All published articles of this journal are available on ScienceDirect.
The Relationship between Social Support and Hopelessness among Iranian Students during Coronavirus disease 2019 (COVID-19) Pandemic
Abstract
Background:
The coronavirus disease 2019 (COVID-19) pandemic has major consequences for public health worldwide, especially for mental health. Hope is a dynamic motivational system that empowers one to achieve goals. Social support similarly increases the feeling of well-being to cope with hopelessness. The present study was conducted to determine the relationship between social support and hopelessness in students studying at the Iran University of Medical Sciences during the COVID-19 pandemic considering the importance of performance in medical sciences students.
Methods:
This cross-sectional study was performed continuously for five months, from January to May 2021, at the Iran University of Medical Sciences, Tehran, Iran, where the Persian language is predominantly spoken. Participants were included if they could consent to participate in the study and internet access and membership in social networks. Those who did not fully engage with our data collection tools were excluded. A demographic information form, the Beck Hopelessness Scale (BHS), and the Multidimensional Scale of Perceived Social Support (MPSS) were provided to students via social networks. After students (n=300) completed the questionnaires, data were analyzed through SPSS software version 21.
Results:
The mean age of participants was 23.46 (18-51) years. The mean score of hopelessness among the participants was 6.2. The majority of students (35%) had mild hopelessness, 34.7% had a minimum level of hopelessness, 26.7% had a moderate level of hopelessness, and 11% had a high level of hopelessness. The mean social support score was 59.49, with 52.3% of students having a high level of social support. The correlation coefficient between social support and hopelessness was - 0.401 (p < 0.001). Field of study, degree level, marital status and lifestyle were significantly correlated with hopelessness. Also, only marital status had a significant relationship with social support among students. The results of multiple linear regression analysis showed that out of the variables included in the model, only the variable of social support had a significant effect on the hopelessness score, so this variable predicted 18% of the hopelessness score.
Conclusion:
Given the inverse relationship between social support and hopelessness, it is suggested to increase the level of social support for students to improve their sense of hopelessness.
1. INTRODUCTION
The 2019 Coronavirus (COVID-19) pandemic has created a global health burden that has had major implications for public health worldwide. COVID-19 is a pneumonia-like disease that emerged from the Coronavirus in November 2019 in Wuhan, the capital of Hubei Province, China [1]. Since the beginning of the COVID-19 outbreak, most governments have sought to slow the spread of infection through emergency measures, including public shutdowns, travel cuts, and house quarantine, which resulted in social isolation [2, 3]. Nevertheless, the current COVID-19 pandemic, much like the SARS pandemic of 2003 and other past pandemics, will have long-term impacts on people's mental health. Therefore, it is necessary to actively identify and study the influencing factors related to such pandemics in various contexts [4]. Indeed, many researchers have already studied the psychological impact of pandemics upon various communities and groups, indicating a severe and wide range of mental illnesses [5].
Hope is a dynamic, cognitive, and motivational system that empowers one to set goals, visualize the paths needed to achieve goals, and have the motivation to achieve their goals [6, 7]. The positive emotions which arise from hope increase life satisfaction along with facilitating problem-solving and decision-making, especially in critical situations [8]. Importantly, hope and mental health are related to each other [9-11] and thus may usefully be studied together to better both. Gafari et al. reported a significant inverse correlation between social support scores and total mental health scores among students of Tabriz University of Medical Sciences in Iran, whereby participants’ mental health scores decreased significantly with increasing social support [12]. Yet these academics also recommend conducting similar studies within contexts other than those rooted within Turkish cultures and languages in Iran.
Social support increases emotional well-being, which is one of the best ways to cope with loneliness and despair [13]. Such support has been strongly associated with mental health among various samples, including an aging population [14] and health care workers [15, 16]. However, Fangjun et al. found a weak relationship between social support and mental health in the elderly [17]. In another study, Fiori and Denckla claimed that social support only affects women's mental health and has no effect on men’s mental health [18]. Thus, it will be important to identify which groups' social support may be significant in COVID-19 recovery.
Student life is a stressful period because many expectations in the social and educational fields are placed on students by the family and university [19]. Nevertheless, due to the COVID-19-induced sudden closure of universities, rapid changes in learning and online education, and the significant prevalence of depression among students, such students may now be considered a vulnerable group in need of urgent assessment [20, 21]. The future course of COVID-19 is still unclear, and its reoccurrence is possible [22]. This uncertainty caused by COVID-19 affects all aspects of life, including mental health [23]. However, few studies have been conducted to measure the hopelessness of medical students in developing countries, and those which have been done have not focused on Persian cultures and language, which are most dominant amongst Iranian people. In light of the above, this study aimed to determine the relationship between hopelessness and social support in Persian-speaking students studying at the Iran University of Medical Sciences during the COVID-19 pandemic (Figs. 1 and 2).
2. MATERIALS AND METHODS
2.1. Study Design and Participants
We conducted a cross-sectional study. After receiving ethical approval and the ethics code: IR.IUMS.REC.1399.1049 from the University, sampling was performed continuously for five months from January to May 20201. Due to the lack of access to students, an online questionnaire was used, and its electronic links were sent to students on social networks (WhatsApp, Telegram and Email). The study population included all students studying at the Iran University of Medical Sciences, Tehran, Iran, in 2020, where the Persian language is predominantly spoken. Participants met the inclusion criteria if they were willing to consent to participate in the study and had internet access and membership in social networks. Participants were excluded if they only partially engaged with our data collection tools.
2.2. Study Sample
The following formula was used to determine the sample size:
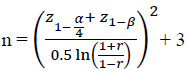 |
In this formula, α and β are the first and second type errors, respectively, considered as 0.05 and 0.10 in this study. R is the correlation between hopelessness and social support obtained from the study of Madani et al. and is equal to 0.27 [24]. According to the above equation, the minimum sample size of 146 students was calculated, but 300 students were selected to increase the study’s capacity and allow for dropout rates.
2.3. Outcome Measures and Measurements
Data collection tools included a demographic information form, the Beck Hopelessness Scale (BHS) (Supplementary file 1) and the Multidimensional Scale of Perceived Social Support (MPSS) (Supplementary file 2).
The Beck Hopelessness Scale (BHS) measures one’s negative expectations about future events. This scale had 20 questions with yes or no answers, with a score of 0 and 1, respectively. The questionnaire measures three dimensions of hopelessness, including feelings about the future, motivation or loss of motivation and expectations. This questionnaire is designed for people aged 17 to 80; the score obtained on this scale is between 0 and 20. A higher score indicates a higher level of hopelessness. Scores between 0-3 indicate mild hopelessness, scores between 4-8 indicate minimum hopelessness, scores between 9-14 indicate moderate hopelessness and scores of 15-20 indicate severe hopelessness. In the main version of the tool, reliability was reported to be 0.69 after one week and 0.66 after six weeks using the test-retest method [25]. Also, in Iran, the reliability of this tool was measured in a sample of students who had passed the MSc entry exam with Cronbach’s alpha of 0.87 for the whole questionnaire and between 0.83 and 0.86 for subscales [26].
The Multidimensional Scale of Perceived Social Support (MPSS) was used to measure social support. This tool has 12 questions that measure received support from family, friends, and significant others. The score range of this scale is between 12 and 84. A score of between 12-35 indicates a low level of perceived social support, scores between 36- 59 indicate a moderate level of perceived social support, and scores between 60 and 84 indicate a high level of perceived social support. The reliability of this tool has been reported to be between 0.72 and 0.85 using the test-retest method [27]. In the Persian version of this tool, Cronbach's alpha of 0.85 was obtained for the whole questionnaire and 0.91 for the subscales [28].
2.4. Analyses
After data collection, the data were statistically analyzed by SPSS software version 21. Descriptive statistics such as mean, standard deviation, frequency and percentage were used to make sense of the data. Kruskal-Wallis and Mann-Whitney tests were used to examine the relationship between hopelessness, social support and demographic variables. The Spearman correlation test investigated the relationship between hopelessness and social support. A multiple linear regression test was also used to investigate the relationship between hopelessness and other variables. A significance level of 0.05 was considered in all tests.
3. RESULTS
3.1. Participants
After distributing the questionnaires electronically, they were observed by 530 students, 312 of which completed questionnaires. After excluding incomplete questionnaires, data collected from the 300 participants (58%) who met the inclusion criteria were analyzed. The mean age of participants was 23.46 ± 5.35 years. Also, 37.3% of participants were male, and 62.7% were female. The majority of participants were studying medicine (n = 141; 47%) and were single (n = 266; 88.3%) and living with their parents (n = 249; 83%). Moreover, 106 students (35.33%) worked in hospitals and medical centers during the pandemic, of whom 27 (25.47%) directly worked inwards designated to COVID-19 patients. Demographic information of the studied samples is given in Tables 1-3.
| Variables | Frequency | Mean | SD† | δ P-value | |
|---|---|---|---|---|---|
| Age | 300(100) | 59.49 | 14.81 | *0.25 | |
| Gender | Male | 112(37.3) | 57.34 | 15.11 | **0.06 |
| Female | 188(62.7) | 60.77 | 14.51 | ||
| Field of study | Midwifery | 48 (16) | 60.79 | 14.52 | *0.35 |
| Rehabilitation | 29(9.7) | 59.89 | 13.09 | ||
| Science Basic | 15(5) | 53.13 | 18.94 | ||
| Medicine | 141(47) | 58.43 | 14.31 | ||
| Paramedical | 6(2) | 58.41 | 15.66 | ||
| Nursing | 49(16.3) | 61.38 | 16.9 | ||
| Management and information | 12(4) | 66.58 | 8.27 | ||
| Grade | Bachelor | 83(27.7) | 59.62 | 13.65 | *0.48 |
| Master of Science | 69(23) | 59.92 | 17.76 | ||
| General Medicine | 137(45.6) | 59 | 14.03 | ||
| PhD | 11(3.7) | 61.9 | 13.67 | ||
| Marital status | Single | 266(88.3) | 58.83 | 14.98 | **0.04 |
| Married | 34 (11.7) | 64.32 | 12.51 | ||
| Life style | Alone | 22(7.3) | 57.04 | 13.91 | *0.48 |
| With parents | 249(83) | 59.11 | 14 | ||
| With Spouse | 29(9.7) | 64.68 | 13.29 | ||
| Variables | Frequency | Mean | SD† | δ P-value | |
|---|---|---|---|---|---|
| Age | 300 (100) | 6.11 | 4.54 | *0.31 | |
| Gender | Male | 112 (37.2) | 6.33 | 4.41 | **0.36 |
| Female | 188 (62.7) | 5.98 | 4.63 | ||
| Field of study | Midwifery | 48 (16) | 5.37 | 5.12 | *0.05 |
| Rehabilitation | 29 (9.7) | 4.93 | 4.39 | ||
| Science Basic | 15 (5) | 6.86 | 4.34 | ||
| Medicine | 141 (47) | 6.8 | 4.24 | ||
| Paramedical | 6 (2) | 8.61 | 7.05 | ||
| Nursing | 49 (16.3) | 5.71 | 4.69 | ||
| Management and information | 12 (4) | 3.83 | 3.15 | ||
| Grade | Bachelor | 83 (27.7) | 5.63 | 4.85 | *0.04 |
| Master of Science | 69 (23) | 5.37 | 4.49 | ||
| General Medicine | 137 (45.6) | 6.75 | 4.26 | ||
| PhD | 11 (3.7) | 6.45 | 5.39 | ||
| Marital status | Single | 266 (88.3) | 6.31 | 4.56 | **0.01 |
| Married | 34 (11.7) | 4.32 | 3.87 | ||
| Life style | Alone | 22 (7.3) | 6.86 | 3.93 | *0.03 |
| With parents | 249 (83) | 6.27 | 4.62 | ||
| With Spouse | 29 (9.7) | 4.21 | 3.91 | ||
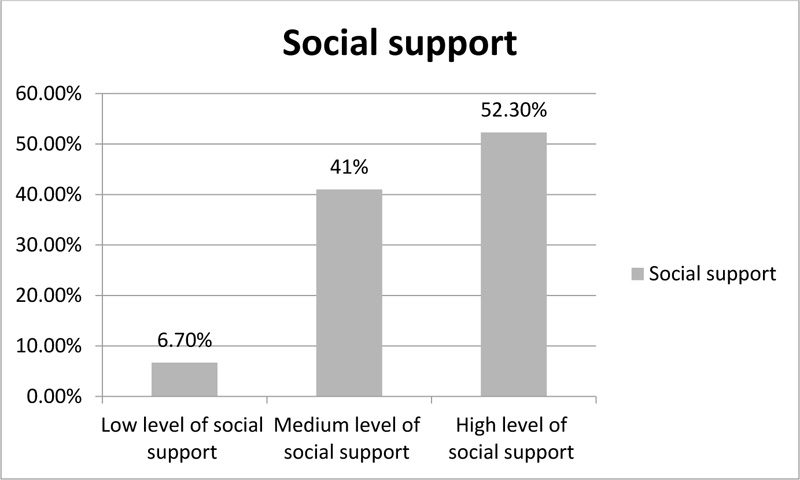
3.2. Social Support
The mean score of social support was 59.49 ± 14.81. The lowest score for social support was 14, and the highest was 84. Also, 52.3% of students had a high level of social support, 41% had a medium level, and 6.7% had a low level of social support (Table 2). Among the dimensions of social support, the mean and standard deviation of family support was 21.08 ± 5.58, others’ support was 19.11 ± 5.72, and friends’ support was 18.17 ± 6.2. There was no significant relationship between perceived social support and demographic variables of age, gender, lifestyle, the field of study, and working in a hospital during the COVID-19 pandemic. However, there was a statistically significant difference between social support and marital status (p = 0.04), as married students had higher levels of social support (64.32 ± 12.51) than single ones (58.83 ± 14.98).
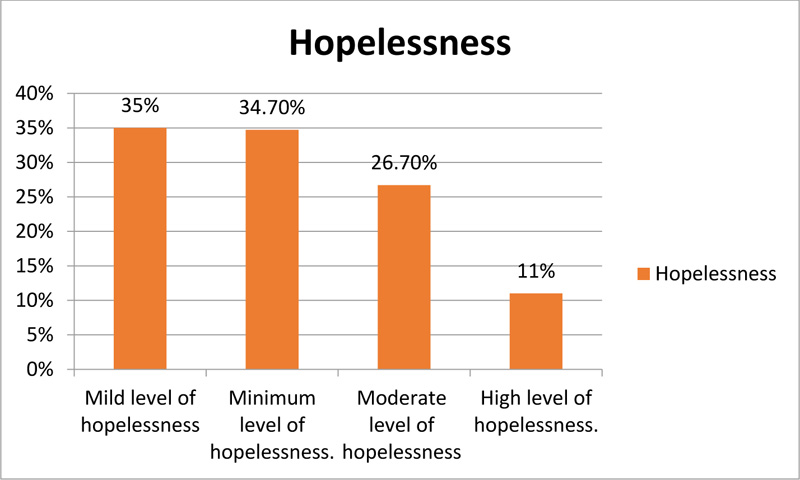
3.3. Hopelessness
The mean score of hopelessness was 6.11 ± 4.54. The lowest score of hopelessness was 0, and the highest was 20. Also, 35% of students had a mild level of hopelessness, 34.7% had a minimum level of hopelessness, 26.7% had a moderate level of hopelessness, and 11% had a high level of hopelessness. There was no significant relationship between hopelessness and demographic variables of age, gender, the field of study and working in a hospital during the COVID-19 pandemic. However, there was a statistically significant difference (p = 0.04) between hopelessness and degree level, as hopelessness seemingly increased with the increasing degree level. Single students (6.31 ± 4.56) had higher levels of hopelessness than married students (4.32 ± 3.87) (p = 0.01). Students who lived with their spouse (4.21 ± 3.91) also had lower levels of hopelessness than students who lived with their parents (6.27 ± 4.62) or alone (6.86 ± 3.93), and this difference was significant (p = 0.03), (Table 2).
3.4. Hopelessness Correlates
According to the Spearman correlation test results, there was a statistically significant relationship between social support and hopelessness (r = - 0.401, p <0.001). With increasing social support scores, the level of hopelessness decreased.
Variables with p < 0.05 were entered in the multiple linear regression model to estimate the effect of demographic variables and social support on hopelessness. The results of multiple linear regression showed that, among the variables included in the model, only the variable of social support significantly affected the hopelessness score. This variable predicted 18% of the hopelessness score (Table 4).
Table 3.
| Variables | Frequency | Hopelessness | Social support | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD† | P-value | Mean | SD | P-value | |||
| I have worked in hospitals and medical centers during the COVID-19 pandemic. | Yes | 106 | 6.82 | 4.68 | *0.07 | 57.57 | 13.96 | *0.08 |
| No | 194 | 5.73 | 5.73 | 60.54 | 15.17 | |||
| Have you been active in the ward of patients hospitalized with COVID-19? | Yes | 27 | 7.37 | 4.51 | *0.41 | 55.03 | 17.46 | *0.47 |
| No | 79 | 6.63 | 4.78 | 58.44 | 12.56 | |||
| Has your activity at the hospital been voluntary? | Yes | 6 | 5.16 | 5.13 | *0.93 | 54.33 | 13.82 | *0.93 |
| No | 21 | 7.9 | 4.23 | 55.23 | 18.65 | |||
| Duration of presence in hospitals and medical centers from the beginning of the pandemic outbreak | 6 month | 64 | 6.57 | 4.56 | *0.83 | 58.03 | 12.85 | *0.83 |
| 7 month or more | 42 | 7.89 | 4.89 | 56.88 | 15.64 | |||
* Kruskal–Wallis H test.
Table 4.
| Independent Variables | Unstandardized Coefficients B | Standardisted Coefficient Beta | 95% Confidence Interval for B | *P-value | R2 | |
|---|---|---|---|---|---|---|
| Grade | Bachelor | - 1.006 | - 0.099 | - 2.13 to 0.12 | 0.081 | 0.18 |
| Master of Science | - 0.956 | - 0.089 | - 2.26 to 0.35 | 0.152 | ||
| PhD | 0.368 | 0.015 | - 2.21 to 2.94 | 0.779 | ||
| General Medicine | Reference category | |||||
| Marital status | Married | - 0.554 | - 0.039 | - 4.234 to 3.127 | 0.76 | |
| Single | Reference category | |||||
| Life style | Alone | 0.453 | 0.026 | - 1.363 to 2.269 | 0.264 | |
| With spouse | - 0.505 | - 0.033 | - 4.466 to 3.456 | 0.802 | ||
| With parents | Reference category | |||||
| Social support | - 0.126 | - 0.411 | - 0.158 to 0.094 | < 0.001 | ||
4. DISCUSSION
The present study aimed to determine the relationship between hopelessness and social support in Persian-speaking students studying at the Iran University of Medical Sciences during the COVID-19 pandemic. In relation to this, diverse and expanding studies conducted since the pandemic outbreak show increased hopelessness and stress scores in different social groups [29-31]. In the present study, the mean score of hopelessness was 6.20 (0-20), with a standard deviation of 4.98. These figures are higher than similar figures in studies conducted in South Africa or the study of Kocalevent et al. (2017) [32, 33]. In the present study, approximately one-third of students reported a minimum level of hopelessness, and 6% reported a high level of hopelessness, which is consistent with the findings of a study by El-Zoghby et al. [34], who reported that more than half of Egyptian adults had severe mental health problems. Nevertheless, in the present study, all participants were students of medical sciences and thus were more exposed to patients with COVID-19, the risk of infection and subsequent transmission. In this study, participants who were members of the treatment team also reported less stress and mental distress than other community members. This lower level of hopelessness may be due to their greater awareness of the disease and methods of transmission and treatment.
In terms of social support, more than half of the students in the present study reported high social support, 39.9% reported moderate social support, and 6.5% reported low social support. In most other studies, it has been proven that hopelessness and social support are inversely related to each other, so hopelessness decreases with increasing support from family, friends or relatives [35]. Indeed, in one study conducted in the Philippines, a moderate level of social support was reported by nurses (3.95), while in our study, slightly more than a third of the samples reported a moderate level of social support, and more than half of them reported a high level of social support [36]. This difference in social support may be because medical students are not formally responsible for patients during a pandemic, while nurses are fully responsible for caring for patients with COVID-19. On the other hand, in the above study, the mean age of nurses was 30.94 years, while in our study, the mean age of participants was 23.6 years, with 219 students being female.
In a study conducted by El-Zoghby et al., a statistically significant relationship was reported between age and female gender in terms of the effect of COVID-19 on mental health [34]. While the findings of a study by Cheung et al. entitled: “The impact of COVID-19 on the mental health of elderly people” showed the important role of aging in increasing mental problems caused by the pandemic [35]. Also, in the study of Kizilkurt et al. in Turkey, women reported lower levels of mental problems than men. Despite the above reports, in another study conducted in South Africa with medical and paramedical students in the Western Cup to assess their level of depression during the COVID-19 pandemic, no statistically significant difference was found in the levels of hopelessness between men and women [32, 36]. Future studies may usefully explore why such differences may be apparent (or not).
The results of the Spearman test showed a significant and inverse relationship between hopelessness and social support among students during the COVID-19 pandemic, so with increasing social support, the level of hopelessness decreased among students. Social support comes from various sources, including family (father, mother, child or spouse), friends, and sometimes from the organization in which people work. In other studies conducted in the same region, people who lived with family and benefited from family support similarly reported a lower level of hopelessness. For example, Adelinejad and Alipour investigated the relationship between perceived social support and preventive behaviors mediated by the variables of life expectancy and mental well-being among women living in Tehran City, Iran. Study results showed a positive and significant relationship between perceived social support and mental well-being, perceived social support and life expectancy, and mental well-being and life expectancy [37]. Among students of Tabriz University of Medical Sciences in Iran, mental health scores decreased significantly with increasing social support scores [12]. Another study conducted elsewhere reported that with increasing support from family or their organization, nurses similarly reported a lower level of anxiety caused by the COVID-19 pandemic [38]. These results are in line with the results of the present study, as are the results of a study by Li et al., which equally showed the important role of support given by family and friends in reducing depression, anxiety and hopelessness [39]. The results of the above studies importantly confirm the current study results, which further adds to rich and contextualized understandings in this area.
In the present study, there was a statistically significant relationship between marital status and hopelessness during the COVID-19 pandemic, as married people had lower levels of hopelessness. Many studies in different parts of the world have reported similar results. Most married people are heads of households and are responsible for providing food, clothing and housing for other family members [35, 39]. Similar results have been found in the study of El-Zoghby et al., in which married Egyptian adults felt more stress than single people during the pandemic [34]. In addition, a descriptive study by Kizilkurt et al. in Turkey supports the findings of our study [36]. In their study, marital status was directly related to hopelessness and anxiety symptoms, as most married people were concerned about food shortages, laundry and disinfection, and even the delay in their children's education due to home quarantine [32]. In addition to all the information about the impact of social support on hopelessness, Labrague et al., in their study, showed a statistically significant and inverse relationship between social support, aggression and hopelessness among nurses, so that social support was able to reduce the harmful and stressful effects of the environment [40]. With increased social support from family and friends, the level of anxiety reduces in nurses working in COVID-19 wards. These nurses have also reported a higher level of resilience against anxiety and better job performance. These results emphasize the need to increase social support during and after a pandemic outbreak.
In the present study, the voluntary presence of students in hospitals during the outbreak of the COVID-19 pandemic did not affect their hopelessness scores. In the case of voluntary presence, people will usually participate in an activity of their own free will, and people who are afraid of illness experience more stress and are less likely to engage in such voluntary activities. Also, the social support reported by students working in hospitals during the pandemic was significantly lower than that of other students. The present study's findings are inconsistent with the study of El-Zoghby et al., in which social support among Egyptian participants increased during the COVID-19 pandemic, and they were more likely to share their concerns and stresses with family and friends [34]. This discrepancy may be explained by the fact that sometimes some people working in the intensive care unit to care for patients with COVID-19 are afraid of transmitting the disease to other people in the community, especially their family and friends, which makes them distance themselves from them. This issue, in turn, causes these people to receive less social support, and people close to them are likely to reduce contact with them for fear of possible infection transmission [39]. Other reasons for this discrepancy may be that our study examined social support in three dimensions (family, friends, and significant others), and the students received the highest level of social support from their families. Such family support may be reduced in the number of participants living in dormitories away from family. Moreover, the length of hospital stay did not affect the score of hopelessness and social support. In the present study, the hopelessness score increased with the degree level. Our research results differ from those El-Zoghby et al., in which people with postgraduate degrees reported a lower level of hopelessness and mental health problems. In addition, a study conducted in South Africa reported that undergraduate students experienced more stress and hopelessness than ordinary people in the community. According to these previous studies, it is predicted that with an increasing level of education, people become more aware of themselves and experience more stress concerning self-care [32, 34]. The results of the present study support the need for more social support for students learning during a pandemic. Nevertheless, one of the limitations of this study is the lack of full access to all students due to the covid-19 pandemic, as they could not attend the university during this time. Additionally, because this study was conducted with students, its results cannot be wholly generalizable. Future research may usefully be conducted following the COVID-19 pandemic and during the quarantine period.
CONCLUSION
The two components of social support and hopelessness are significantly and inversely related, so hopelessness decreases with increasing social support. Therefore, health care managers must make the necessary plans in this area. Married people also experience a higher level of hopelessness, as we found an inverse relationship between hopelessness and social support. Therefore, we can decrease hopelessness in married people by increasing social support from the authorities and families. Since students working in COVID-19 wards were voluntarily receiving lower levels of social support from their families and relatives, it is expected that by increasing public awareness in this area, we can, in turn, strengthen social support for these people and reduce their level of hopelessness. Given the differences between the present and previous studies, future research may usefully explore gaps in this area.
LIST OF ABBREVIATIONS
| BHS | = Beck Hopelessness Scale |
| MPSS | = Multidimensional Scale of Perceived Social Support |
AUTHORS' CONTRIBUTIONS
N.H., M.A., and L.A.F. designed the study. N.H., T.S., and M.S.H. analyzed and interpreted the data. Z.D., N.H., L.A.F. and SP wrote and revised the paper.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The present study was approved by the Research Committee of Iran University of Medical Sciences with the code: IR.IUMS.REC.1399.1049.
HUMAN AND ANIMAL RIGHTS
All the experimental protocols involving human data were per the Declaration of Helsinki guidelines in the manuscript.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the participants who were completely informed of the study's purposes and procedures. In addition, the participants were assured about the confidentiality of their information.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and analyzed during the current study are not publicly available due to the confidentiality of information, but they can be available through the corresponding author [L.A.F] upon reasonable request.
FUNDING
The present article is extracted from research funded by the Student Research Committee of Iran University of Medical Sciences, Tehran, Iran.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This article results from a research project approved by the Student Research Committee of Iran University of Medical Sciences with No: 15-2-15-18557. The author would like to thank the students who participated in this study.
SUPPLEMENTARY MATERIALS
Supplementary material is available on the Publisher’s website.


