All published articles of this journal are available on ScienceDirect.
Counseling by Acceptance and Commitment Therapy Approach on Fear of Childbirth: A Randomized Clinical Trial
Abstract
Background:
Fear of childbirth (FOC) is a common problem during pregnancy, that causes anxiety during pregnancy and severe labor pain.
Aims and Objectives
This study wants to investigate the effects of counseling during pregnancy in order to reduce the fear of childbirth (FOC). This clinical trial investigated the efficacy of acceptance and commitment therapy (ACT) on the fear of natural childbirth.
Methods:
This randomized clinical trial was conducted on 66 consenting nulliparous women. After obtaining written informed consent from each participant, those who met the inclusion criteria were eligible to enter the study. Eight 45-60 minute sessions of ACT were held for the experimental group during prenatal care. The control group received just routine prenatal care. All subjects completed the Harman’s questionnaire at baseline, immediately after, and 4 weeks after intervention. The data were analyzed using a t-test, repeated measurement ANOVA, and Chi-square tests.
Results:
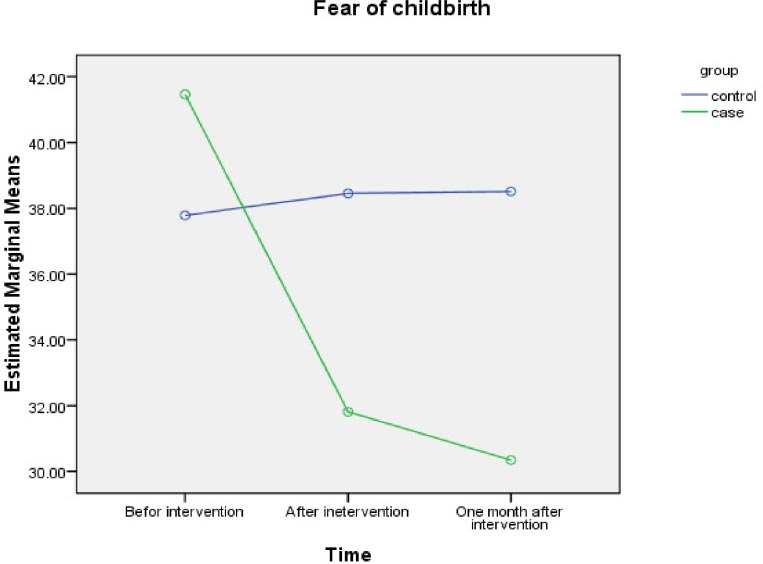
The results of the main outcome showed that the score of fear in the intervention group, from 41.47 decreased to 31.81 (p-value=0.001) immediately and 30.34 scores (p value = 0.001) 4 weeks after intervention. In control group, fear from baseline(37.79±6.85) changed to 38.45±7.01 and 38.52±7.15 in immediately and 4 weeks later (p=0.05).
Conclusion:
ACT is an effective method of reducing the fear of childbirth in nulliparous women. We recommend this method can be added to the contents of prenatal training classes.
Clinical Trial Registration No.
The registration cod is: IRCT20190910044736N2
1. BACKGROUND
Fear of childbirth(FOC) is a common problem during pregnancy [1]. It was found that 6-13% of pregnant women suffer from an intense fear of natural childbirth [2]. It is estimated that, in Iran, about 5-20% of pregnant women are afraid of natural childbirth; one in 5 pregnant women is afraid of childbirth [3]. Although mild fear is a natural response to a very first pregnancy and childbirth, intense fear of natural childbirth causes anxiety and stress in women [4]. The fear of natural childbirth is associated with increased childbirth pain, prolonged labor, low childbirth self-efficacy, and unpleasant labor experience which can have adverse effects on post-delivery such as postpartum depression [5, 6]. The reasons for fear of vaginal childbirth can include fear of labor pain, risk of injury to themselves or their newborn baby, and complications during or postpartum ward [7, 8]. The other reasons for fear of natural childbirth can include fear of perineal injury during vaginal delivery, fear of death, fear of unexpected problems, poor delivery self-efficacy, and worry about postpartum sexual problems and the baby's health [1].
Other possible outcomes of childbirth fear include increased labor pain [9] epidural analgesia [10], and cesarean birth [11]. To reduce the fear of childbirth in pregnancy, different interventions such as pharmacological [10] and non-pharmacological therapies were recommended [12-14]. Non-pharmacological therapies are preferred to pharmacological therapies since they are cheap, simple to be implemented, non-invasive, pleasant to the mother, have no interference in delivery, and adverse effects [15]. Fears that an individual feels aboutchildbirth (values, low self-esteem, history of prenatal and delivery complications), social(lack of social support, low socioeconomic level), and cultural factors [16]. The application of modern methods of counseling is of great consideration in midwifery, such as mindfulness [17] and acceptance and commitment therapy (ACT) [18, 19]. The studies have suggested ACT as an appropriate treatment for mood disorders [20], post-traumatic stress disorder [21], panic disorder [22], generalized anxiety disorder, anxiety, and quality of life during pregnancy [19, 23]. Treatment through the commitment and acceptance approach teaches the client to accept his/her thoughts and emotions and opt for new ways for his/her life and act committed [24].
ACT is a unique empirical psychological intervention and includes six core processes of acceptance, cognitive defusion, being present, self as context, valuing, and committed action for psychological flexibility. ACT teaches how to deal with the thoughts, and difficult feelings of the memories rather than avoid them, as well it teaches a person to move toward values [25]. This study was designed to assess the ACT approach regarding the fear of childbirth in pregnant women.
2. METHODS
2.1. Type of Study
This randomized clinical trial study with a parallel design was conducted on 66 nulliparous pregnant women who were referred to the health centers of Khomein City, Iran.
2.2. Sample Size
The sampling method was convenient, and the sample size was determined by the α=0.05, β=20%, as well as considering 10% for compensating for sample loss due to follow-up, 33 pregnant women were in the control and 33 in the experimental group.
2.3. Participants Recruitment
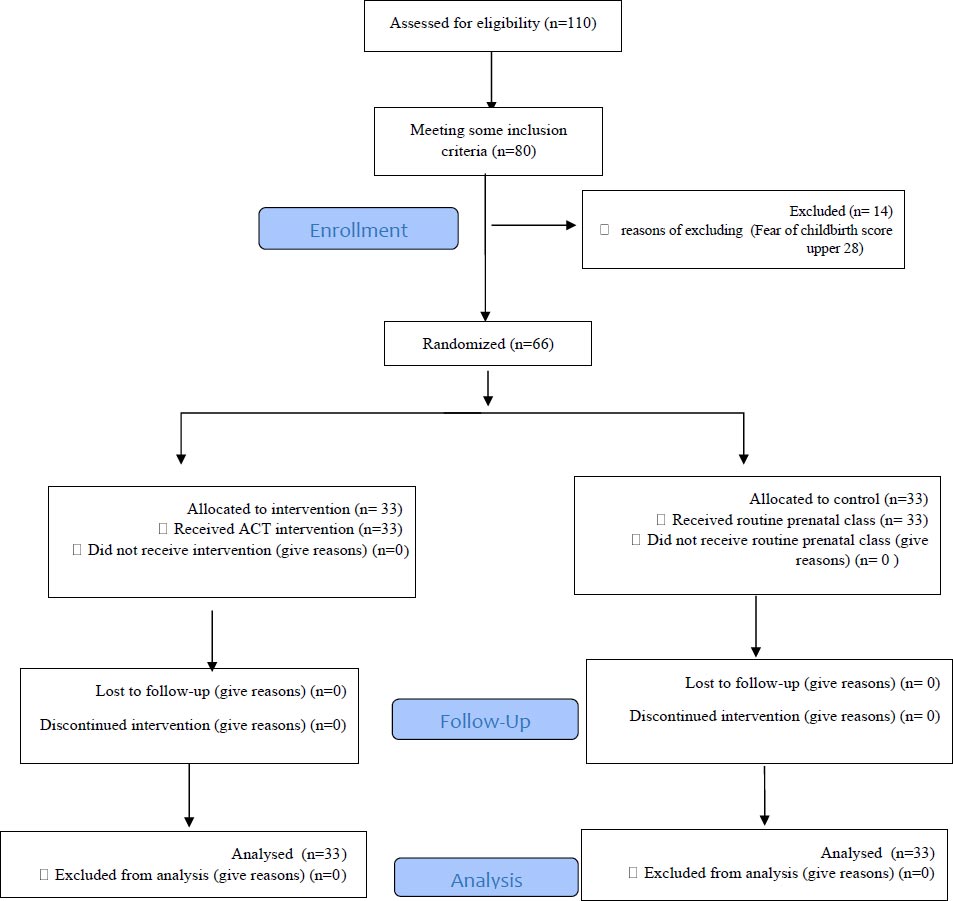
The individuals' demographic, obstetric, internal diseases, and surgical procedures information were recorded in the national health integrated system titled as (SIB). SIB is an electronic file containing recorded pregnant women, and hence, the researcher could find samples in this system. The researchers called the women who had inclusion criteria in their files. Out of 110 pregnant women, 66 who met the inclusion criteria were recruited into the study by researcher as a counselor midwife (Diagram1).
The inclusion criteria for selecting the participants for the study were as follows:
Being pregnant and in the 20th to 25th gestation weeks, nulliparous, scoring 28 or higher on Harman's questionnaire, being diagnosed as a low risk pregnancy, absence of a psychiatric disorder except for the fear of childbirth, absence of medical complications during pregnancy, and being able to read and write and prefer to cesarean if they could opt.
The exclusion criteria were unwillingness to continue with the study at any point in time; having 2 or more absences during the training classes;and presenting with any stressful condition or event during the study. They were told briefly about the scope of the study and were asked to sign a written consent. A total of 66 participants who were selected, were randomly divided into two intervention groups (A and B) using a randomized block allocation method (quadruple AA, BB). After determining the assignment sequence by Excel software using the RAND formula, the sequences were sequentially written on paper and placed in opaque closed envelopes. The envelopes were sequentially numbered.
2.4. Setting of Study
Khomein City is one of the central provinces of Iran. Khomain maternal hospital was situated in Khomain center. It serves a population of 110,000, with about 80-100 childbirth per month. The sampling method was multi-stage. Out of 10 health centers 5 of them were selected randomly. Every health center was considered as a cluster and 11 -14 samples were selected from each health center as a convenient method from May to August 2019.
2.5. Measures and Data Collection
The first part of the questionnaire addressed demographic and obstetric characteristics. The second section encompassed questions related to the Childbirth Attitudes Questionnaire (CAQ), which was developed to measure fear of childbirth [26]. Harman’s questionnaire or the childbirth attitudes questionnaire (CAQ) consisted of 14 Likert-type items, scored on a 4-point scale, ranging from never (1) to very often (4), therefore, the scores ranged from 14 to 56. High scores indicated high fear and the scores of over 28 were considered as fear of childbirth [26, 27]. The reliability of this questionnaire with Cronbach's alpha obtained 0 .84 and its validity has been established by content validity [28].
2.6. Implementation Method
The ACT intervention was conducted in eight weekly sessions of 45-60 minutes over 2 months by one midwife counselor specialist. She was a Master’s of Science in counseling and qualified in ACT approach in 40 hours workshop. On the other hand, the control group received formal prenatal care.
After 8 sessions and one month later, the participants in both groups completed Harman's Childbirth Fear (Childbirth Attitude), Table 1 summarizes the contents of the ACT sessions. Each session included assignments, group feedback, brainstorming, appropriate exercises, and a review of the content of the previous session.
2.7. Data Analysis
Data were analyzed by SPSS 24. Absolute and relative frequency distribution, in descriptive statistics of the descriptive statistics index, was used for quantitative variables. Examining the mean score of the fear outcomes in the two groups of the study, repeated measurement ANOVA was used for fear childbirth assessment. Independent-sample T test, and Chi-square were used for demographic and obstetric variables. The significance level in this study was considered to be 0.05.
3. RESULTS
The age mean of the participants in the experimental group was 26.06±4.79 and in the control group, it was 24.55±5.35 years old (P=0.233), indicating the similarity of the two groups in age (Table 2).
The results of the main outcome showed that the score of fear in the intervention group, from 41.47 decreased to 31.81 (p-value=0.001) and 30.34 score (p-value=0.00) 4 weeks after intervention (Chart 1). The ACT counseling in this study significantly decreased fears in the intervention group as compared to the control group (p=0.05) (Table 3), 22 (68.8) (out of 33) in the intervention had natural childbirth whereas, in the control group 19 (57.6) had vaginal delivery(p=0.351) (Table 4).
| ACT Protocol Per Session | Session |
| 1 | (1) Introducing the group members and the midwife counselor, (2) Explaining the rules of the group, (3)Discussing the fear of pregnancy and (4) A general description of ACT and the goals. |
| 2 | (1) Reviewing the contents of the previous session and assignments, (2) Answering the participants' questions, (3) Stressing the importance of living in the present and avoiding fusions with the past and future (4) Discussing mindfulness and practicing it in class. Homework Assignment:(1) Conscious breathing and body scan exercise, and (2) taking notes on any unpleasant thoughts and feelings. |
| 3 | (1) Reviewing the contents of the previous session and assignments, (2) Answering questions, (3& 4) Concepts of the experiential avoidance and constructive frustration, and (5) Using the metaphors of "well", and "the shovels" to clarify the two concepts. |
| 4 | (1) Reviewing the contents of the previous session and assignments, (2) Answering questions, (3&4) Acceptance of a new way of living with fear and metaphors of" un invited guest" and "bus passengers", (5) Practicing mindfulness in class, and (6) Homework" using metaphors in situations at home. |
| 5 | (1) Reviewing the contents of the previous session and assignments, (2) Answering questions, (3) Defusion: detachment from thoughts, and accepting as normal, (4) description of 3 steps for diffusion by using metaphors, (4) metaphors of "if your hands were your thoughts, and "leaves on the river", and (6) Homework: Using metaphors in domestic or home situations. |
| 6 | (1) Reviewing the content of the previous session and assignments, (2) Answering questions, Self as context, i.e., you are more than your life story, (3) Using the metaphor of "chess board", and "weather". (4) Homework: Taking notes on strategies for controlling unpleasant thoughts and feelings. |
| 7 | (1) Reviewing the content of the previous session and assignments, (2) Answering questions, (3) Values: differentiating between “values” and “goals”, (4) Using the metaphor of "compass", and "funeral", (5) The practice of value-consistent behaviors, (6) Homework :Taking notes on your personal life values and ways to prioritize them. |
| 8 | (1) Reviewing the content of the previous session and assignments, (2) Answering questions, (3) Commitment to value-consistent behavior (4) Helping the participants to use barrier management techniques while moving toward their values and helping them to learn committed action, (5) Practicing mindfulness with a focus on the completion of therapy, (6) End of the sessions and distribution of the questionnaires, thanking the participants and wishing them well. |
| - | Variable | ACT (N = 33) | Control (N = 33) | P-value |
| Education | Secondary school | 1 (2.1) | 3 (9.1) | 0.483 |
| Status | Diploma | 18 (52.1) | 19 (57. 6) | |
| Above the diploma | 14 (43.8) | 11 (33.3) | ||
| Type of Pregnancy | Planned | 23 (69.8) | 28 (84.8) | 0.124 |
| Unplanned | 10 (30.3) | 5 (15.2) | ||
| Occupation | Housewife | 27 (85.4) | 31 (93.9) | 0.214 |
| Employed | 5 (14.6) | 2 (6.1) | ||
| Abortion history | Yes | 2 (7.1) | 3 (9.1) | 0.667 |
| No | 31 (93.9) | 30 (90.9) |
| Fear of Child Birth | ACT | Control | P Value Group | P Value Time | P Value Time × Group |
| Before | 7.04 ± 41.47 | 37.79 ± 6.85 | F = 5.28 | F = 74.66 | F = 97.01 |
| After | 31.81 ± 7.02 | 38.45 ± 7.01 | P = 0.05 | P = 0.001 | P = 0.001 |
| One month later | 30.34 ± 6.61 | 38.52 ± 7.15 | - | - | - |
| Variable | ACT | Control | P-value* |
| NVD | 22 (68.8) | 19 (57.6) | 0.351 |
| C/S | 10 (31.3) | 14 (42.4) | 0.351 |
| Emergency C/S | 7 (70) | 8 (57.14) | 0.273 |
| C/S Electiveid="f | 3 (30) | 6 (42.86) | 0.273 |
4. DISCUSSION
The results indicated that acceptance and commitment therapy can significantly decrease fear of natural childbirth in the intervention group. Attending the counseling sessions, the participants had the skill to live in the moment rather than thinking about the past and future, and move towards their values by understanding their personal values.
The findings of the present study were consistent with those found by Peterson et al, who studied the effect of acceptance and commitment-based therapy on the stress of women pregnant by IVF. They showed that ACT significantly decreased stress in women pregnant by IVF, and the results were stable one month after the intervention [29]. Hence, the present study is in line with that study in that both revealed stable results. ACT is an unbiased and balanced feeling of awareness, which contributes to seeing and accepting emotions and physical phenomena as they occur. In this sense, counseling nulliparous pregnant women who suffer from spiritual and physical problems resulting from fear of natural childbirth leads them to accept their feelings and physical and mental symptoms. The original goal of ACT is fostering psychological flexibility. The individuals, through ACT, gain the ability to be aware of their thoughts and feelings and accept them if they are unpleasant and come into contact with a transcendent sense of self (observing self) [20]. They learn to live at the present time and move towards their values and goals [30]. Fear of pain, fear of death, fear of unexpected problems, poor childbirth self-efficacy, worry about postpartum sexual problems, and the baby's health are considered the main reasons for fear of childbirth [31]. People usually use avoidance strategies to cope with their fear. Pregnant women's experiential avoidance of their thoughts, experiences, feelings, and memories causes a process of trauma for the mother and her baby. In this context, one of the goals of the interventions conducted in this study was to make a change in the initial avoidance pattern.
Vakilian et al. conducted a study in 2016, aiming at investigating the effect of the ACT approach on pregnancy anxiety of pregnant women who were referred to the Health Centers of the city of Arak. The results showed no significant difference between the two groups in childbirth fear (p>0.05) [19]. This result was not in line with the results of the present study, which may be due to the different weeks of pregnancy, and a variety of instruments to evaluate childbirth fear in the two studies. In one study,11 Pregnant women (14-37 weeks’ gestation) were recruited via the UK National Health Service, attended a single-session (<3 hours) ACT intervention alongside routine antenatal care. Findings showed clinical and statistical reductions in fear of childbirth and anxiety.
In general, the results of this study showed although acceptance and commitment therapy was effective in FOC, it is not effective in the final frequency of cesarean section. However, it reduced the number of elective cesarean sections, but it was not statistically significant.
CONCLUSION
It seems that this psychological intervention can reduce the fear of childbirth by changing the attitude with an acceptance and commitment approach.
Considering the effectiveness of ACT on childbirth fear, it is suggested that obstetric and gynecological centers organize counseling sessions in this regard to help pregnant women who fear natural childbirth.
LIMITATIONS
The limitations of this study include the nulliparous pregnant women, which should be cautiously generalized to multipara women.
ETHICAL STATEMENT
The present article is part of the thesis for a Master’s degree in Midwifery Counseling approved in the Clinical Research Center of Amir Kabir Hospital under the ethical code IR.ARAKMU.REC.1397.282 by the Ethics Committee of Arak University of Medical Sciences. Also, written consent was obtained from participants.
CONSENT FOR PUBLICATION
Written consent was obtained from participants.
STANDARDS OF REPORTING
CONSORT guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This research was funded by the University of Medical Sciences of Arak as reference number 3098. The University assisted in the designing of the study and collecting and analyzing the manuscript.
CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
ACKNOWLEDGEMENTS
We hereby, thank the honorable Research Vice-Chancellor of Arak University of Medical Sciences and the professors as well as the staff in the Health Centers of the city of Khomein, who sincerely helped us in this study.


