Evaluating the Safety and Efficacy of Manual Lymphatic Drainage with Thai Traditional Massage on Breast Milk Volume, Breast Pain and Engorgement in Post-Cesarean Mothers of Preterm Infants: A Randomized Controlled Trial
Abstract
Background:
Less breast milk, breast pain, and engorgement are issues that the majority of postpartum mothers have to confront and overcome.
Objective:
This study examined the efficacy of Manual Lymphatic Drainage (MLD), Thai Traditional Massage (TTM), and standard post-partum nursing care on breast milk volume, breast pain, and engorgement in post-cesarean mothers of preterm infants.
Methods:
Thirty-two participants were randomly divided into 2 groups: an intervention group receiving MLD, TTM, and standard post-partum nursing care (n=16), and a control group receiving standard post-partum nursing care alone (n=16). Outcomes were assessed through breast milk volume, breast pain and engorgement scores, and participant satisfaction.
Results:
The study showed that the group receiving MLD, TTM, and standard post-partum nursing care had a safe and equivalent level of breast milk production compared to the control group. Additionally, there were no significant differences between groups regarding daily milk expression frequency, breast pain, and engorgement over seven days (p>0.05). However, the experimental group expressed a high level of satisfaction with the MLD, TTM, and standard post-partum nursing care interventions.
Conclusion:
The combination of MLD, TTM, and standard post-partum nursing care could be a viable alternative for managing post-cesarean care in mothers with preterm infants.
Clinical Trial Reg Number:
TCTR20230330002.
1. INTRODUCTION
Breast milk is widely regarded as the ideal source of nutrition for newborns during their early stages of life, as it provides numerous short and long-term advantages for both infants and mothers [1]. For example, breastfeeding protects infants from infections and malocclusion, as well as promoting increased intelligence and potentially reducing the risk of obesity and diabetes. Additionally, breastfeeding mothers may experience protection from breast cancer, improved birth spacing, and potential protection from ovarian cancer and type 2 diabetes [2]. It is estimated that suboptimal breastfeeding contributes to nearly 600,000 annual child deaths from pneumonia and diarrhea, along with almost 100,000 annual deaths of women from breast and ovarian cancer [3]. Previous research indicated that premature birth is a significant risk factor for adverse breastfeeding outcomes. Preterm infants often struggle to establish breastfeeding due to underdeveloped sucking reflexes, problems with latching onto the breast, and underdeveloped digestive systems. This often leads to shorter durations of breastfeeding compared to infants born at full term. Moreover, mothers who have had a cesarean section may also encounter challenges in starting and sustaining breastfeeding, though the specific effects of a cesarean section on breastfeeding outcomes can vary [4, 5].
Nowadays, The World Health Organization (WHO) strongly recommends exclusive breastfeeding (EBF) in the first six months after birth and continued breastfeeding for up to two years [6]. However, the prevalence of EBF in the first 6 months of life in different countries has been still low rate due to obstacles and barriers [7]. In Thailand, breastfeeding rates are even lower than the global average and seem to be off track to achieve [8]. The most essential reason behind this situation was poor breastmilk production in mothers and half of mothers have problems with insufficient breastmilk supply especially in the first week after delivery [9]. Studies have shown the most common reasons for cessation of breastfeeding were due to difficulties latching to the nipple, cracked and/or tender nipples, painful breasts, and engorged breasts, which may lead to the temporary or permanent cessation of breastfeeding [10, 11]. Therefore, this is an important issue in helping mothers who suffer from this situation. Treatment methods currently used for the aforementioned breastfeeding problems range from pain relief medication, antibiotics, surgical drainage of the affected breast, and ultrasound to cold packs, cabbage leaves, and various other ointments [12, 13]. Furthermore, non-pharmacological interventions have been shown to be effective. Among them is breast massage, it is one such treatment that is used throughout the world and aims to relieve symptoms of breastfeeding problems [14]. There are different approaches to breast massage including the Oketani Lactation Management Breast Massage, Gua Sha therapy, and general massage of breast tissue. Most studies of breast massage report positive results for resolving blocked ducts, increasing milk supply, reducing breast pain, and reducing breast engorgement [15]. Manual lymphatic drainage (MLD) is also the most well-known treatment, which is a massage technique that stimulates lymphatic contractility through gentle, directed stretching of the skin. In addition, decongestive lymphatic therapy includes skin care, serial application of multilayer bandaging, and exercise (gentle, repetitive contraction of the musculature beneath the bandages) [16]. Whereas Thai Traditional Massage (TTM) is performed by those with chronic pain to alleviate pain symptoms. In addition, a growing body of research studies the efficacy of TTM in lowering the severity of chronic pain [17, 18]. Both these types of massage can be used in pregnancy and with post-pregnancy problems such as nipple problems, occluded ducts, breast pain, and engorgement because it has these properties and can relieve breast symptoms [19, 20]. However, no studies have specifically examined the effect of the combination of MLD and TTM. Therefore, this study aimed to evaluate the safety and effectiveness of MLD combined with TTM plus the standard nursing care in postnatal care by measuring breast milk volume, breast pain, and engorgement.
2. MATERIALS AND METHODS
2.1. Study Design
This study was a well-designed randomized controlled trial (RCT) to compare the effects of MLD plus TTM along with standard post-partum nursing care versus standard post-partum nursing care alone on breast milk volume, breast pain, and breast engorgement in mothers who have undergone cesarean section and have a preterm infant. The study took place at Thammasat Hospital in Pathum Thani Province, Thailand, from April 2022 to November 2022 and the results were collected using questionnaires and measuring breast milk volume.
2.2. Participants and Sample Size
Thirty-two participants were enrolled by sample size calculation from Jones, E., Dimmock, P. W., & Spencer, S. A.,2001 [21]. showing the mean and standard deviation of the milk volume from previous research in the breast massage group was 125 ± 31.55 and in the control group was 88 ± 18.93 milliliter. The sample size was calculated by using a formula for the estimation of two groups, Stata program with statistic error is 0.05 (α-error), power 0.9. This study requires a minimum of 11 participants in each group to reduce the risk of randomization bias. Additionally, 5 participants per group were added to account for potential dropout. Therefore, this study has 32 mothers who have undergone cesarean section to be a participant. Inclusion criteria were 1) mothers who have undergone cesarean section and have a preterm infant with a gestation age between 28 to 34 weeks 2) the infant must be admitted to the hospital at least 7 days after birth 3) Age of mother must be above 18-year-olds. 4) Mother must have a normal physical of nipple and breast. 5) No multi-fetal pregnancy and must not have complications after giving birth 6) No mental health complication or signs of postpartum blue 7) No contraindications to breastfeeding such as HIV pregnancy. 8) The mother must not have a history of drug use which might affect the lactation process. 9) Must not receive drugs or supplements to increase lactation and 10) No cigarette-smoking, drug-use, or alcohol-consumption habits. During the study period, the subjects were not allowed to take any other medications or supplements. The study was conducted with written informed consent and participants were able to withdraw at any time.
2.3. Intervention and Outcome
This study design was a randomized controlled trial, which is a type of experimental study design used for comparing the safety and efficacy of an intervention with a control group. The use of randomization helps to control potential confounders and bias, and this study used a block of 4 randomization to ensure that the two groups were balanced with respect to the number of participants in each group. The interventions included a group that received MLD, a gentle skin-stretching massage along the lymphatic pathways in the breast area, in addition to TTM in the back, shoulders, and posterior region, based on the principles of Thai traditional medicine. Both MLD and TTM were administered once, for one hour, within 24 hours postpartum. This group also received standard post-partum nursing care, whereas the control group received only the standard post-partum nursing care. The primary outcome measures in this study are the amount of milk volume from day 1 to day 7, while secondary outcome measures include the level of breast pain and breast engorgement from day 1 to day 3. These outcomes are important for evaluating the effectiveness of the intervention in promoting lactation and reducing discomfort in postpartum mothers.
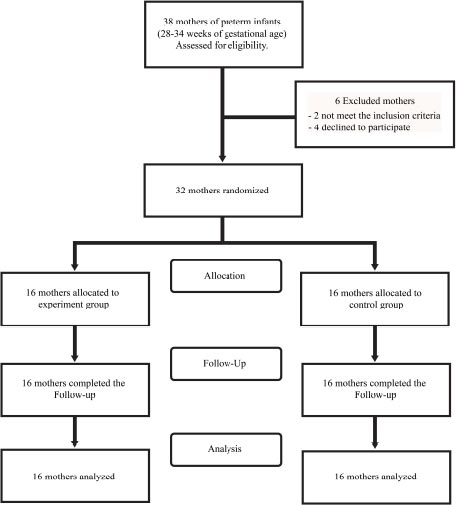
Overall, this study design provided a scientifically rigorous approach to evaluating the effects of MLD plus TTM intervention on postpartum mothers. To measure the amount of milk that is expressed by a mother during each pumping session, participants used a simple measuring device such as a syringe or container specifically designed for this purpose by using the breast pump to express the milk. As soon as the pumping session was completed, the expressed milk was poured into the measuring device. The amount of milk was recorded and expressed in milliliters (mL) or ounces (oz). This process for each pumping session was repeated throughout the day and track of the total amount of milk expressed each day was kept. Participants could borrow electronic breast pumping devices during the study period. To measuring a painful from breast and breast engorgement by using a normal pain scale [22], there are 4 levels of pain; score 0 = no pain, score 1-3 = slight pain, score 4-7 = moderate pain, and score 8-10 = severe pain and breast engorgement scale adapted from a six-point engorgement. The validity and reliability of this scale have been previously reported [23]. The scale is operationally defined as follows; 0 = no breast engorgement, 1-2 soft, no change to slight change, 3-4 = firm, non-tender to beginning tenderness, 5-6 = firm to very firm, tender to very tender. The study flow chart is shown in Fig. (1).
2.4. Data Analysis
The data were analyzed using the Stata software for the Windows operating system. The results have been presented in the form of descriptive statistics, including frequency, percentage, mean, and standard deviation. To compare the differences between groups, the breast milk volume was reported using the median (interquartile range, IQR) and assessed through the Wilcoxon rank-sum test. Concurrently, breast pain and engorgement were documented as frequency and percentage, with their comparative analysis being conducted via Fisher's exact test. P-values less than 0.05 were considered statically significant.
3. RESULTS
3.1. Baseline Demographic and Clinical Characteristics of Participants
Out of the 38 potential study participants, 32 mothers met the inclusion criteria and agreed to participate. They were divided into two groups: 16 mothers in the control group and 16 in the experimental group. Demographic information for the mothers is presented in Table 1. No statistically significant differences were observed between the two groups in terms of marital status, education level, occupation, monthly income, underlying health conditions, smoking, and drinking status. Additionally, there were no differences between the two groups in terms of maternal baseline information such as gestational age, parity (number of births), history of abortion, history of neonatal tracheal intubation, and infant birth weight. The clinical characteristics of the participants, including age, body weight, height, BMI, and vital signs (blood pressure, pulse rate, and respiratory rate), did not show any significant differences between the groups, as shown in Table 1.
| Characteristics | Experiment Group (n=16) |
Control Group (n=16) |
P-value | ||
|---|---|---|---|---|---|
| n (%) | Mean ± SD | n (%) | Mean ± SD | ||
| Age (year) | - | 31.63 ± 6.51 | - | 35.31 ± 7.56 | 0.150 |
| Marital status | |||||
| Single | 2 (12.50) | - | 0 (0.00) | - | 0.484 |
| Married | 14 (87.50) | - | 16 (100.00) | - | |
| Maternal education | |||||
| Bachelor | 6 (37.50) | - | 6 (37.50) | - | 1.000 |
| Postgraduate | 10 (62.50) | - | 10 (62.50) | - | |
| Occupation | |||||
| Unemployed | 4 (25.00) | - | 1 (6.25) | - | 0.089 |
| Merchant | 1 (6.25) | - | 1 (6.25) | - | |
| Employed | 3 (18.75) | - | 4 (25.00) | - | |
| officer | 5 (31.25) | - | 1 (6.25) | - | |
| Other | 3 (18.75) | - | 9 (56.25) | - | |
| Income | |||||
| ≤ 15,000 | 12 (75.00) | - | 6 (37.50) | - | 0.073 |
| > 15,000 | 4 (25.00) | - | 10 (62.50) | - | |
| Weight (kg) | - | 64.84 ± 12.00 | - | 59.59 ± 12.40 | 0.233 |
| Height (cm) | - | 161.44 ± 5.55 | - | 156.06 ± 7.89 | 0.053 |
| BMI | - | 24.91 ± 4.78 | - | 24.44 ± 4.51 | 0.774 |
| Vital signs | |||||
| Blood pressure | |||||
| Systolic | - | 127.44 ± 7.48 | - | 124.25 ± 5.78 | 0.188 |
| Diastolic | - | 83.81 ± 4.55 | - | 83.38 ± 4.57 | 0.788 |
| Pulse rate | - | 83.44 ± 3.76 | - | 82.56 ± 3.56 | 0.504 |
| Respiratory rate | - | 18.44 ± 1.31 | - | 18.63 ± 1.36 | 0.695 |
| Underlying disease | |||||
| No | 14 (87.50) | - | 11 (68.75) | - | 0.394 |
| Yes | 2 (12.50) | - | 5 (31.25) | - | |
| History of smoking | |||||
| No smoking | 16 (100.00) | - | 16 (100.00) | - | - |
| Smoking | 0 (0.00) | - | 0 (0.00) | - | |
| History of alcohol drinking | |||||
| No drinking | 16 (100.00) | - | 16 (100.00) | - | - |
| Drinking | 0 (0.00) | - | 0 (0.00) | - | |
| Birth order | |||||
| First child | 7 (43.75) | - | 5 (31.25) | - | 0.716 |
| Second child above | 9 (56.25) | - | 11(68.75) | - | |
| History of abortion | |||||
| No | 12 (75.00) | - | 13 (81.25) | - | 1.000 |
| Yes | 4 (25.00) | - | 3 (18.75) | - | |
| Child on Intubation | |||||
| No | 10 (62.50) | - | 13 (81.25) | - | 0.433 |
| Yes | 6 (37.50) | - | 3 (18.75) | - | |
| Gestational age (wk) | - | 32.06 ± 1.24 | - | 31.63 ± 1.36 | 0.349 |
| Infant birth weight (g) | - | 1,703.69 ± 211.66 | - | 1,633.5 ± 336.25 | 0.485 |

3.2. Safety
This statement indicates that there were some mild side effects observed in 2 participants in the experiment group, but they were resolved quickly and were not serious in nature. The red marks in the massage area were reported, but there were no reports of itching or pain, and the complaints were resolved after 20 minutes. This suggests that the intervention being studied may have some mild, short-lived side effects, but overall, it was considered safe.
3.3. The Efficacy between 2 Groups in Breast Milk Volume
The result showed that in the frequency of milk expression daily, the experiment group had a median frequency of 2.5 (IQR 1,4) on day 1, which was slightly lower than the control group’s median frequency of 3 (IQR 2,4), although this difference was not statistically significant (p=0.605). Similarly, the experiment group’s median frequency was comparable to the control group’s median frequency for days 2-7, and the differences were not statistically significant (p>0.05). Regarding breast milk volume, there was no significant difference in median breast milk volume between the experiment and control groups on any of the seven days (p>0.05). On day 1, the experiment group had a median breast milk volume of 0.1 (IQR 0, 2.11), while the control group had a median breast milk volume of 0 (IQR 0, 4.6). However, the difference was not statistically significant (p=0.803). Similarly, on days 2-7, the median breast milk volume was comparable between the two groups, and the differences were not statistically significant (p>0.05), as shown in Table 2 and Fig. (2).
| Parameter | Experiment Group (n=16) | Control Group (n=16) | P-value |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| Frequency of milk expression | - | - | - |
| Day 1 | 2.5 (1,4) | 3 (2,4) | 0.605 |
| Day 2 | 6.5 (3,7.5) | 7 (5.5,7.5) | 0.396 |
| Day 3 | 6.5 (5,8) | 6.5 (4,7) | 0.539 |
| Day 4 | 6 (5,8) | 7 (5,8) | 0.527 |
| Day 5 | 7 (4.5,8) | 7 (5.5,7.5) | 0.847 |
| Day 6 | 7 (5,8) | 8 (5,8) | 0.353 |
| Day 7 | 7 (7,8) | 8 (5,8) | 0.604 |
| Breast milk volume | - | - | - |
| Day 1 | 0.1 (0,2.11) | 0 (0,4.6) | 0.803 |
| Day 2 | 2.51 (0.25,12.15) | 1.15 (0,11.8) | 0.376 |
| Day 3 | 15.9 (2,110) | 14 (5.9,129) | 0.910 |
| Day 4 | 127.8 (7.1,207.5) | 140 (30.35,198) | 0.763 |
| Day 5 | 122.5 (26.5,350.5) | 190 (17.5,300) | 0.734 |
| Day 6 | 202.5 (19.3,567.5) | 260 (155,355) | 0.792 |
| Day 7 | 325 (23,655) | 345 (162.5, 490) | 0.925 |
| Parameter | Day 1 | Day 2 | Day 3 | |||
|---|---|---|---|---|---|---|
| Experiment | Control | Experiment | Control | Experiment | Control | |
| Breast engorgement | ||||||
| No breast engorgement | 10 (62.50) | 9 (56.25) | 7 (43.75) | 8 (50.00) | 7 (43.75) | 9 (56.25) |
| Soft, no change to slight change | 6 (37.50) | 5 (31.25) | 6 (37.50) | 6 (37.50) | 6 (37.50) | 5 (31.25) |
| Firm, non-tender to beginning tenderness | 0 (0.00) | 0 (0.00) | 1 (6.25) | 0 (0.00) | 2 (12.50) | 0 (0.00) |
| Firm to very firm, tender to very tender | 0 (0.00) | 2 (12.50) | 2 (12.50) | 2 (12.50) | 1 (6.25) | 2 (12.50) |
| P-value | 0.55 | 0.7 | 0.88 | |||
| Breast pain | ||||||
| No pain | 15 (93.75) | 12 (75.00) | 7 (43.75) | 8 (50.00) | 8 (50.00) | 8 (50.00) |
| Slightly pain | 0 (0.00) | 2 (12.50) | 7 (43.75) | 5 (31.25) | 8 (50.00) | 6 (37.50) |
| Moderate pain | 1 (6.25) | 2 (12.50) | 2 (12.50) | 2 (12.50) | 0 (0.00) | 1 (6.25) |
| Severe pain | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (6.25) | 0 (0.00) | 1 (6.25) |
| P-value | 0.39 | 0.88 | 0.72 | |||
3.4. The Efficacy between 2 Groups in Terms of Breast Engorgement and Pain
The study showed that there was no significant difference in terms of breast engorgement and pain between the two groups. The results regarding these symptoms were classified into four severity levels. Most participants in both groups experienced engorgement and pain since day 2. However, on the last day of data collection, the control group had more participants reporting a breast engorgement score of 5 or 6 than the intervention group. Concerning the breast pain, it was found that the pain scale increased on the second day as well, and on the last recorded day, there were no moderate or severe pain symptoms in the experimental group in comparison to the control group, as shown in Table 3.
3.5. Mothers’ Expression
In the present study, apart from the aforementioned measurements, interviews were conducted with mothers who received MLD combined TTM and standard post-partum nursing care. The majority of participants expressed their views in three parts. Firstly, they did not perceive any physical or mental changes during the experiment. Secondly, after breast massages, they experienced a reduction in pain and engorgement, with only mild pain and engorgement occurring before lactation periods. Lastly, the mothers who received both MLD and TTM intervention expressed great satisfaction with the outcomes of this study during their lactation phase, as they felt alleviation of pain and engorgement and slightly increased breast milk volume by the second post-partum day. There was no mother’s complaint regarding severe side effects or the ineffectiveness of the MLD and TTM combination. All participants were pleased with the combination of these massage techniques.
4. DISCUSSION
This research aimed to investigate the safety and efficacy of MLD plus TTM along with standard post-partum nursing care in increasing breast milk volume and reducing engorgement and pain in mothers of premature infants after cesarean section. The demographic characteristics of the participants in both groups were similar at baseline. The primary outcome of the study was to compare the amount of breast milk, and the secondary outcome was to compare engorgement and pain in the experimental and control groups. The result showed that the group receiving MLD plus TTM had the same amount of breast milk production with safety, with no significant difference in the effectiveness of reducing engorgement and pain compared to the control group. One possible explanation for this result is that both groups received good standard nursing advice on expressing breast milk and did it regularly, as evidenced by the higher frequency of breast pumping than six times per day since day 2 in both groups. Therefore, both groups were able to produce enough breast milk. According to a review of the literature, frequent and effective milk removal is critical to maintaining and increasing milk production, especially for mothers of preterm [24, 25]. Moreover, the production and flow of breast milk in lactating mothers can be influenced by a variety of factors, including physical, psychological, and environmental factors. For example, stress can affect milk production in lactating mothers. Previous research has shown that mothers who experience high levels of stress produce less milk than those who are less stressed [26-28]. While this study was conducted on a sample of premature mothers whose infants were hospitalized in an intensive care unit, it may cause mothers to experience stress. Hence, it may be one of the reasons why some mothers produce less milk. This study's weakness was that it did not assess mothers' stress levels. Moreover, numerous additional factors affect the milk supply, like food, rest, or regular activities, etc. [29, 30].
As for engorgement and pain, this study investigated the prevention effect. The study found that this combination therapy did not have any significant impact on preventing breast engorgement or pain. However, the study suggests that MLD plus TTM may have a different effect when used as a treatment for mothers who already have breast engorgement or pain. Unfortunately, there are currently no studies on this topic. In contrast, some types of breast massage showed an effect on reducing engorgement and pain. For example, Therapeutic Breast Massage in Lactation (TBML) has been studied in breastfeeding women who presented with engorgement, plugged ducts, or mastitis. The study involved 42 participants and found that TBML resulted in clinically significant improvements in engorgement, pain, and plugged duct severity [31]. Another study found that Oketani breast massage was effective in alleviating breast pain as well [32], etc.
Although this research study did not show statistically significant differences between the experimental and control groups in terms of increased milk volume, decreased engorgement, and reduced pain, interviews with mothers participating in the study revealed that the group receiving MLD plus TTM massage experienced satisfaction with the outcomes of the experiment during their lactation period since the second day after giving birth, these results included less pain and more milk. There were no complaints from mothers regarding severe side effects or the ineffectiveness of MLD plus TTM, and all of them were pleased with the massages. This is consistent with previous research in which mothers who received various forms of breast massage were satisfied with the results, such as reduced breast pain and engorgement [31]. When considering the mechanism of breast massage in reducing these symptoms, it can be explained through the stimulation of lymphatic drainage. This process involves the activation of the lymphatic system, which is responsible for removing excess fluid and waste products from breast tissue. By promoting lymphatic drainage, breast massage can help reduce breast engorgement and pain [33]. Furthermore, breast massage also improves blood flow to the breast tissue, which can help to reduce inflammation and promote healing, thereby alleviating breast pain and engorgement [10, 15, 34]. Moreover, breast massage can help to relax the muscles in the chest and breast area, which can alleviate tension and pain. Whereas TTM focuses on circulation and pressure points, helping to relieve muscle tension and increase blood circulation [35]. These can be particularly helpful for mothers experiencing breast pain related to hormonal changes or stress [15, 36]. Potential limitations of this study included the lack of measurement of stress levels and controlling for daily routines, behavior, diet, or other factors that may affect breast milk volume and symptoms in pain and breast engorgement. Consequently, future studies would be beneficial to investigate the effects of MLD plus TTM on postpartum mothers experiencing pain and engorgement by controlling relevant factors and extending the study period. Additionally, the research should maintain a consistent frequency of milk expression for a more accurate assessment of breast milk volume.
CONCLUSION
The application of MLD with TTM, alongside standard post-partum nursing care, did not have significant differences in comparison to the provision of standard post-partum nursing care alone in terms of breast milk volume, breast engorgement, and pain. Nevertheless, participants in the experimental group expressed a high degree of satisfaction with the intervention involving MLD and TTM.
LIST OF ABBREVIATIONS
| MLD | = Manual Lymphatic Drainage |
| TTM | = Thai Traditional Massage |
| TMBL | = Therapeutic Breast Massage in Lactation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Approval for this study was obtained from the Ethics Committee of the Faculty of Medicine at Thammasat University (MTU-EC-SS-1-082/64, 138/2564). The trial was registered with the Thai Clinical Trials Registry (TCTR20230330002). In addition, each participant received a consent form in writing. The informed consent was explicit, stated the goal of the study, and explained the participant's right to withdraw from the study at any time. In addition, confidentiality and anonymity were maintained by issuing each participant a code number for analysis purposes only. There were no incentives or prizes for participants in the study.
HUMAN AND ANIMAL RIGHTS
No animals were used for this study. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants signed the written informed consent.
STANDARDS OF REPORTING
CONSORT guidelines were followed for the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Zenodo Repository at https://doi.org/10.5281/zenodo. 8365995.
FUNDING
This study received financial support from the Faculty of Medicine, Thammasat University, Thailand (Grant Number: TP.1-11/2564).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors extend sincere gratitude to all the participants who dedicated their time to this research project. Profound appreciation is also extended to all the staff members of Thammasat Hospital who were involved. Special thanks go Faculty of Medicine, Thammasat University for their crucial financial support.


