this study was that it sought to establish participants’ attitudes and this is a subjective process.
CONCLUSION AND RECOMMENDATIONS
The study demonstrated that participants have adequate knowledge about the strategies for preventing malaria. Participants mentioned high fever, shivering, and headache as the most common symptoms of malaria. Participants also knew how malaria is transmitted and its cause. What is worrisome, however, is that a significant percentage could not identify the major signs and symptoms of malaria. The findings also revealed that most participants used mosquito coils and mosquito sprays to prevent mosquito bites that could cause malaria. Yet, there is no decrease in the number of malaria cases reported. The community still has challenges when it comes to prevention practice at the household level. Thus, this study recommends an improvement in the implementation of the control program such as: the training of health workers and the dissemination of public information about the prevention of malaria disease and the reduction of misinformation. The strengthening of malaria education programs for local health authorities in this study setting to eradicate malaria is also recommended.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the University of Venda’s Research Ethics Committee (SHS18PH/12/1806).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent has been obtained from the participants involved.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that they have no competing interests
ACKNOWLEDGEMENTS
Declared none.


