All published articles of this journal are available on ScienceDirect.
Impact of Therapeutic Education on Asthma Control, Medication Adherence, Knowledge and Quality of Life in Moroccan Adult Asthma Patients
Abstract
Background:
Asthma is still a partially or not controlled disease in most cases despite the availability of effective treatment options. It is among the most common causes of annual intensive care unit visits and physician admissions. Therapeutic patient education can be an effective strategy to improve patients' knowledge to understand their disease and develop coping strategies. This will eventually lead to symptom control and improvement in treatment compliance and quality of life.
Objective:
This study aimed to assess the effects of a structured educational intervention on asthma control, medication compliance, asthma knowledge, and quality of life of adult asthma patients
Methods:
This study included 211 adult asthma patients over 18. The Asthma Control Test (ACT), the eight-item Morisky Medication Adherence Scale (MMAS-8), the mini Asthma Quality Life Questionnaire (mini-AQLQ), and the Adult Patient Asthma Knowledge Questionnaire (AP-AKQ) were completed both before and after the three-month educational intervention. Comparison of pre-and post-education outcomes was performed by the Wilcoxon test for quantitative variables with non-normal distribution as well as qualitative variables.
Results:
Three months after the educational intervention, there was a significant improvement (p<0.001) in ACT score from (18.00 (15.00-21.00) to 20.00 (19.00-21.00), mini-AQLQ score from 5.04 (4.44-5.72) to 5.75. (5.25-6.35), MMAS-8 score from 6.00(3.00 - 8.00) to 8.00(6.00 - 8.00) and AP-AKQ score from 39.00(36.00-43.00) to 51.00(48.00-52.00). Also, the proportion of patients with well-controlled asthma, good compliance, and higher quality of life increased significantly.
Conclusion:
Our results suggest that a structured educational intervention, with content based on patients' perceived needs, may provide benefits regarding disease control, medication adherence, quality of life, and knowledge in asthma patients.
1. INTRODUCTION
Asthma is a common chronic respiratory condition that affects approximately 300 million people worldwide, with a mortality of around 250,000 per year. Over the past decade, the goals of asthma management have shifted to focus on achieving and keeping good asthma control and reducing future risks, such as decreased lung function, asthma exacerbations, hospitalizations, adverse effects of treatment, and death [1]. Despite the availability of highly effective inhaled medications, the disease remains insufficiently controlled in a large proportion of patients. This is partly because these therapies are only effective when used correctly. 56% of asthmatics admitted not taking their controller medications daily [2] with prolonged interruptions over the long term. It's the same for inhaler handling and the peak flow meters using [3]. As a result, poor adherence leads to poor health outcomes, decreases patient well-being, and increases healthcare costs [4, 5]. However, asthma treatment includes non-pharmacological components, namely environmental control and sports practice. The goal of asthma treatment is to achieve optimal disease control: to limit chronic symptoms, especially at night, to allow normal physical activity, to prevent exacerbations and limit visits to the emergency room and hospitalizations, to maintain normal or near-normal lung function (>80% of the theoretical value) [6]. Moreover, asthma is often associated with a number of organic or functional comorbidities that worsen disease control and contribute to impaired patient quality of life (QOL) [7, 8].
The strategies for optimal asthma control include reduction of environmental risk factor exposure, assessment of asthma severity, appropriate treatment according to severity level, regular symptom and lung function monitoring, with adjustment of treatment intensity if necessary, and finally, patient education and counselling [1].
Many previous studies recommended therapeutic patient education (TPE) and self-management training to improve patients' skills and showed that education and information about the disease could help patients improve their asthma control, lung function, and QOL [9-13]. Therapeutic patient education is a structured, ongoing process integrated into care and centered on the patient, comprising organized activities, including psychosocial support, designed to make patients aware and informed about their illness and about hospital care, organization and procedures, and health and illness-related behaviours [14]. It aims to enable patients and their families to acquire and maintain the self-care and coping skills necessary to manage their lives with a chronic illness [15].
Thus, asthma education is considered by current asthma guidelines and strategies as an important component of bronchial asthma management and is recommended with the highest level of evidence [1]. It can help patients improve their asthma control and lung function, reduce the frequency of asthma attacks and nocturnal respiratory disorders, decrease the number of hospitalizations, emergency room visits, unscheduled medical visits and days of absence from school or work and eventually enhance the asthma patient's quality of life [16].
The purpose of this study was to investigate the effect of a structured TPE program on asthma control, medication adherence, knowledge, and QOL in adult asthma patients.
2. MATERIALS AND METHODS
2.1. Study Design
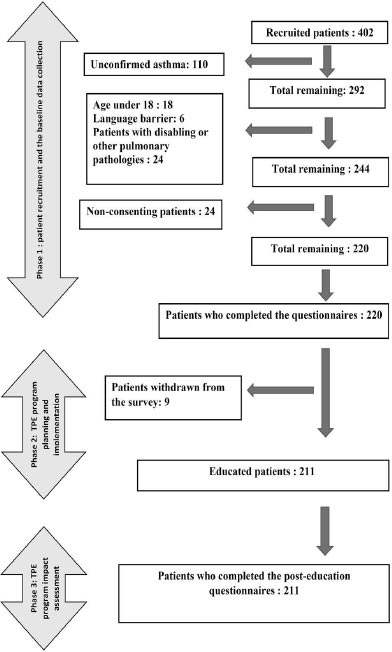
We conducted a quasi-experimental study among 220 adult asthma patients consulting at the University Hospital of Fez. The study was performed in three phases (Fig. 1). The first phase included patient recruitment and baseline data collection. It lasted four months (March to May 2022). In the second phase, which lasted two months (June-July 2022), educational sessions were planned and implemented. Three months later, the third phase focused on a post educational intervention evaluation through data collection using the same instruments.
2.2. Patients and Sampling
The minimum sample size required was estimated at 156 participants by G*Power software [17], to provide the effect size of 0.2 in ACT score change calculated from a pilot study in which the ACT score after the educational intervention increased from 19.4±14.1 to 20.4±2.8. A study power of 80% was set, with a 2-sided significance level of 0.05. Afterward, it was considered that 15% of the participants could withdraw from the study, so the final sample size required was 180.
Finally, we enrolled 220 adult patients with asthma who were at least 18 years old and whose asthma had been confirmed by functional and clinical investigation for at least six months. Patients with disabling or pulmonary pathologies other than asthma and those with language barriers were excluded. Nine patients withdrew before the educational intervention. Only 211 patients participated in the educational sessions and completed the evaluative phase.
2.3. Data Collection Tools
2.2.1. Asthma Control Measurement
The Arabic version of Asthma Control Test (ACT) was used to assess asthma control. The internal consistency reliability was Cronbach's Alpha = 0.92 [18] (for our population Cronbach's Alpha = 0.918) . It is a five-question questionnaire with a 5-point scale ranging from 1 (reporting the respective symptom all or very frequently) to 5. (never reporting the respective symptom). The total ACT score ranges from 5 to 25. An ACT score of 15 indicates uncontrolled asthma, a score of 15 to 19 implies partially controlled asthma, and a score of 20 to 25 indicates well-controlled asthma [19].
2.3.2. Medication Compliance Measurement
Compliance was assessed using the Arabic version of the eight-item Morisky Medication Adherence Scale validated by Ashur et al. [20] and successfully used in several studies on Arab populations [21]. Our asthma patients' reliability and validity showed excellent psychometric properties (Cronbach's Alpha = 0.886). Each answer has a defined value. Adding the values for each question yields a score between 0 and 8. A value = 8 means good compliance. A score between 6 and 7 means average compliance. A value < 6 signifies poor compliance [22-24].
2.3.3. Knowledge Assessment
Asthma knowledge was assessed by the 54-item Adult Patient Knowledge Questionnaire (AP-AKQ), which consists of four sections: “Pathophysiology of asthma: 13 items”; “Triggers: 15 items”; “Diagnosis and management: 19 items”; and “Asthma treatment: 7 items”. It was developed by experts in the field after consulting 18 surveys and the GINA documents on asthma knowledge that every patient should have [25]. A reliability assessment of the Arabic version revealed an acceptable Cronbach's Alpha (0.762). Content validity was attested by a team of experts, including a psychologist, a pulmonologist and an expert in educational sciences.
The scores were considered dichotomous “correct/incorrect answer”, a “don't know” answer was considered incorrect. An answer key was used to score the questionnaire. A score of 1 was assigned to each correct answer and a score of 0 to each incorrect answer. The total score ranged from 0 to 54 [26].
2.3.4. Quality of Life Assessment
The mini-AQLQ measured QOL validated Arabic version for adult patients with 15 items [27, 28]. The reliability tested in our patients was very satisfactory, with a Cronbach's alpha score equal to 0.915. The survey is divided into four domains: symptoms (5 items), activity limitation (4 items), emotional function (3 items), and environmental stimuli (3 items). Patients respond to each item on a seven-point scale, and results are reported as the mean score of all items (1: extremely impaired, to 7: no impairment). Quality of life was considered good when the overall score is ≥ 6, average between 4 and 6 and poor below 4 [29].
2.4. The Educational Intervention
The educational content was developed in response to the patient’s expressed needs. The main components of the educational program were: disease characteristics, symptoms, causes, complications, inhalation technique, the action of medications and their potential side effects, the difference between rescue and control medications, dosing regimen, goals of asthma treatment, improving compliance, use of peak flow meter, triggers and their avoidance, recognition, and action in case of asthma attack, smoking cessation, general recommendations on nutrition, physical activity, sleep, and vaccination. Furthermore, patients were given a hands-on demonstration and training in inhalation technique, inhaler cleaning, and storage. All participants received two-hour group sessions (10-12 patients) at 2-week intervals.
The program was based on an interventional educational framework tailored to the patient's characteristics and the study's theoretical framework: the Reasoned Action Approach (RAA). For this purpose, transformative learning, an intervention framework based on adult learning theory, was chosen. It is a learner-centered approach to gaining confidence in new roles and relationships [30]. Furthermore, educational programs based on this theory have yielded promising results in preventing unhealthy behaviors [31, 32].
2.5. Statistical Data
Data were analyzed using IBM SPSS statistics (version 25) software. Descriptive analysis included frequency and percentage for categorical variables. Based on the normality assumption, the continuous variables were described by a mean ± standard deviation or by a median with an interquartile range. Comparison of pre-and post-education outcomes was performed by the Wilcoxon test for quantitative variables with non-normal distribution and qualitative variables. The normality of continuous variables was verified by Kolmogorov-Smirnov. P-values < 0.05 were considered significant.
2.6. Ethical Considerations
The study was approved by the local ethics committee under number 15/2022. Before the investigation, each participant signed a written informed consent to participate in the study. The informed consent contained detailed information about the purpose and relevance of the study so that participants could make an informed choice about whether to participate or withdraw at any time if they wished. Also, the following considerations were guaranteed: voluntary participation; anonymity; confidentiality; and protection from any harm.
3. RESULTS
The survey included 211 patients, and the primary outcome was asthma control (using the ACT). Other endpoints were medication compliance, knowledge, and quality of life. Two hundred and eleven patients completed pre- and post-education questionnaires and participated in educational sessions.
Patients mean age was 48.67± 15.36 years (Table 1). 72.04% were women, 72.04% were married, half (50.71%) were not attending school, and 76.78% lived in urban areas. Regarding smoking status, 67.77% were non-smokers. The median years with asthma was 7.00 (3.00 -1.00). Only 25.59% were covered by health insurance. The detailed demographic profile of the participants can be seen in Table 1.
The primary outcome was asthma control (using ACT). The proportion of patients with well-controlled asthma increased significantly from 39.81% to 62.56% after three months of the educational intervention, while the proportion of patients with uncontrolled asthma decreased significantly from 25.12% to 1.89% (p ˂0.001). The median ACT score increased from 18.00 (15.00-21.00) to 20.00 (19.00-21.00) (p ˂0.001) (Table 2).
| - | Categories | Effective (n=211) | Percentage (%) | Mean ±SD |
|---|---|---|---|---|
| Gender | Femal | 152 | 72.04 | - |
| Male | 59 | 27.96 | - | |
| Age | - | - | - | 48.67 ± 15.36 |
| Duration of asthma | - | - | - | 7.00 (3.00 -1.00) * |
| BMI | - | - | - | 26.92 ± 4.47 |
| Marital status | Single | 35 | 16.59 | - |
| Married | 152 | 72.04 | - | |
| Divorced | 8 | 3.79 | - | |
| Widowed | 16 | 7.58 | - | |
| Educational level | No schooling | 107 | 50.71 | - |
| Primary | 51 | 24.17 | - | |
| Secondary | 38 | 18.01 | - | |
| Higher | 15 | 7.11 | - | |
| Residence | Urbain | 162 | 76.78 | - |
| Rural | 49 | 23.22 | - | |
| Coverage by health insurance | Yes | 54 | 25.59 | - |
| No | 157 | 74.41 | - | |
| Smoking status | Ex-smoker | 30 | 14.22 | - |
| Non-smoker | 143 | 67.77 | - | |
| Passive smoker | 37 | 17.54 | - | |
| Active smoker | 1 | 0.47 | - |
*: median (interquartile range)
| Variable | Responses | Baseline | 3-month Visit | P-value |
|---|---|---|---|---|
| Asthma control | ACT score, median (Interquartile range) |
18.00 (15.00-21.00) | 20.00 (19.00-21.00) | ˂0,001 |
| Well-controlled, n (%) | 84 (39.81) | 132 (62.56) | ˂0,001 | |
| Partially controlled, n (%) | 74 (35.07) | 75 (35.55) | ||
| Uncontrolled, n(%) | 53 (25.12) | 4 (1.89) | ||
| Asthma knowledge | AP-AKQ Score, median (Interquartile range) |
39.00 (36.00-43.00) | 51.00 (48.00-52.00) | ˂0,001 |
| Medication adherence | MMAS-8 score, median (interquartile range) | 6.00 (3.00 - 8.00) | 8.00 (6.00 - 8.00) | ˂0,001 |
| High adherence, n (%) | 91 (43.13) | 133 (63.03) | ˂0,001 | |
| Medium adherence, n (%) | 29 (13.74) | 49 (23.22) | ||
| Low adherence, n (%) | 91 (43.13) | 29 (13,75) | ||
| Quality of life | Mini-AQLQ score, median (interquartile rang) | 5.04 (4.44-5.72) | 5.75 (5.25-6.35) | ˂0,001 |
| Good QOL, n(%) | 38 (18.01) | 95 (45.02) | ˂0,001 | |
| Average QOL, n(%) | 148 (70.14) | 113 (53.56) | ||
| Low QOL, n(%) | 25 (11.85) | 3 (1.42) |
ACT: asthma control test
AP-AKQ-AP: adult patient asthma knowledge questionnaire
MMAS-8: The eight-item Morisky Medication Adherence Scal
Other endpoints were medication adherence, knowledge, and quality of life. Regarding compliance, The Morisky score improved significantly (p˂0.001) from 6.00(3.00 - 8.00) to 8.00(6.00 - 8.00), and the percentage of patients with good compliance increased from 43.13% to 63.03%, while one of patients with poor compliance decreased from 43.13% to 13.75% (p˂0.001).
Three months after TPE, the Mini-AQLQ score for quality of life improved significantly (p˂0.001) from 5.04 (4.44-5.72) to 5.75. (5.25-6.35). Similarly, the proportion of patients with a good quality of life increased from 18.01% to 45.02%, while those with a poor quality of life decreased from 11.85 to 1.42%.
Finally, there was a significant improvement in the score knowledge, which significantly improved from 38.85±5.37 to 50.08 ± 2.62 after education (p˂0.001).
4. DISCUSSION
Therapeutic patient education is a nonpharmacological intervention that assists patients and their families in developing or maintaining the skills required for managing their chronic disease. Several previous studies back up the hypothesis that therapeutic patient education is critical for improving asthma patient knowledge, disease self-management, and attack prevention [13, 33].
There was no control group in our study. We used pre-education data as a control and compared it to post-education data. We educated our patients on the pathophysiology of asthma, its causes, complications, inhalation technique, medication action and potential side effects, triggers, and their avoidance, warning signs of attack, attack management, and healthy lifestyle rules.
This study was therefore conducted to examine the effect of a structured asthma TPE program based on participants' perceived needs on asthma control and asthma knowledge and quality of life in adult asthma patients. We postulated that TPE would improve asthma knowledge and, as a result, disease control and quality of life in Moroccan adult asthma patients. And according to our findings, we confirmed this hypothesis.
We have proved the importance of an educational intervention over a short period (3 months). This enhanced the participants' asthma knowledge, disease control, medication compliance, and quality of life. This improvement occurred even without changing the patients' previous pharmacological treatment, thus showing the importance of the educational approach in asthma management. The observed improvement in asthma control, medication compliance, and quality of life can be attributed to an increase in patients' knowledge as a result of an educational intervention that covered multiple aspects of the condition.
After asthma education, there was a highly significant improvement in the level of asthma control (the primary goal of long-term management) in our study. This was consistent with several studies [11, 12, 16, 34, 35] that showed significant improvement in asthma control after asthma education in adults and children using the Asthma Control Test (ACT). Other studies, however, did not show a significant effect of asthma education on asthma control as assessed by the number of symptom-free days, daily peak flow measurement, or ACT score [13, 36-38].
In terms of medication adherence, our results showed an improvement in its score with a significant increase in the proportion of participants with good adherence. Similarly, recent reviews have shown a positive impact of pharmacist-led interventions on inhaler technique and medication adherence in adult asthma patients [39-41]. Also, many studies have reported improved compliance after educational interventions with adult and pediatric asthma patients [37, 42, 43]. In Turkey, nevertheless, a randomized controlled trial did not reveal a statistically significant difference between the Morisky Medication Adherence Scale scores in the intervention and control groups in medication compliance [44]. Medication compliance in asthma patients decreases with age, particularly from adolescence onwards. There are several reasons for poor compliance: the complexity of the treatments, difficulties in using the inhalers, lack of understanding or perception of their benefits and fear of side effects. Hence, poor compliance is associated with risks of unnecessary therapeutic escalation and worsening of asthma, with more exacerbations, increased school absenteeism, deterioration of quality of life, and even excess mortality. The management of non-compliance implies a good caregiver/asthmatics relationship, better provider training and personalized patient education [45].
Regarding QOL, it’s a very broad concept influenced in a complex way by the individual's physical health, psychological state, level of independence, social relationships and relationship to the essential elements of the environment. For an asthmatic, a good quality of life means not being hampered by the disease and being able to carry out activities and projects without being hampered by respiratory symptoms. A good QOL for an asthmatic also means not having to live with the constant fear of an attack, not being woken up at night by a cough and the risk of visiting the emergency room.The impact of TPE on the quality of life of asthma patients has been assessed in several studies. In some of them, there was no difference in the quality of life, such as the one conducted by Perry et al. among asthmatic children [37]. Whereas in others, there was an improvement in QOL scores after educational interventions [46, 47] using asthma-specific questionnaires. Recently, Felix et al. study assessed the quality of life change measured by the AQLQ questionnaire after education. There was an improvement in the intervention group after four and eight weeks (p = 0.005) [13].
Finally,a recent survey in Morocco found that the five dimensions of quality of life measured by the EUROQOL questionnaire were significantly satisfactory after three months of educational intervention [34]. The 5-dimensional EUROQOL questionnaire is not specific for asthma but rather generic for all diseases [48].
Further, effective asthma management requires that patients should have specific knowledge in order to control their asthma. Accordingly, patients should recognize: the pathophysiology of asthma and the lung changes underlying the disease, the role of different medications used in the treatment of asthma, self-monitoring and the use of inhalers and spacer devices, environmental controls (asthma triggers), and the signs and symptoms of uncontrolled asthma that may indicate an exacerbation [49].
For asthma knowledge, a very significant improvement in the score was revealed by our study. A better knowledge of asthma will assist patients in understanding the necessity of maintaining their disease under control [39]. Similarly, other studies among adult and teenage asthma patients have shown similar results [10, 50, 51].
CONCLUSION
Our findings suggest that an educational intervention may improve asthma patients' disease control, medication adherence, quality of life, and knowledge. However, these findings must be interpreted in light of the study's limitations. First, there was no control group in the study. Second, patients agreed to participate in the study voluntarily, and it is to be expected that patients will be highly motivated to participate in self-care education, resulting in higher outcome estimates.
STUDY LIMITATIONS
Our study had no control group, but the pre-PET program results were used as a control. Furthermore, the follow-up time after the educational intervention was limited to three months, whereas behavior change is a long-term process.
LIST OF ABBREVIATIONS
| ACT | = The Asthma Control Test |
| MMAS-8 | = The Eight-item Morisky Medication Adherence Scale |
| Mini-AQLQ | = The Mini Asthma Quality Life Questionnaire |
| AP-AKQ | = The Adult Patient Asthma Knowledge Questionnaire |
| RAA | = The Reasoned Action Approach |
| QOL | = Quality of life |
| TPE | = Therapeutic Patient Education |
| BMI | = Body Mass Index |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the local ethics committee under number 15/2022. Before the investigation, each participant signed a written informed consent to participate in the study. The informed consent contained detailed information about the purpose and relevance of the study so that participants could make an informed choice about whether to participate or withdraw at any time. Also, the following considerations were guaranteed: voluntary participation; anonymity; confidentiality; and protection from any harm.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were by the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ACKNOWLEDGEMENTS
We would like to thank all the patients who participated in the study. We also thank all the health professionals of the pneumology department of the CHU Hassan II of Fez for their support throughout this study.


