All published articles of this journal are available on ScienceDirect.
Trends in Risk Factors for Peripartum Depression in Socio-economically Disadvantaged Childbearing Community
Abstract
Introduction:
Perinatal depression is defined as a depressive episode(s) during the pregnancy and/or postpartum period up to one year. Studies have shown that childbearing people in urban settings experience a higher burden of social factors, such as low socioeconomic status, which may influence the likelihood of developing perinatal depression. Of note, episodes of perinatal depression have been shown to negatively impact child development. Our study has identified population trends in Center for Epidemiological Studies Depression Scale (CES-D) scores >10 during perinatal periods alongside significant social risk factors for people served by LSA Family Health Service providing skilled home-based nursing visits to reduce adverse outcomes.
Methods:
A retrospective chart review of nursing notes from 2009-2017 was conducted for this cross-sectional study. Outcome measures included antepartum (AP) and postpartum (PP) Center for Epidemiological Studies Depression Scale (CES-D) scores, with a score of > 10, suggesting a positive risk for developing depression. Data were grouped and analyzed using Microsoft Excel and SPSS software (SPSS version 23). Data have been presented as yearly population percentages scoring >10 on their CES-D screen.
Results:
The maternal outreach program (MOP) enrolled 1,183 birthing individuals from 2009-2017. The mean parental age was 27 years. 70% were Latinx (n=829) and 20.88% (n=247) were Black. Spanish was the primary language for 43.62% (n=516) of participants. Among CES-D screens completed in the antepartum period, 4.5% to 24.6% of the population met criteria over the 9-year study period for risk of developing depression. Positive CES-D screens completed postpartum ranging from 11.9% to 27.2% during the study period. Significant risk factors for positive postpartum CES-D screens were postpartum risk assessment score (p=0.03), increased gestational age (p=0.05), low income (p=0.03), teen/inexperienced parents (p=0.003), and low education levels (p=0.04).
Conclusion:
Trends of positive antepartum and postpartum depression screens in this population have fluctuated over the study period; however, we have identified significant risk factors for positive postpartum screens. Screening for postpartum depression risk factors is important to identify birthing parents who may most benefit from mental health interventions.
1. INTRODUCTION
Perinatal depression is defined by the DSM V as experiencing at least a two-week depressive episode with onset during pregnancy or up to one year postpartum [1]. A 2016 report estimates that peripartum depression affects about 14% of the U.S. population, with increasing prevalence worldwide in low-income and middle-income countries compared to high-income countries [2]. The prevalence of peripartum depression increases significantly if a childbearing individual has a past medical history of a mood disorder (50%) and/or a past family history of postpartum psychosis (70%) [3]. Research indicates that perinatal depression is not yet well detected or managed [4]. Studies have also shown that urban women experience a higher burden of social factors, such as low socioeconomic status, which may influence the likelihood of developing perinatal depression [5, 6]. In this paper, we have utilized the definition of social determinants that acknowledge an individual’s environment, such as financial resources or life events, etc., that can influence their likelihood of developing a condition or illness. In conjunction with social risk factors, episodes of perinatal depression are increasingly recognized over the years as a potential driver of poor health and developmental outcomes for both the gestational parent and child. Given the documented negative effects, screening for perinatal depression can serve as a tangible way to identify those at risk and initiate prevention and/or intervention. Without timely screening, studies have shown longer duration of perinatal depressive episodes [7, 8]. Individuals may have more frequent contact with the healthcare system during their pregnancy, highlighting the utility of screening during this time [9].
Our study features the nursing sector of LSA Family Health Service (LSA) located in an underserved neighborhood in East Harlem, New York. Their mission is dedicated to closing the health inequities that plague low-income and under-resourced communities. As a certified home health agency, the nursing arm of this nonprofit agency has the capacity to assess and follow up on groups, like high-risk maternity patients, who may most benefit from preventive measures. They do this with public health nurses who perform in-home assessments of both medical and social characteristics. They also run other supportive programs, including breastfeeding and parenting workshops, designed to mitigate important social risk factors. With this unique scope, we felt it important to document the impact of this program.
This cross-sectional study utilized an urban, multiethnic population with a variety of social risk factors. We have demonstrated a trend of positive (score of > 10) antepartum and postpartum CES-D screening scores from 2009-2017 from a community-based maternal outreach program. We have also reported the number of participants who have screened positive for selected psychosocial risk factors. This study is unique due to its 9-year frame and aims to highlight an association between social risk factors and elevated CES-D scores in an urban under-resourced community. This study will also serve to quantify the impact of the community organization to advocate for program expansion.
2. METHODS
2.1. Study Setting
Data were sourced from the maternal outreach program (MOP) of LSA, a non-profit community nursing organization located in East Harlem, New York. The 2018 New York City (NYC) community health profile describes East Harlem as a population composed mostly of adults aged 25-64 years [10], with more than three-quarters of the population identifying as either Latinx (50%) or Black (30%). Also, of note is that the East Harlem community shoulders an increased burden of poverty, unemployment, and adults without access to health care compared to the general NYC population [10]. The MOP of the chosen non-profit organization provides social and home health services to this low-income/high-risk population.
2.1. Study Population
Our study population consisted of pregnant and postpartum child-bearing individuals referred to the MOP between 2009 and 2017. Referrals were either self-referrals or from local obstetric clinics and hospitals [11]. All individuals of the MOP with singleton pregnancies during the study time frame were eligible for inclusion in the study. Multiple births were excluded from analysis due to unavailable data for most of the study time frame.
2.3. Study Design and Analysis
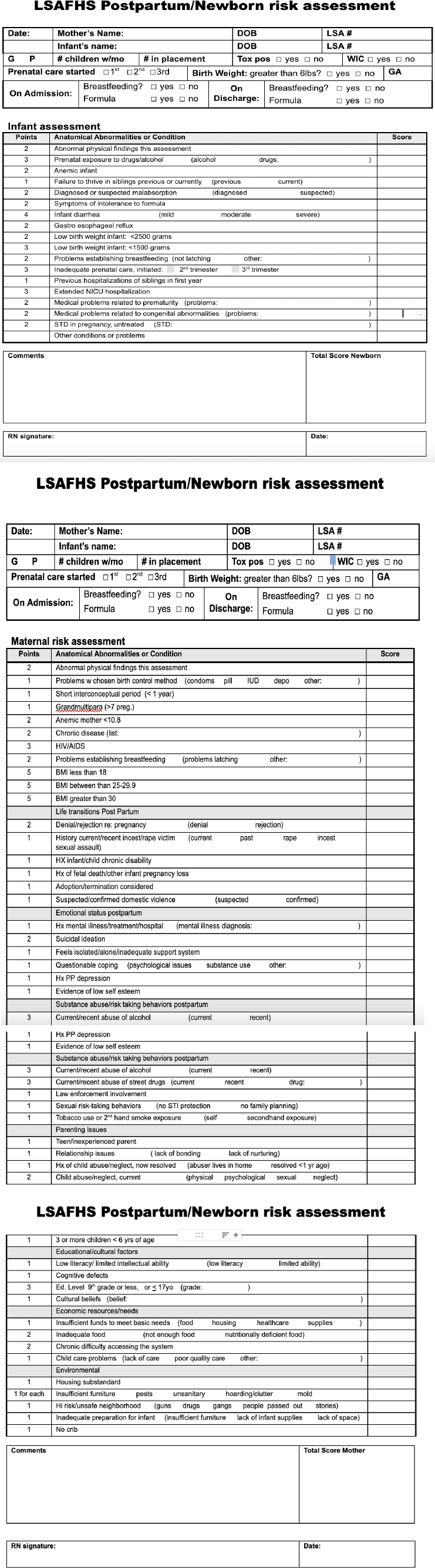
A retrospective paper chart review on MOP data from 2009-2017 of enrolled participants was conducted by trained research assistants. Prior to the chart review, LSA nurses collected various data points as part of their routine intake and follow-up process. Of particular interest were antepartum (AP) and postpartum (PP) Center for Epidemiological Studies Depression Scale (CES-D) scores, with a score of 10 or greater flagged as concerning for a future depressive episode. The CES-D has been proven as a reliable screening tool in a low-income perinatal population [12]. Also collected were social risk factors, identified with the MOP’s own screening forms, attached in the appendix. Risk factors of interest included insufficient income, substandard housing, unsafe neighborhood, less than high school education, teen/first-time parent, preeclampsia, gestational diabetes, and PP risk assessment score in our study participants. Appendix A includes the intake form with definitions of the risk factors used by LSA nurses.
Data were grouped according to risk factors collected from intake forms and analyzed with SPSS software (SPSS version 23). Data have been presented as yearly population percentages who scored >10 on their CES-D screen. Individuals with collected risk factors of interest and CES-D scores of 10 or greater were identified. Additionally, logistic regression was used to model potential associations between social risk factors identified during initial program intake and CES-D scores.
| Characteristic | Participants (n) | Participants (%) | SD |
|---|---|---|---|
| Mean maternal BMI | 27.72 | -- | 7.174 |
| Mean maternal age at delivery | 27.05 | -- | 6.43 |
| - | - | - | - |
| Race/Ethnicity | - | - | - |
| African-American/Black | 247 | 20.88% | - |
| Latinx | 829 | 70.08% | - |
| Other | 13 | 1.10% | - |
| Missing | 94 | 7.95% | - |
| - | 100.00% | - | |
| - | - | - | - |
| Primary language spoken | - | - | - |
| English | 412 | 34.83% | - |
| Spanish | 516 | 43.62% | - |
| Both | 222 | 18.77% | - |
| Other (i.e., Creole) | 16 | 1.35% | - |
| Missing | 17 | 1.44% | - |
| - | 100.00% | - | |
| - | - | - | - |
| Risk factor | - | - | - |
| Insufficient income | 546 | 46.15% | - |
| Teen/inexperienced parent | 475 | 40.15% | - |
| Substandard housing | 410 | 34.66% | - |
| Inadequate food | 374 | 31.61% | - |
| Less than high school Education | 398 | 33.64% | - |
| High risk/unsafe neighborhood | 304 | 25.70% | - |
| AP elevated CES-D | 50 | 4.23% | - |
| PP elevated CES-D | 229 | 19.36% | - |
3. RESULTS
Population characteristics are demonstrated in Table 1, and Table 1,183 charts met inclusion criteria and were included for analysis. Most of the MOP participants were identified as Latinx (70.08%, n=829), classified as overweight (mean BMI= 27.72), and almost half of them spoke Spanish as their primary language (43.62%, n=516).
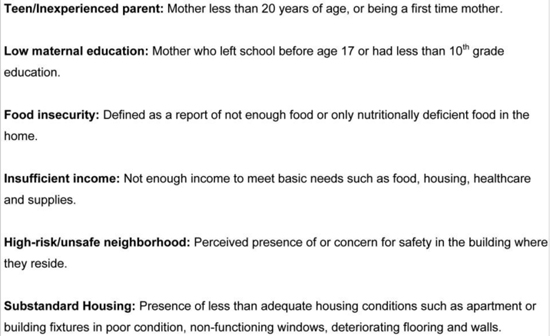
Participants frequently identified with more than one risk factor and risk factor definitions are featured in Fig. (1). Almost half of the participants reported having insufficient income (46.15%, n=546) per intake screening questions and were classified as either a teen or first-time (inexperienced) parent (40.15%, n=475). The next most prevalent risk factors overall were living in substandard housing (34.64%, n=410) and having less than a high school education (33.64%, n=398). One quarter (25.70%, n=304) of the participants were flagged as living in an unsafe neighborhood. The postpartum CES-D screening group comprised 671 people and 34.13% (n=229) had an elevated postpartum CES-D screen. The antepartum group during the study period consisted of 66 people and 4.23% (n=50) were documented with an elevated antepartum CES-D score.
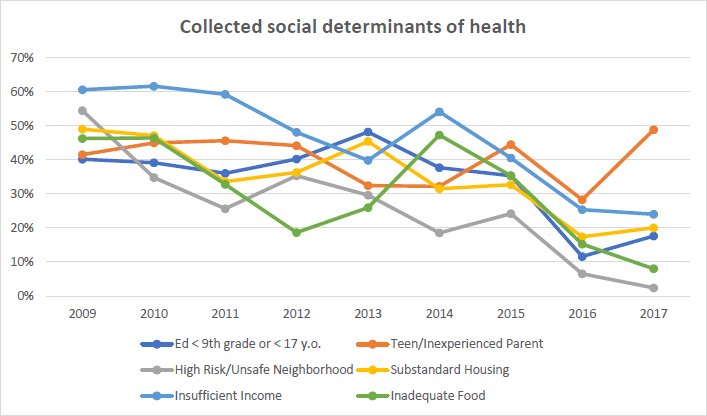
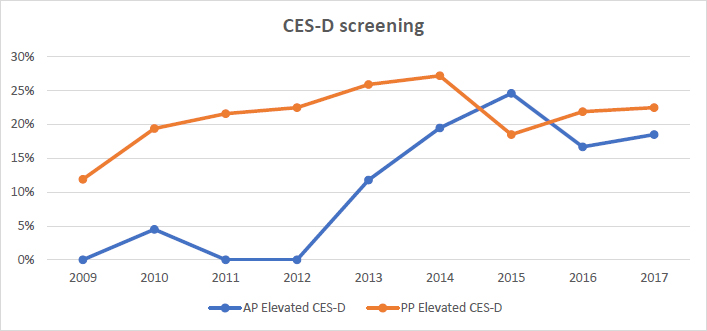
Fig. (2) outlines risk factor trends by year. The category of less than high school education exhibited a notable percentage drop from 2015 to 2016 from 37.50% to 13.00%. The year 2017 revealed the highest percentage of those classified as teen/inexperienced parents at LSA at 54.50%. Fig. (3) reveals the prevalence of positive antepartum screens, which ranged from 4.5% to 24.6% over the study period. Data were missing for AP CES-D screens for the years 2009, 2011, and 2012. Prevalence of positive postpartum CES-D screening ranged from 11.9% to 27.2% over the study period. The years 2015 and 2014 saw peak prevalence for positive antepartum and postpartum CES-D screens, respectively, at 24.60% and 27.20%.
The following categories declined over the nine-year study period: high-risk/unsafe neighborhood, substandard housing, insufficient income, and inadequate food. The prevalence of “high-risk/unsafe neighborhood” ranged from its peak in 2009 at 54.40% to its trough in 2017 at 2.70%. Substandard housing saw a notable decline between 2015 and 2016 from 34.70% to 19.50%. The insufficient income category experienced two notable declines between 2011 and 2013 from 59.20% to 39.80% and again between 2014 and 2016 from 54.10% to 28.50%. The “inadequate food” category also experienced two declines between 2010 and 2012 from 46.40% to 18.60% and again between 2014 and 2017 from 47.30% to 8.90%.
Table 2 features logistic regression data attempting to identify risk factors associated with elevated CES-D scores. Factors significantly associated with an elevated CES-D screen were postpartum risk assessment score (p=0.03), gestational age (p 0.05), low income (p 0.03), teen/inexperienced parents (p=0.003), and low education levels (p 0.04).
| Factors | Odds Ratio | Lower Confidence Limit | Higher Confidence Limit | p-value |
|---|---|---|---|---|
| BMI | 1.001 | 0.966 | 1.038 | 0.36 |
| Pre-eclampsia | 1.053 | 0.493 | 2.248 | 0.95 |
| Gestational DM | 2.424 | 1.109 | 5.3 | 0.89 |
| PP risk assessment score | 1.093 | 0.999 | 1.195 | 0.03* |
| Gestational age | 1.041 | 0.849 | 1.276 | 0.05 |
| Food insecurity | 1.746 | 0.898 | 3.395 | 0.10 |
| Low income | 0.489 | 0.258 | 0.926 | 0.03* |
| Inexperienced | 0.449 | 0.265 | 0.761 | 0.003* |
| Housing insecurity | 1.18 | 0.712 | 1.957 | 0.52 |
| Low education levels | 0.542 | 0.305 | 0.963 | 0.04* |
4. DISCUSSION
Our study highlights the nine years’ trends of social risk factors assessed in LSA’s MOP population. Trends have revealed a general decrease throughout almost all categories, with greater fluctuance in the latter study years. Of note, the teen/inexperienced parent and substandard housing categories appeared to vary the least. Embedded within the East Harlem community, LSA’s MOP population experienced greater rates of poverty and lower housing quality than fellow community members and NYC overall during a similar time period [10].
This study has also identified the following social factors as associated with elevated postpartum CES-D scores: low income, teen/inexperienced parenting, and low education. This is comparable to another study that found ethnicity, education, and social support predictive of elevated CES-D scores in a similar population [13]. When compared to the general East Harlem population, the MOP reported greater rates for several significant factors, including insufficient income, substandard housing, and inadequate food (2018). The trend for elevated postpartum CES-D score did not increase past 27% during the study period, which has been slightly lower than the 32.4% reported in another similar population [14]. The inexperienced risk factor did not improve over time, corroborating similar findings in another study on depressive symptoms that found younger and more socially isolated women scoring > 16 on CES-D screening [15]. Other studies have corroborated a positive association between positive CES-D screening and subsequent development of depression, particularly in disadvantaged populations [16, 17].
Perinatal depression impacts anywhere from 10 to 20% of pregnancies in the United States [18]. Undiagnosed perinatal depression can compromise parent-child attachment as well as negatively impact physical, cognitive, and behavioral development in children [19]. Untreated peripartum depression has also been associated with significant morbidity during the neonatal period, which includes attachment disorder, developmental delay, and failure to thrive [20]. Peripartum depression is also considered one of the leading precipitators of maternal mortality due to suicide [3]. The snowball effect of social risk factors influencing depression screening and the negative long-term ramifications of undiagnosed/untreated perinatal depression highlights the continued need for MOPs and depressive symptom screening in low-income populations.
The U.S. Preventive Services Task Force has recommended grade B to screen pregnant and postpartum women for depression to enhance identification, referral, and counseling treatment [21]. Home-visiting programs, especially those with public health nurses, are a great avenue to readily screen for perinatal depressive symptoms and are uniquely positioned to provide long-term follow-up and promote continuity of care through a direct point of contact. A successful example of this would be the Nurse-Family Partnership (NFP), an evidence-based community health program shown to be “a targeted public health intervention program designed to improve child and maternal health through nurse home visiting” [22, 23]. Randomized trials of the NFP in certain states have shown improvement in the following areas: health during pregnancy, the total number of pregnancies, the interval between pregnancies, maternal employment, and welfare use [23]. Another randomized control trial demonstrated the NFP program model to be a cost-effective investment in addressing social determinants of health [24]. It is estimated that by 2031, the NFP will have mitigated key risk factors, including closely spaced second births, infant death, premature birth, intimate partner violence, high school completion, employment, and pregnancy complications, which will ultimately reduce Medicaid and Supplemental Nutrition Assistance Program spending [25-27].
LSA classifies as a local/community-based nurse-family partnership. Our study has highlighted this community’s struggle with social risk factors and their relationship to perinatal depression development. Additionally, LSA’s MOP provides the advantage of being embedded in their neighborhood and is therefore more likely to be accepted by community members. These characteristics ensure that LSA has an appropriate foundation to contribute to accomplishing the USPSTF’s recommendation. Programs, like LSA’s maternal outreach program, show great value in identifying significant risk factors associated with postpartum depression and providing interventions to parents most in need. Our findings also show the importance of expanding referral capacity to improve access to perinatal depression screening, particularly for vulnerable populations. With cultural humility acknowledged, we could hope to see the same long-term benefits in our high-risk population and others like it.
5. LIMITATIONS
The MOP receives a combination of self- and medical referrals, which may have led to a selection bias. Internal validity/observer bias may also be a limitation of the study, as intake forms were completed by multiple nursing staff at the MOP. Gaps in data are another limitation of this study as our reporting has been based on the data abstracted and, as shown in the results, several data points have been inconsistently collected. The database was not created with the intention of research, therefore limiting consistency. Other variables, such as genetic predisposition, biomarkers, and environmental factors have also been shown to be associated with postpartum depression, which has not been addressed in this study. Since these data points were not collected by the staff at the MOP, discussion of these factors is beyond the scope of our paper. However, these factors should be investigated in future studies.
CONCLUSION
This paper has documented fluctuating population trends in perinatal CES-D scores > 10 along with significant social risk factors over a nine-year period in an urban high-risk perinatal population serviced by a non-profit organization providing nursing home visits through their maternal outreach program. Our findings highlight the importance of funding trusted community-based organizations, such as LSA, in neighborhoods with significant social health needs. Early identification, evaluation, and eventual management of perinatal depressive symptoms are essential to help vulnerable families.
LIST OF ABBREVIATIONS
| AP | = Antepartum |
| PP | = Postpartum |
| CES-D | = Center for Epidemiological Studies Depression Scale |
| MOP | = Maternal Outreach Program |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The institutional review board (IRB) at Icahn School of Medicine at Mount Sinai, New York, NY, USA, deemed this study exempt from IRB approval and exempt from an informed consent as it was a retrospective chart review utilizing only de-identified data.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The IRB provided us a waiver declaring exemption from informed consent due to the data being de-identified.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is solely housed within the institution’s archive and not currently accessible through an online data repository.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank LSA Family Health Service for their willingness to participate. This paper is in memory of Sister Susanne Lachapelle who spearheaded LSA’s community-based outreach efforts.
APPENDIX A: LSA INTAKE FORM