All published articles of this journal are available on ScienceDirect.
Epidemiological Patterns of Hypertension and Type 2 Diabetes Mellitus in the Socialist Republic of Vietnam: an Ecological Study
Abstract
Background:
Hypertension and type 2 diabetes mellitus belong to the most costly chronic diseases worldwide. The Socialist Republic of Vietnam is a country with a high burden of communicable and non-communicable diseases, with hypertension and diabetes among the top contributors to premature mortality.
Objective:
The aim of the study was to describe and assess the scale of the burden of hypertension and type 2 diabetes mellitus in the Socialist Republic of Vietnam.
Methods:
An ecological study employing secondary data analysis was conducted. Data from the Institute of Health Metrics and Evaluation and Vietnamese Health Statistic Yearbooks were analysed by linear and polynomial regression analyses, Kendall rank correlation, and Pearson correlation.
Results:
From 1990 to 2017, on average, 22% of all deaths and 11% of all disability-adjusted life years were associated with high systolic blood pressure, and 3% of all deaths and 2% of all disability-adjusted life years were attributable to type 2 diabetes mellitus in the Socialist Republic of Vietnam. The decrease in the number of elementary nurses, as well as the increase in health insurance expenditures per inpatient, seems to be, with the highest degree of certainty, correlated with type 2 diabetes mellitus death and disability-adjusted life years rates.
Conclusion:
If the tracked progress remains at the same pace, the Socialist Republic of Vietnam will likely be unable to achieve the targets related to Goal 3 of the United Nations 2030 Agenda for Sustainable Development. Developing regulatory frameworks and social demand for professionalism could encourage nurses to pursue higher education.
1. INTRODUCTION
Non-communicable diseases (NCDs) have become the leading cause of the global burden of disease, accounting for two-thirds of mortality worldwide. Cardiovascular diseases (CVDs) are responsible for the largest proportion of this burden, contributing to one-half of the NCDs deaths, three-quarters of which occurred in low- and middle-income countries [1]. Hypertension (HT) is one of the most significant risk factors for CVDs, which were the leading cause of premature deaths globally [2, 3]. There is a strong association between type 2 diabetes mellitus (DM) and CVDs, which are the most prevalent cause of morbidity and mortality among patients with DM [3, 4]. The incidences of HT and DM continue to rise, with these two diseases among the most prevalent and costly chronic diseases worldwide [3, 5]. The prevalence of HT and type 2 DM among adults in low- and middle-income countries are similar to or higher than in high-income countries because of a sharp increase in prevalence over the past few decades [6, 7].
In 2008, there were an estimated 14.5 million total deaths in Southeast Asia (SEA), with 55% attributable to NCDs. CVDs alone accounted for 25% of all deaths, and HT is responsible for nearly 1.5 million of those deaths annually [8]. The prevalence of diabetes is also growing at an alarming rate and has almost doubled in many SEA countries between 2005 and 2015 [9]. The Socialist Republic of Vietnam (SR Vietnam) is a SEA country with a high burden of NCDs and CVDs, with HT and diabetes among the top contributors to premature mortality [10].
In the context of high NCD-associated burdens in the SEA region, SEA countries have endorsed several policy frameworks and national programs, such as the South-East Asia Regional Network for Prevention and Control of Noncommunicable Diseases in 2005 and the Action plan for the prevention and control of NCDs in SEA in 2013 [11]. One of these endorsements is the project Scaling-up NCD Interventions in South-East Asia (SUNI-SEA), which is currently ongoing in three SEA countries (Indonesia, Myanmar and SR Vietnam). The project aims to validate effective scaling-up strategies for evidence-based DM and HT prevention and management programs [12]. This study was part of the project implementation for SUNI-SEA with the aim to create a basis for the research hypothesis for the SUNI-SEA project in SR Vietnam. For this purpose, we described and assessed the scale of the burden of CVDs, HT, and type 2 DM and attached financial and contextual factors affecting its progress.
2. MATERIALS AND METHODS
2.1. Study Design and Data Sources
To investigate the epidemiological burden of HT and type 2 DM in SR Vietnam, we conducted an ecological study employing secondary data analysis. Data from the Institute of Health Metrics and Evaluation were accessed using the Global Burden Disease (GBD) Results Tool [13]. In the database, ICD-10 coding was used. Although the wide range of the confidence intervals limits the validity of this data, it belongs to the most appropriate among accessible, up-to-date data sources. Data were age-standardized using the GBD reference population by researchers in the Global Burden of Disease Study in 2019 [14].
The data from the Vietnamese Health Statistics Yearbooks (VHSY) published by the Vietnamese Ministry of Health [15] were analysed for financial and contextual factors (human resources, health insurance, health expenditures, etc.). The Yearbooks published between 2009 and 2016 were selected (8 yearbooks in total) [16-19]. Because of changes in reports, resulting in missing or incomplete data, we excluded any Yearbooks before 2009.
2.2. Variable Definitions and Statistical Analysis
To analyse the epidemiological situation of CVDs and type 2 DM, we used the variables Cardiovascular diseases (code B.2) and Type 2 diabetes mellitus (code B.8.1.2) coded under the “Causes” category in the GBD Results Tool. The burden of HT was assessed by the variable High systolic blood pressure (SBP) (SBP≥ 110-115 mmHg) coded under “Risk factors” from the “All causes” category.
Four financial and contextual factors were selected from VHSY. In the category of “Health personnel”, 23 professions were identified, and to promote clarity of the study’s results, some were clustered (college and university nurses with second-degree to higher degree nurse) or excluded based on their relevance to the aims of the study (pharmacists, midwives, etc.).
All data obtained were sorted out in Microsoft Excel. The proportion of deaths and DALYs attributable to CVDs, High SBP, and type 2 DM were calculated as a percentage of all deaths in SR Vietnam from 1990 till 2016. The age-standardized death rates and disability-adjusted life years (DALYs) of CVDs, high SBP, and type 2 DM were analysed by linear and polynomial regression analyses to assess their changes over time. The fit of each regression was assessed by the coefficient of determination R2, i.e., if R2 =0 then the model does not predict the outcome, if R2 is between 0-1 then the model partially predicts the outcome, if R2 =1 then the model perfectly predicts the outcome. To assess the type of data distribution, Kolmogorov-Smirnov Test was used. Due to the continuous data format and normal distribution of the data, the Pearson correlation coefficient was used to estimate the correlation between selected financial and contextual variables and age-standardized death rates and DALYs of CVDs, high SBP, and type 2 DM. To signify the amount by which the selected variables changed in time, the regression coefficient was calculated. The statistical analysis was performed in the R project software [20].
3. RESULTS
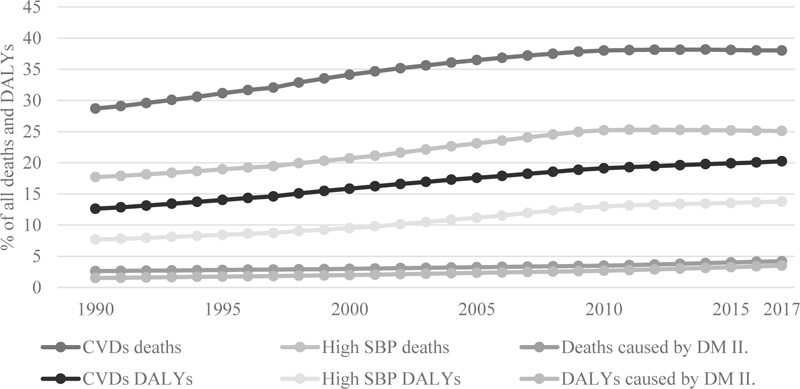
Deaths caused by CVDs represented approximately 35% of all deaths in SR Vietnam from 1990 to 2017, of which 58% were attributable to high SBP. Similarly, out of 15% of all DALYs which were attributable to CVDs, 59% were caused by high SBP. On average, 22% of all deaths and 11% of all DALYs were associated with high SBP, and 3% of all deaths and 2% of all DALYs were attributable to type 2 DM between 1990 and 2017 in SR Vietnam (Fig. 1).
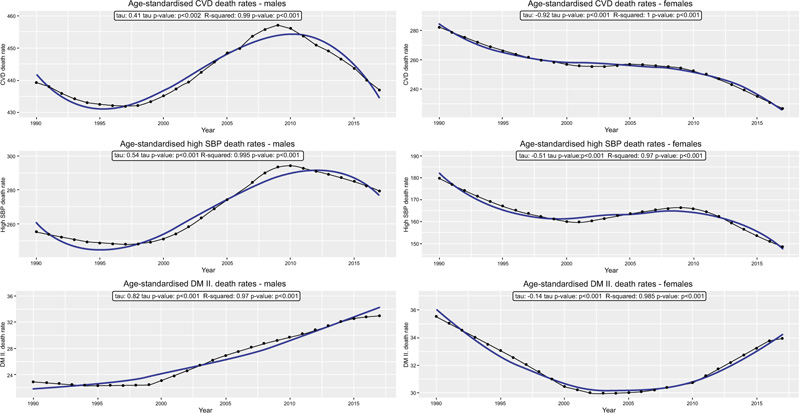
Between 1990 and 2017, the CVD death rate among males declined for several years until the late 1990s and then increased to a peak in 2009 followed by a sharp fall. During the observed time, there was also a significant increase in mortality, in high SBP and type 2 DM death rates respectively, with the highest increase in type 2 DM death rate. On the contrary, a significant decrease in CVD death rates was observed for females. High SBP death rates among females decreased till 1995 and then flattened, starting to decrease again in 2011. Age-standardised type 2 DM death rates among females tended to decrease over time from 1990 to 2002 but in 2006 began to increase again, which was very different from the pattern of type 2 DM death rates among men (Fig. 2).
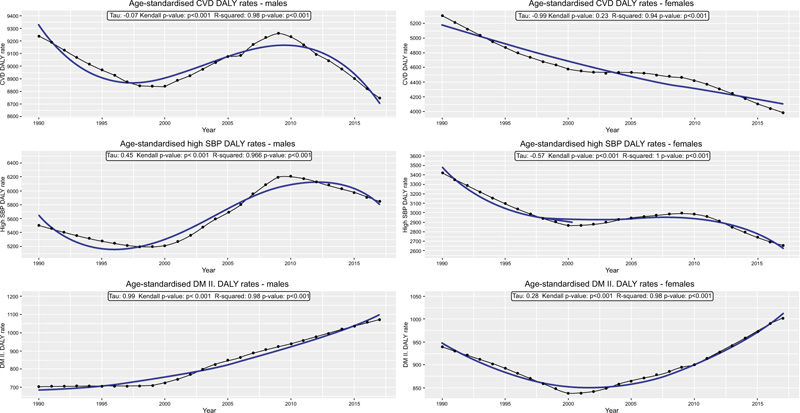
From 1990 to 2016 the CVDs DALYs rate decreased significantly for females but not for males. Among females this decrease was more stable until 2002, followed by a small increase during 2004-2005 and then continued to decrease, thus again showing a different pattern than in men. High SBP DALYs rate similarly decreased over time significantly for females but increased significantly for males. Among men, we observed an actual decline in the high SBP DALYs rate until 2000, but since 2001 DALYs rate began to increase rapidly till 2010 followed by the next decline until 2016. An increase in type 2 DM DALYs rate was significant for both males and females. Even though till the late 1990s the DALYs rate was stable among men and even declining among women, it began to increase substantially since 2000 among both sexes (Fig. 3).
Between 2009 and 2016, health personnel capacities in SR Vietnam have significantly increased, mainly in the categories of Bachelor of Public Health (or higher) and among nurses with higher degrees. As many nurses pursued higher education levels, there was a significant increase in the number of citizens that pertain to 1 elementary nurse (EN). Over the years, this increase has also been observed for assistant doctors and traditional medicine practitioners (Table 1).
The number of health consultations that citizens attended per year did not change significantly from 2013 to 2016. Between these years in SR Vietnam, there has been a substantial increase in expenditures per inpatient from health insurance, but not in expenditures per outpatient (Table 2).
| Year | AD | BoPH | EN | HDN | MD | MT | TMP |
|---|---|---|---|---|---|---|---|
| 2009 | 1 685 | 186 604 | 10 422 | 1272 | 1 518 | 6 211 | 319 794 |
| 2010 | 1 657 | 133 735 | 12 173 | 1173 | 1 390 | 6 113 | 329 272 |
| 2011 | 1 612 | 94 962 | 14 113 | 1074 | 1 364 | 5 785 | 401 096 |
| 2012 | 1 627 | 83 355 | 15 372 | 1027 | 1 363 | 5 650 | 374 569 |
| 2013 | 1 602 | 59 410 | 16 803 | 982 | 1 310 | 5 264 | 391 742 |
| 2014 | 1 618 | 52 354 | 19 866 | 931 | 1 289 | 5 321 | 405 040 |
| 2015 | 1 684 | 52 830 | 23 160 | 929 | 1 247 | 5 048 | 465 550 |
| 2016 | 1 731 | 41 234 | 26 993 | 898 | 1 169 | 4 965 | 441 405 |
| r2 | 0.1 | 0.9 | 1.0 | 0.9 | 0.9 | 1.0 | 0.8 |
| b | 5.3 | -18 737 | 2257.4 | -51.4 | -40.9 | -188.4 | 18 591 |
| CI 95% | -12.3; 22.9 | -26673; -10799 | 1807; 2707 | -66.5; -36.2 | -52.7; -29.1 | -225; -152 | 10104; 27078 |
| p-value | 0.5 | <0.01 | <0.001 | <0.001 | <0.001 | <0.001 | <0.01 |
| Year |
Average Consultations Per Capita |
Health Expenditure Per Inpatient | Health Expenditure Per Outpatient |
|---|---|---|---|
| 2013 | 2.4 | 85 | 10 |
| 2014 | 2.2 | 97 | 7 |
| 2015 | 2.3 | 106 | 7 |
| 2016 | 2.5 | 121 | 9 |
| r2 | 0.2 | 1.0 | 0.1 |
| b | 0.04 | 12.0 | -0.3 |
| CI 95% | -0.2; 0.3 | 8.8; 15 | -3.9; 3.3 |
| p value | 0.6 | <0.01 | 0.8 |
| CVDs Death Rate | High SBP Death Rate | DM type 2 Death Rate | ||||
|---|---|---|---|---|---|---|
| Variable | r | CI 95% | r | CI 95% | r | CI 95% |
| BoPH | 0.9 | 0.5; 1.0 | 0.9 | 0.4; 1.0 | -0.9 | -1.0; -0.6 |
| EN | -1.0 | -1.0; -0.9 | -1.0 | -1.0; -0.9 | 1.0 | 0.9; 1.0 |
| HDN | 0.9 | 0.6; 1.0 | 0.9 | 0.6; 1.0 | -1.0 | -1.0; -0.8 |
| HIEpI | -1.0 | -1.0; -0.9 | -1.0 | -1.0; -0.9 | 1.0 | 0.9; 1.0 |
| MD | 1.0 | 0.9; 1.0 | 1.0 | 0.9; 1.0 | -1.0 | -1.0; -0.7 |
| MT | 1.0 | 0.7; 1.0 | 1.0 | 0.7; 1.0 | -1.0 | -1.0; -0.8 |
| TMP | -0.9 | -1.0; -0.3 | -0.9 | -1.0; -0.3 | 0.9 | 0.3; 1.0 |
| CVDs DALYs Rate | High SBP DALYs Rate | DM type 2 DALYs Rate | ||||
| Variable | r | CI 95% | r | CI 95% | r | CI 95% |
| BoPH | 0.9 | 0.5; 1.0 | 0.9 | 0.5; 1.0 | -0.9 | -1.0; -0.6 |
| EN | -1.0 | -1.0; -0.9 | -1.0 | -1.0; -0.9 | 1.0 | 0.9; 1.0 |
| HDN | 0.9 | 0.7; 1.0 | 0.9 | 0.6; 1.0 | -1.0 | -1.0; -0.7 |
| HIEpI | -1.0 | -1.0; -0.9 | -1.0 | -1.0; -0.9 | 1.0 | 0.9; 1.0 |
| MD | 1.0 | 0.8; 1.0 | 1.0 | 0.8; 1.0 | -1.0 | -1.0; -0.8 |
| MT | 1.0 | 0.8; 1.0 | 1.0 | 0.7; 1.0 | -1.0 | -1.0; -0.8 |
| TMP | -0.9 | -1.0; -0.3 | -0.9 | -1.0; -0.3 | 0.9 | 0.3; 1.0 |
From the results of the correlation analysis, the contextual variables Number of citizens per 1 EN and Health insurance expenditures per inpatient, were identified with the relatively narrowest confidence intervals (width ≤0.15). These contextual variables were strongly associated with all six main variables – negatively with CVDs and high SBP, and positively with type 2 DM in terms of death rates and DALY rates. For all other contextual variables, the 95% confidence intervals in the correlation analysis were wider. The variables of Citizens per 1 assistant doctor, Average number of medical consultations per capita, and Health insurance expenditures per outpatient all had strong correlations with CVDs, high SBP, type 2 DM death, and DALY rates (positively or negatively). However, they had extremely wide confidence intervals and p values greater than 0.05, thus were excluded as nonsignificant (Table 3).
4. DISCUSSION
The health burden of many NCDs in SR Vietnam has increased since the 1990s, with an attributable mortality rate from NCDs at nearly 78% for all deaths in 2015. A similar situation affects the whole SEA region, ranging from 45% of NCD-related deaths in Timor-Leste to 85% in Brunei Darussalam in 2016 [21]. The proportion of DALYs attributable to NCDs and mortalities from NCDs in SR Vietnam since the 1990s are progressing at the same rate as estimated proportions of NCDs DALYs and deaths for countries with middle socio-demographic indices [22]. However, if the tracked progress remains at the same pace, SR Vietnam will likely be unable to achieve the targets related to Goal 3 “Good health and well-being“ of the UN 2030 Agenda for Sustainable Development [23].
SR Vietnam has made significant progress in its health workforce development over the last decade. Although it still did not meet the World Health Organization (WHO) standard of 1 medical doctor (MD) per 1000 patients [24], this ratio increased from 0.66 in 2009 (1518 citizens per 1 MD) to 0.86 in 2016 (1169 citizens per 1 MD). Similar progress has been partially made in the nursing profession, in which nurses have started to achieve higher levels of education. This progress could be a possible contributor to the decrease in the total number of ENs in SR Vietnam. With economic growth, the establishment of the Joint Coordinating Committee on Nursing in 2007, continuous development of regulatory frameworks, and increased social demand for quality care and professionalism in SR Vietnam, nurses may feel more empowered and supported to pursue higher education [25].
In our analysis, the decrease of ENs was strongly correlated with a decrease in CVDs and high SBP death and DALY rates, but also with an increase in type 2 DM death and DALY rates. It is important to mention that correlation is not the same as the causation and the decrease in the number of EN over time does not necessarily explain the decrease in CVDs and high SBP death and DALY rates or the increase in type 2 DM death and DALY rates. Other factors may have influenced and contributed greatly to these decreased or increased rates but were not included in the analysis (for example because of the availability of data) or were beyond scope of our ecological study (previous interventions, policy changes). However, regarding skilled health workers (SHW) and the WHO standard to achieve 80% coverage of essential health services, SR Vietnam lacks more nurses than medical doctors. The nurse-to-patient ratio in SR Vietnam was 1.45 per 1000 patients in 2016, while the WHO standard is to have at least 4 nursing personnel per 1000 patients [26]. This also corresponds with the number of medical consultations (MCs) per capita in SR Vietnam, which is much lower than the OECD average of 6.9 MCs per person per year. The variations in MCs per person annually between countries in the SEA region may be due to the differences in the economic development of these countries or the number of their SHWs, e.g., Cambodia in 2015 had 0.6 MCs per capita, Singapore in 2013 had 1.7, and Brunei Darussalam in 2008 had 3.9 [27].
Health insurance expenditures per inpatient (HIEpI) in SR Vietnam have significantly increased within the past few years and will need to be handled in the future. Our findings can be understood as the utilization of inpatient services is likely linked with serious NCD-associated conditions and complications. Health financing reforms that shift resources from hospital care to primary care should be developed to improve access to early diagnosis and chronic care and thus mitigate serious NCD-related complications and their associated economic burden of health expenditures on the population.
The CVDs, high SBP, type 2 DM death rates, and DALY rates since the 1990s in SR Vietnam have become more differentiated between males and females as we move closer to the present. Although males have significantly higher rates attributable to CVDs, high SBP, and since 2007 DALY rates related to type 2 DM, in the female population the type 2 DM death rate is higher. Even though it has been recognized in the past that the impact of type 2 DM is greater in females than in males, it is not yet fully understood. Possible explanations could be correlated to different cardiovascular risk profiles or differences in the quality of health care provided, but this would need to be further examined [28].
With the estimated burden attributable to CVDs, policymakers will have a fundamental role in tackling their impact in SR Vietnam. The economic utility in the implementation of preventive measures to reduce the health burden of both HT and type 2 DM has been demonstrated in the past [29]. Consequently, the Vietnamese government has nationally implemented the One Strategic Plan to reduce four main NCDs by 10% between 2017 and 2021 [30]. Similarly, since 2016, 11 SEA countries have endorsed national multisectoral NCD action plans to implement the Colombo Declaration on NCDs, which seems to have helped accelerate the necessary progress [31]. To achieve the SDG target of 3.4 by 2030, decision-makers in SR Vietnam, as well as in other Asian countries, will have to endorse networked governance with strong political leadership oriented towards capacity building in health and primary health care as keystones in reducing the burden of NCDs [32].
However, there are some limitations to this study that we would like to acknowledge. The ecological character of this study limited our inference possibilities about the individuals; thus, conclusions must be taken with caution and should serve as a basis for further analysis. The study was also limited by the availability of historical data on health personnel in SR Vietnam, as the presence and analysis of older data could reveal further differences.
CONCLUSION
The burden of HT and type 2 DM has risen significantly since the 1990s in SR Vietnam, and this growth will likely continue if the government will not endorse effective precautions. Although the health workforce has increased significantly over the years, SR Vietnam still has not achieved WHO standards, and HT and type 2 DM death rates and DALYs affect more Vietnamese people each year. Moreover, since 2010, female deaths and DALY rates related to type 2 DM are increasing at a much higher pace. The decrease in the number of ENs, as well as the increase in health insurance expenditures per inpatient, seems to be, with the highest degree of certainty, correlated with HT and type 2 DM death and DALY rates.
LIST OF ABBREVIATIONS
| CVDs | = Cardiovascular diseases |
| DALYs | = Disability-adjusted life years |
| DM | = Diabetes mellitus |
| EN | = Elementary nurse |
| GBD | = Global Burden Disease |
| HIEpI | = Health insurance expenditures per inpatient |
| HT | = Hypertension |
| MCs | = Medical consultations |
| MD | = Medical doctor |
| NCDs | = Non-communicable diseases |
| SBP | = Systolic blood pressure |
| SEA | = Southeast Asia |
| SHW | = Skilled health workers |
| SR | = Vietnam Socialist Republic of Vietnam |
| SUNI-SEA | = Scaling-up NCD Interventions in South-East Asia |
| VHSY | = Vietnamese Health Statistics Yearbooks |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Because of the ecological character of the study employing aggregated data from routine statistics, no ethical approval nor consent to participate was needed.
HUMAN AND ANIMAL RIGHTS
This research was not conducted on human subjects and no animals were used in this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the (GHELI repository) at (https://repository.gheli.harvard. edu/repository/11444/), reference number [15]” and in the (Health-Statistical-Yearbooks-2009-2016) at (https://github. com/PatrikSivco/Vietnam-Health-Statistical-Yearbooks-2009- 2016.git), reference number [13]”.
FUNDING
This study was funded by European Commission (Horizon 2020) Funder ID: FundRef DOI: 10.13039/100010661 Awards/Grant number: 825026.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The research leading to these results was done within the framework of the SUNI-SEA project (https://www.suni-sea. org/) coordinated by Academisch Ziekenhuis Groningen (UMCG).


